The DCCT/EDIC (Diabetes Control and Complications Trial/Epidemiology of Diabetes Intervention and Complications) study showed that early intensification of glycaemic control in people with type 1 diabetes has a beneficial legacy effect of up to 30 years, reducing the risk of cardiovascular events by 30% (Nathan et al, 2014). Structured diabetes education is key to achieving this early glycaemic control; however, current programmes, such as Dose Adjustment for Normal Eating (DAFNE), are aimed at people with established diabetes and, to the authors’ knowledge, no programme exists for those newly diagnosed with type 1 diabetes.
In 2015, the HbA1c levels of people with type 1 diabetes in Scotland were significantly higher than in the other home nations, and developing models of care to improve this was a priority for the Scottish Diabetes Education Advisory Group. The HbA1c results in NHS Forth Valley were among the worst in Scotland (Diabetes in Scotland, 2015). As a result, we secured funding for 30 hours per month for 3 years from the Scottish Diabetes Education Advisory Group to find out how type 1 diabetes education was being delivered in Scotland at diagnosis and, based on this, create a structured education programme for people with newly diagnosed type 1 diabetes.
State of diabetes education in 2015
We contacted teams across Scotland to find out how education was delivered at diagnosis. We contacted each Health Board in Scotland via the National Managed Clinical Networks. We had a 100% response rate.
Each team in Scotland was delivering similar education; however, contacts were variable in terms of duration, target blood glucose levels and content of education. Most areas used a checklist, with no structured lesson plan, learning outcomes or feedback. Carbohydrate counting was taught but this could be up to one year after diagnosis. People were squeezed into appointments, which meant they were told what to do rather than taught self-management. Some areas were offering DAFNE or equivalent courses, but this could be several months or years after diagnosis. In most areas, HbA1c results were significantly higher than the target 48–58 mmol/mol (6.5–7.5%) recommended in the SIGN 116 guideline (SIGN, 2010).
Using audit data, we were also able to contact people recently diagnosed with diabetes to ask them what they would like if we were to develop a new education programme. Consistency of message (not specifically the person delivering the education) and time off work to help them adjust to their diagnosis were the most common requests.
Aim of the STEP programme
The aim of the resulting Scottish Type 1 Education Programme (STEP) is to provide people with newly diagnosed type 1 diabetes with the understanding and confidence to carbohydrate count and independently adjust their insulin dose. Its methodology can be summarised by the Chinese proverb: “Tell me and I will forget, show me and I will remember, involve me and I will understand”.
The Government’s 2011 Skills for Life survey showed that one in seven adults in England have literacy levels at or below Entry Level 3, equivalent to the literacy skills expected of a 9–11-year-old (Department for Business, Innovation and Skills, 2012), and this was considered when writing STEP. Our education programme uses an approach that treats the person as an individual, is respectful of their health beliefs, and is supportive, consistent and non-judgmental.
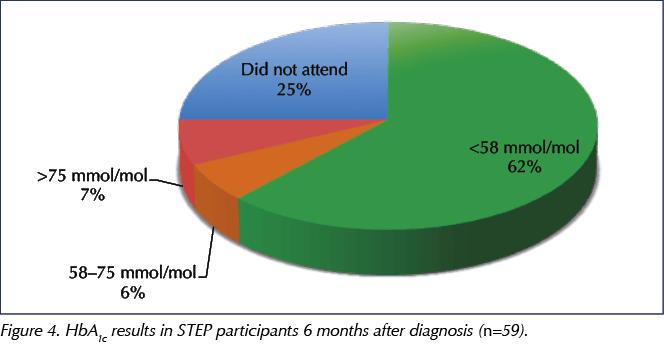
In Scotland, a national campaign to highlight glycaemic targets at diagnosis, Know The Numbers (Figure 1), had recently been launched, and we were all happy to recommend these targets within the STEP programme.
STEP uses a blended learning approach (Thorne, 2003), which combines written, verbal and online resources, giving the person with type 1 diabetes different opportunities to learn in the ways most appropriate to them. Unlike traditional approaches, our goal was to empower people with diabetes to take control, think critically and make autonomous, informed decisions (Anderson and Funnell, 2010).
STEP will be reviewed every 3 years and changes made if required.
Programme practicalities
Planning is paramount. We use Diabetes UK’s Everyday Life with Type 1 Diabetes (available at: www.diabetes.org.uk/Professionals/Resources) and JDRF’s Toolkit for adults with type 1 diabetes (available at: https://bit.ly/2EkDcGs) for written information. URLs for the two charities are provided, and patients are registered with the My Diabetes My Way website (available at: www.mydiabetesmyway.scot.nhs.uk) so that they can access all their own diabetes health records, including clinic letters and education modules.
As a team, we discussed how best to prioritise education for those newly diagnosed with type 1 diabetes. Appointments are 1 hour long and take place in the first hour of a clinic. The number of people diagnosed is fairly predictable, but when they are diagnosed is not. We continue to fit in the first session flexibly, but all other sessions are preset (both days and time) for the year, and the dates are given on the day of diagnosis.
Packs are prepared in advance to be given on the day of diagnosis (Figure 2). This reduces workload, promotes better time management for staff and allows protected time for those newly diagnosed with diabetes to ask questions and reflect on their decisions.
Prior to launching STEP, we were concerned that the programme would provide too much information too soon, that people would not take time off work, and that we would be unable to fit the education sessions into our current workload. However, we all wanted to see improvement, so in March 2016 we started to deliver the programme.
Delivering STEP
To deliver STEP, the healthcare professional has to be a trained educator according to the Assessment of Patient Education in Diabetes in Scotland process, and to complete regular peer review and self-reflection. The programme is delivered in our outpatients department.
Education starts on the day of diagnosis, and appointments are given for the next nine sessions. The lessons can be delivered one-to-one or as part of a group with others who are diagnosed that week. On the day of diagnosis, a Statement of Fitness to Work certificate is given to allow 2 weeks off work. Contact from a consultant on day one highlights the importance of the diagnosis and the need to attend the education sessions.
STEP uses lesson plans and learning outcomes, and is delivered by the team, including diabetes specialist nurses (DSNs), consultants, dietitians and psychologists. The DSN who sees the individual on the day of diagnosis becomes their named nurse, whom they can contact between appointments if required.
There are 10 lesson plans to be used within four months of diagnosis (Box 1). Six of these contacts are within the first two weeks, when carbohydrate counting is taught. At each appointment there is an opportunity to ask questions, and before new information is taught time is spent recapping the information given at the previous appointment.
Starting doses of insulin
The NICE NG17 guideline (NICE, 2015) recommends a basal–bolus regimen comprising twice-daily insulin detemir and a rapid-acting insulin before meals (we use insulin aspart). We originally calculated the starting dose based on weight at diagnosis and blood ketone levels, suggesting a one-third basal, two-thirds bolus split. However, after 6 months, we realised that 0.4 units/kg was not enough and now use 0.6 units/kg if blood ketone levels are <2 mmol/L and 0.8 units/kg if ketones are >2 mmol/L.
Programme of care
The person with diabetes is given all the resources that will be used throughout STEP on day 1, and a copy of what to expect at each appointment. They are encouraged to upload to Diasend at home and to reflect on their results. Meters are uploaded in clinic so that results can be discussed and insulin changes made if required.
Each quarter, all those diagnosed with type 1 diabetes during that period meet in a full-day group session. The morning session is facilitated by a clinical psychologist and the afternoon session is facilitated by a consultant. As shown by Simmons et al (2013), peer support has proven to be invaluable.
Audit results
We have been delivering STEP for almost three years and have made some changes along the way based on feedback from participants and staff. At week 5 of the programme and after 4 months we measure participants’ confidence to manage their diabetes and to make changes by themselves. We also ask for feedback about programme content, appointment times, and whether time off work was useful. We have made changes to the programme based on this feedback; as mentioned previously, the dose of insulin at diagnosis has increased, and we now discuss the effect of prolonged exercise on blood glucose levels. We have also changed the timing of when we give advice about ordering repeat prescriptions, and the consultant- and psychology-led group sessions are now held on the same day, which has improved attendance. In addition, clinical outcomes are audited using SCI-Diabetes, a shared national electronic diabetes record.
The following results are based on our experience with 69 participants and 15 staff. Those with latent autoimmune diabetes in adulthood or pancreatic insufficiency have also participated but have not been included in the results.
Participant feedback
Participants completed a questionnaire (Box 2) at the eighth visit (within 4 months of diagnosis) to provide feedback on the programme and to assess their confidence to self-manage their diabetes and make changes to their insulin dose independently.
A score of ≥7 out of 10 is deemed an acceptable indicator of confidence (Koenigsberg and Corliss, 2017). The feedback showed that 98% of participants felt confident to self-manage their diabetes and 91% were confident to independently adjust their insulin.
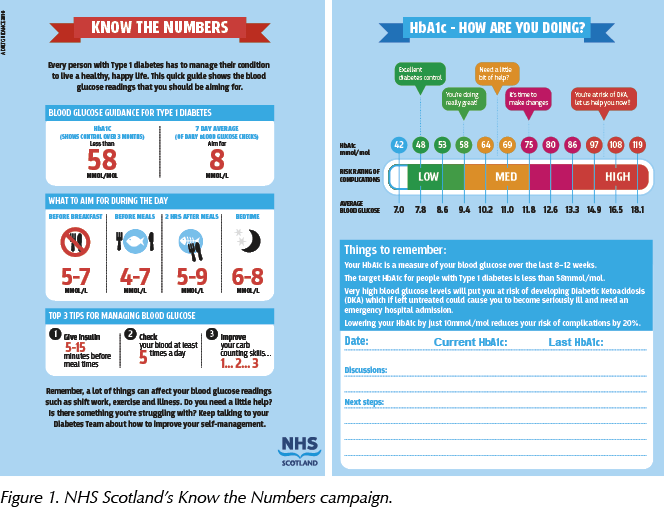
A word cloud of the most common comments in the feedback questionnaire (Figure 3) suggests that participants were very happy with the programme.
Clinical outcomes
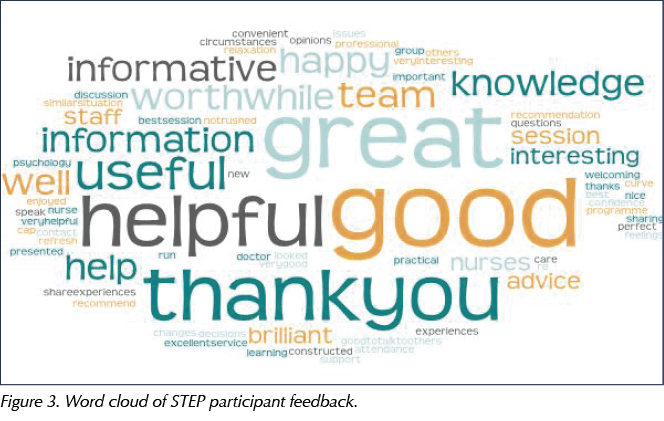
Figure 4 shows the proportion of STEP participants achieving HbA1c targets 6 months after diagnosis (results from 59 participants attending STEP between 2016 and 2018). Overall, 62% achieved an HbA1c of <58 mmol/mol (7.5%).
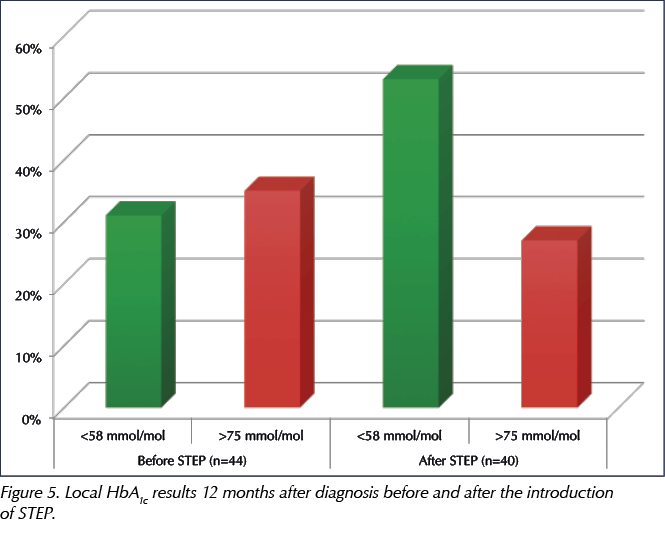
Using data from the SCI-Diabetes register, Figure 5 compares the proportion of people with newly diagnosed type 1 diabetes achieving HbA1c targets before the introduction of STEP in 2014–2015 (n=44) and, after the introduction of STEP, in 2016–2017 (n=40). The results show an increase in those achieving an HbA1c of <58 mmol/mol (7.5%) and a reduction in those with an HbA1c >75 mmol/mol (9.0%).
Final comments
As a team, we are delighted to see improved understanding and confidence in our patients, which promotes independence with insulin adjustment and carbohydrate counting. This has resulted in a significant improvement in HbA1c results. Seeing people with diabetes who are confident in self-management and have improved HbA1c has also led to an increase in job satisfaction and boosted team morale.
There are 14 Health Boards in Scotland. Of these, the Highland, Borders, Lothian, Shetland and Grampian Boards are now using STEP, and the Glasgow and Ayrshire & Arran Boards have also expressed interest. STEP has also been used as the basis for a national diagnostic pathway and timeline, currently in development, for people newly diagnosed with type 1 diabetes.








NHS type 2 diabetes prevention initiative reaches more people than ever.
5 Jun 2025