In West Dorset, at the time of this project, services had one sixth of the recommended number of DSDs for the population and so were unable to meet local needs. This pilot project, conducted between September 2017 and September 2018, aimed to determine whether changing access to and the format of DSD-led primary care services would increase service uptake without the need for additional staffing.
Methods
Context
The project was undertaken within the Health Education England Wessex School of Quality Improvement Fellowship. A qualified DSD led and conducted the study, and so the pilot was undertaken in one GP surgery to create a manageable workload. The problem of limited DSD access was explained to those surgeries that used the existing DSD services, and a volunteer surgery was requested to help develop and pilot a new service model. One surgery volunteered and so became the pilot surgery.
Prior to the project, existing practice was that the surgery could refer to a structured education course for people newly diagnosed with type 2 diabetes. After that initial course, individuals could be referred by a healthcare professional to the community hospital DSD clinic for a one-to-one appointment if certain criteria were met; these criteria limited the people who could access the DSD to those who had already developed diabetes-related physical health complications or were exhibiting risk factors, such as high HbA1c (Figure 1).
Of the 544 people registered at the surgery who had a diagnosis of type 2 diabetes for more than 1 year, and who therefore may have benefitted from regular dietary updates, only ten had seen the DSD in clinic in the previous year.
Ethical approval was not necessary for this project as clinical provision within the pilot was equivalent to the previous service and within the bounds of usual DSD care. The pilot did not restrict service access for any people (the existing clinic and referral route remained available for those who met pilot exclusion criteria). Attendees were informed at invitation and in the session that the service was a pilot and gave written consent for their data to be used.
New service design
After discussions with practice nurses, service users and the DSD providing the existing clinic, structured group education, to be delivered in the surgery, was identified by the project lead as the most impactful service improvement, in order to provide dietary updates to people with type 2 diabetes. A single group session could accommodate ten people in 2 hours, compared with four people per clinic in the existing service, which allocated 30 minutes per patient. Patients’ input was sought via the pilot surgery’s Patient Participation Group, and this helped to name the sessions “Taking Control of Diabetes”.
Referral pathways were discussed by the project lead with the practice nurse, practice information analyst and practice manager. From this discussion came one of the key differences to the service: attendees would not be referred by a healthcare professional. All patients would be contacted directly, enabling them to self-select whether to access the service, no longer limiting access to those who had or were at high risk of complications and no longer requiring GPs or practice nurses to administer the referral (Figure 1).
Anticipated uptake was unknown, so three sessions catering for ten people each were scheduled, providing triple the capacity of the previous year’s DSD service use.
New service pilot
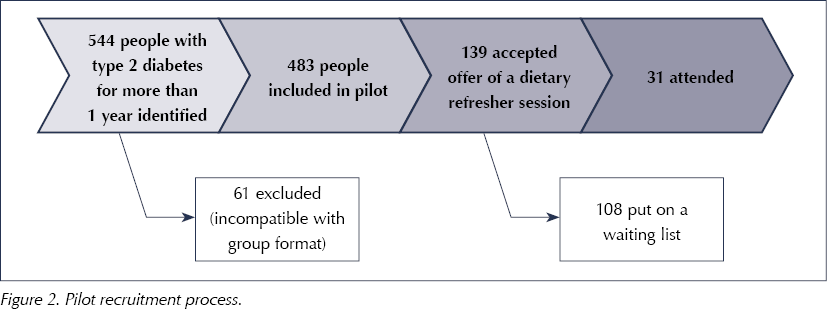
Of the 544 people within the surgery population who had type 2 diabetes for more than 1 year, 61 were excluded for reasons of incompatibility with the group education format: dementia, being housebound, a learning disability and not speaking English. After those exclusions, a cohort of 483 were identified for inclusion in the pilot.
An invitation letter, which had been co-designed with the surgery’s Patient Participation Group, was sent to each of the 483 individuals via the GP mailing system (to maintain data security), explaining the pilot and inviting them to one of three pre-planned session dates. Responses were collated by the diabetes service secretaries, and participants were booked onto the sessions on a first come, first served basis.
Measures
The primary measure of impact was the number of people who accepted the invitation. This number was taken to represent user demand for DSD services, for comparison with the demand that had been apparent in the previous year’s activity, resulting from the previous service format and referral pathway.
The secondary measures were changes in attendees’ knowledge and confidence. The balancing measure was attendee satisfaction with the new service. Information for these measures was assessed via feedback forms that were given out and collected at each session. Reflection by the experienced project lead DSD was also used to assess success of the session from the clinician perspective.
HbA1c and BMI levels were also assessed to determine whether or not those accessing the new service were the same cohort who would meet the referral criteria for the original DSD clinics.
Results
Uptake shows that more patients wanted DSD services than were able to access it via the existing GP/nurse referral route and criteria-restricted clinics, and that they would able to access them via the self-selection format. Overall, 139 (29%) of the 483 people who were invited took up the offer of a dietary refresher session, compared with ten who had accessed the DSD clinic in the preceding year. The pilot therefore indicates that direct, proactive contact to enable patient self-selection, combined with group education, is an effective method to increase access to dietary advice. Demand exceeded the 30-place capacity of the pilot and a waiting list was created (Figure 2).
Of the 139 people who wanted to attend, 14% had HbA1c and BMI values below the clinical criteria for referral to the DSD under the established service process, and so would not have been able to access that service.
Three sessions of Taking Control of Diabetes were delivered to a total of 31 people. In comparison, the previous service would have had capacity for 18 people (three clinics) using the same amount of DSD time. Whilst not all individuals’ needs will be met by group education, replacement of some clinics with group sessions offers a means to increase capacity without the need for additional DSD staffing.
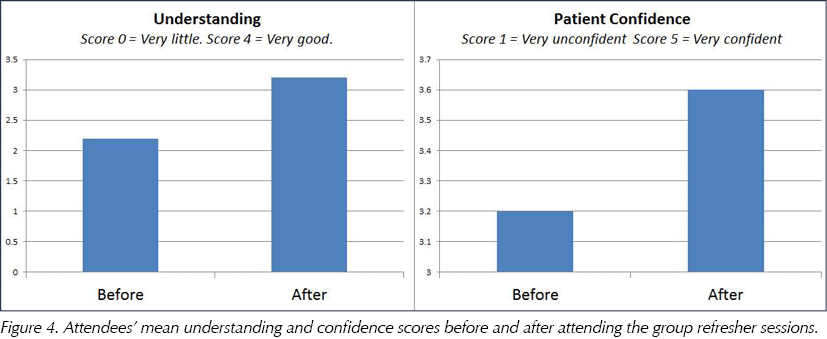
Feedback was sought using Likert scales and space for free-text comments. Using the standard NHS Friends and Family Test, 30 attendees stated they would recommend the session to friends or family with diabetes, one gave a neutral response and none said they would not recommend the service. When asking whether the session helped participants to achieve what mattered to them or their goals, an average feedback score of 3.4 (on a scale of 0 [made it a lot harder] to 4 [helped a lot]) shows that the session was person-centred in addressing what mattered to the attendees (Figure 3). Understanding of diabetes was shown to increase after attending a session (Figure 4), as was confidence in self-management, which may be an indicator of positive impact on health outcomes (NHS England, 2019).
 |
 |
The groups contained a highly heterogeneous mix of participants (Table 1). The project lead reflected that the need to adapt the information to meet the differing needs of attendees within each group inhibited clarity of message and took up time. However, no other detrimental impact of delivering the session to a group of self-selected participants, compared with patients who had been referred, was identified.
Discussion
Group education is an established and impactful method of dietetic service provision (Lawal and Lawal, 2016), and this pilot showed that it increased capacity for type 2 diabetes services within the existing DSD staffing resource. If the service format were to be rolled out on a larger scale, the impact on administrative and informatics staffing would need to be considered to give an accurate cost analysis.
The increased number of people who opted to access the DSD service and the positive feedback showed that patient self-selection is an effective method to achieve increased uptake of dietary updates for people with type 2 diabetes.
The heterogeneity of the groups increased the complexity of service delivery for the DSD. A next step for this service improvement could be to run a further pilot in which participants are allocated to groups according to their medication type and/or to a group specifically for those with moderate or severe frailty. With more homogeneous groups it should be possible to increase group size, which would further improve DSD service efficiency.
Overall, 14% of those who took up the offer of the DSD service did not meet the criteria to access the previous service, as their health metrics did not show any problems with their diabetes. That these people wanted dietary updates indicates that the service can provide a role in preventing development of diabetes-related ill health in the future. Prevention is a key tenet of the NHS Long Term Plan (NHS England, 2019) and has the potential to reduce future service pressures. Longer-term assessment may be needed to demonstrate the impact that this DSD service had on preventing ill health.
While participant feedback was very positive, it must be considered that respondents had self-selected to attend, and therefore we should assume a preceding interest in the subject matter, and thus selection bias in the population who provided the feedback. It is important, however, to consider dietary knowledge in a broader context, as it alone is not sufficient to improve health outcomes: behaviour change is necessary. The transtheoretical model posits that health behaviour change involves progress through the cycle of change (Prochaska and Velicer, 1997). It could be presumed that self-selection enables people to access the service when they are ready to change, compared with the existing access route, which is likely to offer the service at a time when a healthcare professional thinks a change is needed. Targeting services in accordance with the individual’s readiness to change should improve outcomes (Norcross et al, 2011), and this may be worth further study. Patient confidence (activation) is also thought to be related to health outcomes (Greene and Hibbard, 2012), and the participant feedback supports that the DSD service increased confidence as well as knowledge.
This pilot required close working with the GP surgery and use of its administrative systems to maintain data security. This may not be feasible for a service covering multiple surgeries, and so consideration is needed regarding the administration if the service is to be rolled out on a wider scale.
Take-up was greater than anticipated, requiring a waiting list to be created. If the new service model is further developed or rolled out, the results of this pilot will provide a more accurate predictor of anticipated uptake.
Changing from a one-to-one clinic to a group format would not have been sufficient to accommodate 139 people if restricted to the DSD time previously allocated to provide for ten clinic appointments. As the service is not urgent, however, it would be possible to phase the invitations over time so that service demand becomes more manageable within existing resources.
Limitations
The pilot was carried out in one GP surgery with project lead DSD time funded by Health Education England Wessex. It did not take into account the following issues, which would need to be considered if the service were to be implemented at full scale: administrative support, patient data access and security.
Conclusion
This pilot service model, based on proactive invitation and patient self-selection and group education, has proven to be effective at increasing uptake of dietary education updates for people with type 2 diabetes without requirement for more DSD staffing. The increased efficiency of DSD time makes it a sustainable model; however, the capacity of support services needs to be considered. The model is replicable in other GP surgeries but consideration is needed regarding the limitations of running multiple surgery-specific services or whether a local Primary Care Network approach would increase efficiency and offer increased choice to service users. Further research is needed to assess the longer-term health implications. The next step is to consider roll-out of the service on a larger scale, with separate sessions for people on insulin, non-insulin diabetes medications and no diabetes medications. Expansion of the sessions to include practice nurses or DSNs should also be considered.
Funding acknowledgement
The DSD project time was funded by the Health Education England Wessex Quality Improvement Fellowship.







NHS type 2 diabetes prevention initiative reaches more people than ever.
5 Jun 2025