Self-care practices are essential in the management of diabetes and its complications but are affected by many factors, such as a person’s belief in their ability to perform them (ElSayed et al, 2023). This perceived self-efficacy (SE) affects a person’s capacity to perform healthy behaviours, so it is a critical determinant for a person’s well-being; it reflects their ability to commit and adhere to self-care activities that affect clinical outcomes (Adam and Folds, 2014; Walker et al, 2014). High levels of SE engender a sense of responsibility and a feeling of freedom in performing self-care activities (D’Souza et al, 2017).
From this perspective, it was important to study SE, and its underlying sub-scales, to determine the needs of people with diabetes. Few studies have examined the level of SE among people with diabetes and, in a literature review, no studies were found to have assessed SE by its specific sub-scales among people with type 1 diabetes.
Aims
This study aimed to investigate the level, specific sub-scales and correlates of self-efficacy among Jordanian people with type 1 diabetes. Specifically, it sought to answer the following:
- What is the level of SE among people with type 1 diabetes in Jordan?
- Which of the SE sub-scales are they most confident and least confident to perform?
- Based on demographic categories, what are the differences in SE among people with type 1 diabetes in Jordan?
Method
Design and settings
This study was a part of a larger research project. A descriptive, cross-sectional and quantitative design was used, utilising a self-report, online questionnaire on Google Forms. The sample was recruited from outpatient clinics at two large governmental hospitals in Jordan’s two largest cities – Amman and Irbid.
Sampling
A non-probability, convenience sample was used to recruit participants aged 18–30 years with a diagnosis of type 1 diabetes for over six months, and who were able to use a smartphone or computer to complete the online questionnaire. Anyone who was critically ill or had any mental or physical disabilities was excluded from the study.
Instruments
The data was collected using a self-administered questionnaire composed of a demographic data sheet and the Arabic version of the Diabetes Self-Efficacy Scale (DSES). The DSES is composed of 60 items that measure patients’ confidence levels in performing specific activities and behaviours, and managing their disease.
These items were categorised into seven subscales: 15 on eating healthy foods; 6 items on activity; 7 on blood glucose monitoring; 6 on adherence to medication; 7 on foot care; 4 on problem-solving; and 15 on reducing risks.
Participants responded to the DSES items on a six-point Likert scale from “Strongly disagree” (0) to “Strongly agree” (5). Total scores ranged from 0 to 300, with higher scores reflecting a greater SE. The DSES is a valid, reliable scale (Sousa et al, 2009); Cronbach’s alpha coefficient in the current study was 0.94.
Finally, a pilot study was conducted to assess the reliability and comprehensibility of this DSES version, and to highlight any technical problems that participants could faced relating to the online questionnaire.
Data collection
After obtaining ethical approvals, the principal investigator approached the nurse managers working in the diabetes clinics at the chosen hospitals, explained the study purpose and procedure, and obtained their permission to meet potential participants. They were then interviewed and, if they met the inclusion criteria, informed consent was obtained for their participation.
Subsequently, a link to the online questionnaire was sent to their phones, and they were asked to complete it while they waited to see the physician in the diabetes clinic. This took around 20 minutes, during which the investigator was available to answer any questions.
Data analysis
Data were analysed using SPSS (v.26). Descriptive statistics were used to describe the study sample and their responses to the questionnaire. The differences in participants’ scores based on their characteristics were assessed by conducting a series of t-tests and one-way ANOVA. Further, the Pearson coefficient was used to detect relationships between the participants’ characteristics and their SE scores.
Ethical considerations
Ethical approvals from the University of Jordan and the Ministry of Health were obtained before commencing the research. Also, this research was conducted under the principles of the Declaration of Helsinki.
Results
Sample characteristics
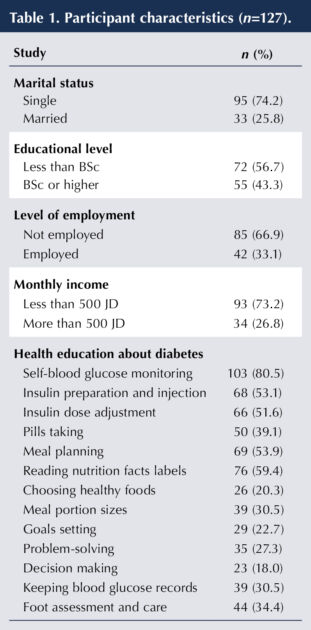
The total sample comprised 127 participants. Most were female (n=75; 58.6%) and single (n=95; 74.2%). Their mean age was 23.47±4.09 and their average weight was normal based on BMI (24.11±4.01). Only 39 (30.5%) declared being a smoker, and 75 participants (58.6%) had no other medical conditions. Most declared receiving diabetes education (n=117; 91.4%), with the most-reported topic on which education was received being “Self-blood glucose monitoring” (n=103; 80.5%; Table 1).
Diabetes self-efficacy
Participants’ total DSES mean score (M) was 215.46 (SD, 34.98; range, 97–299). Responses to the DSES scale and subscales are summarised in Table 2. The greatest confidence participants had in managing their condition was in “Problem-solving” activities (M=4.35±0.76), followed by “Adherence to medication regimen” (M=4.12±0.80). Conversely, the lowest confidence was related to “Eating healthy foods” (M=3.08±0.77) and “Activity” (M=3.34±1.01).
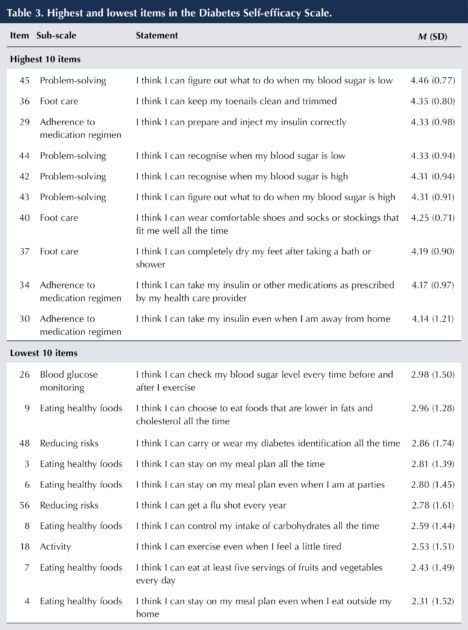
The participants’ responses to each item were calculated to detect items with high or low diabetes SE (Table 3). Generally, the highest items belonged to the “Problem-solving”, “Foot care” and “Adherence to medication regimen” subscales.
The highest mean was for item 45: “I think I can figure out what to do when my blood sugar is low” (M=4.46±0.77), followed by item 36: I think I can keep my toenails clean and trimmed (M=4.35±0.8). The lowest scores were for “Eating healthy foods” and “Activity”. The lowest means were for item 4: “I think I can stay on my meal plan even when I eat outside my home” (M=2.31±1.52) and item 7: “I think I can eat at least five servings of fruits and vegetables every day” (M=2.43±1.49).

Differences in self-efficacy levels in people with type 1 diabetes
The differences in scores based on the participants’ characteristics were assessed. Efficacy in “Eating healthy foods” significantly differed based on income (t(125)=2.01; P=.046). Those with a monthly income of less than 500 Jordanian Dinar exhibited higher efficacy (M=47.51±11.31) than those with higher income (M=42.91±11.72). Participants’ efficacy in “Physical activity” significantly differed based on their gender (t(125)=2.66; P=.004), with males exhibiting higher efficacy in “Activity” (M=21.73±5.25) than females (M=18.87±6.42). The rest of the demographics (marital level, education level and employment) did not reveal significant differences.
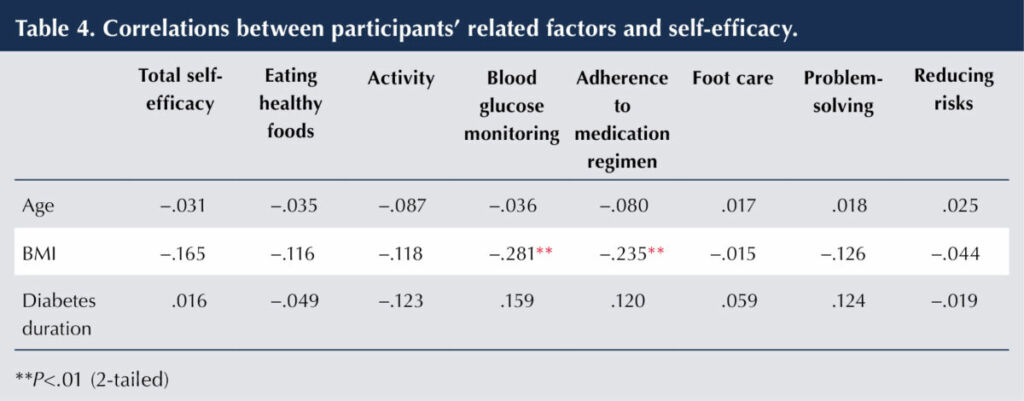
The Pearson correlation coefficient was used to test associations between age, BMI, diabetes duration and SE total scores and each subscale (Table 4). There were no significant relationships between age or diabetes duration with SE scores. However, there was a significant negative relationship between BMI and efficacy in “Blood glucose monitoring” (r=−.28; P=.001) and efficacy in “Adherence to medication regimen” (r=−.23; P=.008). This suggests that those with a higher BMI exhibit lower confidence in monitoring their blood glucose levels and adhering to their medication regimen.
Discussion
The purpose of this study was to evaluate the level and determinants of self-efficacy among Jordanian adults with type 1 diabetes, which is essential for the effective self-care management that is considered a cornerstone of diabetes care. Participants reported a relatively high level of SE (215 out of 300; 71.7%). Compared to people with type 2 diabetes, this is higher than the 52.5% and 60.6% reported by Oluma et al (2020) and Calli and Kartal (2021), respectively, but lower than the 91.14% and 73.8% reported by Şahin et al (2021) and Rashid et al (2018). A Brazilian study found that all 35 participants with type 1 diabetes reported medium to high levels of SE in diabetes management (Nass et al, 2019).
Self-efficacy is one of the most important factors affecting quality of life in people with diabetes. Higher SE leads to better adherence to various self-care behaviours, better glycaemic control and fewer complications (Tharek et al, 2018; Abdelghaffar et al, 2020). It has been reported that people with higher SE have lower levels of diabetes-related distress (Abdelghaffar et al, 2020) and that SE is the strongest predictor of well-being among people with type 2 diabetes (Calli et al, 2021).
Self-efficacy can be improved through an increased knowledge of diabetes management via education programmes (Walker et al, 2014). In an Iranian quasi-study of 76 adolescent girls with type 1 diabetes, those in the intervention group received texts or video educational messages. Results indicated a significant increase in SE in this group compared to the control group, particularly in the diet control, blood glucose control and medical care domains (Chopoghlo et al, 2021).
In the current study, confidence in diabetes management was highest in problem-solving, followed by adherence to medications. In contrast, the lowest confidence was in eating healthy foods and activity. This is partly consistent with Amer et al (2018), who found that 392 patients with type 2 diabetes were more confident in managing medications, followed by nutrition then physical exercise. Also, Rashid et al (2018) reported that 329 participants with type 2 diabetes had higher SE levels in managing medications, followed by blood glucose monitoring, physical exercise and then an eating plan. Furthermore, a Saudi study of 75 people with type 2 diabetes reported higher levels of SE in managing medications, followed by foot care and blood glucose monitoring. In contrast, SE in managing diet and exercise was found to be the lowest (Alaboudi et al, 2016).
Item analysis of the SE scale in our study revealed that the highest reported SE levels related to problem-solving, medication adherence and foot care. This was consistent with reported levels of SE in managing medications (Amer et al, 2018; Rashid et al, 2018) and foot care (Alaboudi et al, 2016). One possible reason for high level of SE in foot care is that Muslim participants have to perform ablution each time they pray, which may be many times daily. This includes washing their feet, which also provides opportunities to check them. The lowest reported SE levels were items related to eating. This is consistent with former studies that reported the lowest levels of SE in managing eating and exercise (Alaboudi et al, 2016; Rashid et al, 2018).
Self-efficacy has been linked with a better attitude toward self-care management and, consequently, improved adherence to these behaviours (Karimy et al, 2018). It has been found correlate with various self-care management behaviours, including controlling and testing blood glucose, medication adherence, diet, exercise and foot care. Those with higher SE levels adhere more to these behaviours (Alaboudi et al, 2016; Saad et al, 2018). For example, those with higher SE in blood glucose monitoring were found to have better glycaemic control.
The current study indicates that patients with less income reported higher levels of SE in eating healthy foods. Those with a lower income are used to living in specific circumstances and have adjusted their needs based on limited resources, perhaps resulting in more confidence managing their condition. Nass et al (2019) found that in a cohort of young people with type 1 diabetes, those who were unemployed showed slightly higher levels of SE.
Based on a literature search, no studies reported relationships between specific sub-scales of SE with any of the demographic characteristics. However, our findings revealed that males reported higher levels of SE in physical activity than females. This could be attributed to fewer perceived barriers to exercise for males than females, such as places to exercise (Shajrawi et al, 2021). In Jordan, females need closed areas to exercise. However, Almutary and Tayyib (2020) found that educational level was the main factor correlating with exercise SE. As self-efficacy affects adherence to and the performing of self-care activities, those with higher levels of SE exercise more than those with lower levels (Oluma et al, 2020; Şahin et al, 2021).
Our results reveal that those with higher BMI reported lower levels of SE in blood glucose monitoring and adherence to medication. This is consistent with Malaysian and Turkish studies of people with type 2 diabetes (Tharek et al, 2018; Şahin et al, 2021), but contradicts the study by Nass et al (2019), in which it was not significant.
There was a significant relationship between BMI and the level of SE. This can be interpreted as increasing BMI negatively affecting a person’s self-image, their feelings of control, self-confidence and their belief in their capabilities to perform self-care behaviours, leading to decreased motivation, commitment and adherence to their self-care behaviours, and thus poor management of diabetes and increased complications. Interventions aimed at improving SE could, therefore, enhance a person’s confidence in their abilities, improve adherence and commitment to perform self-care behaviours, and achieve better outcomes, including lowering BMI.
Limitations and recommendations
This study’s limitations include the convenience sampling of participants and their limited age range (18–30 years), which affects the generalisability of the results. However, it was the most suitable method to recruit a sample with specific characteristics.
Also, using a self-report questionnaire affects the validity and accuracy of the information provided. However, it was the best data collection method for a geographically dispersed population. It is also possible that, because of the questionnaire’s length, participants lost focus while completing it, and subsequently provided inaccurate data.
Improving SE among people with diabetes is based on improving their knowledge and experience in performing self-care behaviours, particularly those that they have low confidence in. This could be achieved by planning educational programmes based on patients’ needs that could be implemented in various user-friendly and easily accessible formats, such as mobile phone apps and websites. Also, it is recommended that exercise programmes provide settings and times that females feel comfortable with.
Conclusion
This study highlights the importance of SE among people with type 1 diabetes. Participants had relatively high levels of SE, but not in all sub-scales. Confidence in identifying and managing any alteration in blood glucose level, adherence to insulin and foot care were reported the highest, while eating healthy foods and exercising were the lowest. Efforts should be focused on people’s needs to improve their SE in needed areas. Self-efficacy varies according to many factors that should be taken into consideration. Self-efficacy is one of the most critical factors affecting self-care management of diabetes. Those who showed higher levels of SE reported better adherence to self-care activities, resulting in better glycaemic control, fewer diabetic complications and, subsequently, better quality of life.





Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025