Results from the 2017 National Diabetes Inpatient Audit (NaDIA) confirm that 18% of hospital beds in England and Wales are occupied by people with diabetes (NHS Digital, 2017). With the prevalence of diabetes increasing year on year, acute hospitals will subsequently be treating significant numbers of inpatients with this condition.
Hypoglycaemia, defined as a blood glucose level below 4 mmol/L (Diabetes UK, 2018), with or without symptoms, is a frequent occurrence experienced by inpatients with diabetes. According to NaDIA, approximately one in five inpatients (18%) had a hypoglycaemic event during their hospital stay. Inpatient hypoglycaemia increases expenditure in the NHS, being a well-documented risk factor for adverse outcomes. It is associated with increased mortality and morbidity (Yeh et al, 2016), with hospital length of stay increased by a mean of 2.5 days for each day a patient experiences a hypoglycaemic event (Turchin et al, 2009).
Care bundles
The concept of care bundles was developed by the US Institute for Healthcare Improvement (Resar et al, 2012), and these have been extensively used in secondary care to improve patient outcomes since 2001. Care bundles are checklists based on accepted national guidance and reflect best practice. The goal of the bundle approach is to amalgamate a short list of recommended interventions and treatments that are generally accepted by local consensus as being applicable to the majority of the intended recipient population.
A plethora of literature exists on the use of care bundles; however, there is a dearth of evidence on their specific use in diabetes management. Rushmer and Voigt (2008) developed an evidence-based care cluster as part of a safer patient initiative to design a new insulin prescription chart. Maynard et al (2015) introduced a hypoglycaemia reduction bundle targeting the most common remediable contributors to iatrogenic hypoglycaemia, which improved event rates in non-critical-care patients. Care bundles are most effective when used with patients receiving particular treatments in defined patient populations. Therefore, they are ideally positioned to assist with the management of hypoglycaemic events in people with diabetes.
Background
The Royal Cornwall Hospital is an Acute Hospital Trust with approximately 743 beds and over 20 outpatient departments. The population with diabetes in Cornwall has now risen to approximately 32000, with an inpatient prevalence of 15.5% (NHS Digital, 2017). Cornwall Partnership NHS Foundation Trust provides inreach diabetes inpatient services to the Acute Trust.
Previous successful hypoglycaemia educational initiatives and innovative point-of-care simulation training established at our hospital has significantly improved staff knowledge of hypoglycaemic events and patient outcomes (Sleeman et al, 2018). As an adjunct to these improvements to our inpatient diabetes care, and to enhance care further, a hypoglycaemia care bundle label was explored and subsequently advocated.
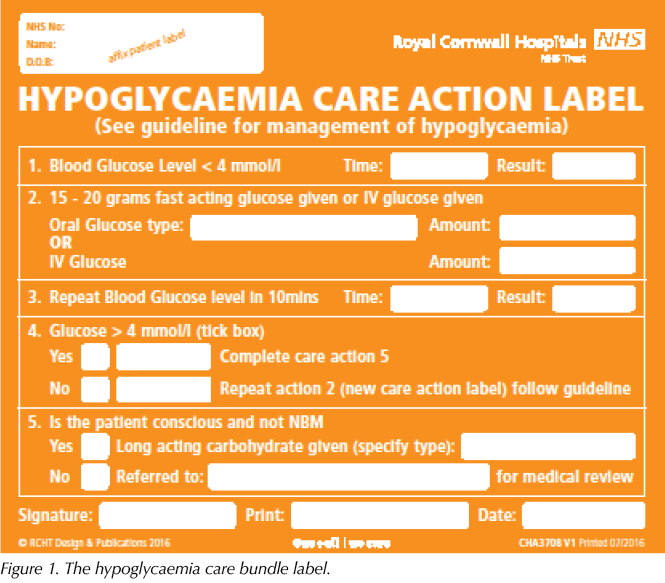
The diabetes inpatient specialist nurse (DISN) team devised the hypoglycaemia care bundle label (Figure 1). It is a succinct version of the hospital’s local hypoglycaemia guideline algorithm (Appendix 1), which is based on guidance by the Joint British Diabetes Societies for Inpatient Care Group (2018). The bundle label is intended to be placed into the nursing notes. It aids comprehensive documentation of hypoglycaemia whilst serving as an aide mémoire to prompt staff to correctly treat and manage hypoglycaemic events according to the Trust’s guideline.
The documentation, treatment and management of hypoglycaemia are audited each year via NaDIA. Use of the care bundle label assists with collation of data for the annual audit, making the process timelier, with the additional intention of improving the hospital’s NaDIA hypoglycaemia results and patient outcomes.
Care bundle label pilot
The Cardiac Investigation Unit (CIU) was designated as the pilot ward. The CIU has a recognised cohort of inpatients with diabetes owing to its cardiac specialism and the increased risk of cardiovascular disease in people with type 2 diabetes. Additionally, the CIU had successfully participated in a previous educational intervention in 2015–16, which reviewed nursing practice surrounding the identification and treatment of hypoglycaemic events.
All stakeholders were engaged, with agreement reached to trial for a 3-month period initially, with an option to extend to 6 months if required. The DISN team reviewed their working day and made adaptions to enable them to undertake the pilot without additional funding for the agreed period.
Pilot aims and objectives
The aims were as follows:
1. Improve documentation of hypoglycaemic events.
2. Raise awareness of correct hypoglycaemia treatment.
3. Increase compliance with the Trust’s hypoglycaemia guideline algorithm.
The objectives were:
1. Contemporaneous documentation of hypoglycaemic events.
2. Improved patient outcomes post-hypoglycaemia.
Pilot expectations
- Any hypoglycaemic event, defined as a blood glucose level <4 mmol/L, would be treated according to the Trust’s hypoglycaemia guideline algorithm.
- The hypoglycaemia care bundle label would be placed into the current section of the nursing documentation and fully completed for each hypoglycaemic event by the nursing staff.
- DISNs would review the patients’ diabetes management and the nursing documentation for compliance for all hypoglycaemic events that occurred Monday to Friday.
- Any hypoglycaemic event without a hypoglycaemia care bundle label in the nursing documentation would have an incident (Datix) form completed.
– The Datix would be completed by the DISN team that identified the non-compliance. - DISNs would report monthly to the matron and ward sister/deputies.
Pilot process
- The DISN project/pilot lead met with the clinical matron and ward sister, and devised an information flyer advertising the pilot and its expectations.
- The ward sister and deputies shared the flyer with the staff for one month prior to the start of the pilot.
- The start date was agreed with the DISN team, ward sister and clinical matron.
– The nursing team used the hypoglycaemia care bundle labels and placed them in the nursing notes for all hypoglycaemic events from the pilot start date. - The DISN team accessed Bio Viewer, a web-based storage centre for all blood glucose results recorded using the Trust’s connective glucose meters, Monday to Friday.
- The DISNs generated a hypoglycaemia report for the CIU of all patients with blood glucose results <4 mmol/L over the previous 24 hours.
- The DISNs visited the ward Monday to Friday to clinically review the patients and provide a management plan of care.
– Any changes to clinical management were communicated to the ward staff and doctor team, and were documented in the patients’ medical notes. - The DISNs reviewed whether the hypoglycaemia care bundle label had been completed correctly and the hypoglycaemia was managed correctly.
- Any non-compliance with the Trust’s hypoglycaemia guideline algorithm, management issues or incomplete filling-in of the care bundle label was reported via Datix.
- Monthly summary reports were compiled by the DISN project/pilot lead and sent to the ward sister, deputies and clinical matron.
- Learning was shared with the ward team.
Results
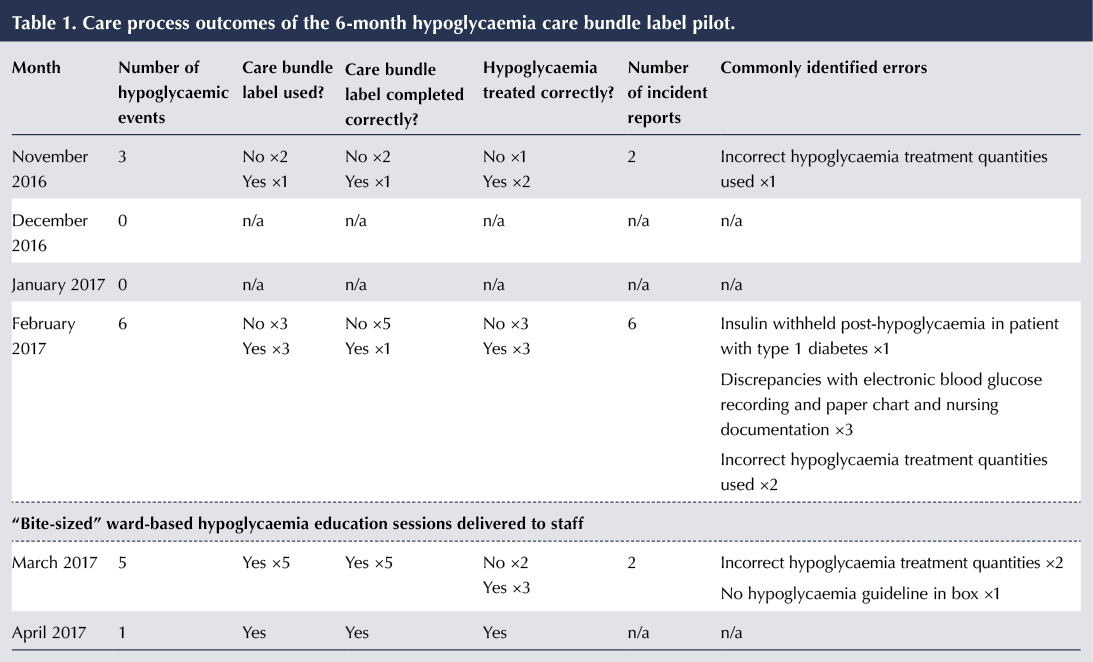
The pilot was initially planned to run for a period of 3 months. It was subsequently extended to 6 months due to low numbers of hypoglycaemic events, in order to gain meaningful data and outcomes. A total of 15 hypoglycaemic events were identified in this 6-month period. The main outcomes are summarised in Table 1.
Commonly identified errors
- Incorrect hypoglycaemia treatment quantities were used.
- Nursing documentation surrounding hypoglycaemic events was not well recorded.
- The hypoglycaemia care bundle label was not fully completed.
- Discrepancies between electronic blood glucose results and paper chart recordings.
- Management errors (e.g. insulin withheld post-hypoglycaemia).
An additional educational intervention was initiated in month four. This was requested by the ward sister due to the number of Datix reports for inappropriate hypoglycaemia management. The education consisted of a DISN visit to the CIU at morning handover to provide “bite-sized” education for half an hour over a one-week period. The aim of the sessions was to improve compliance with use of the hypoglycaemia care bundle label and to increase staff knowledge on hypoglycaemia management. Correct use of the care bundle label and the Trust’s hypoglycaemia guideline algorithm was reinforced, along with general diabetes Q&A sessions. This involved the majority of the ward staff, and a register of attendance was kept for compliance with governance.
This proved to be a successful intervention. As a direct result of the education, hypoglycaemia management outcomes improved. This was demonstrated via improved compliance with use of the care bundle label and an increase in the correct treatment and management of hypoglycaemia events. Additionally, positive changes to practice were made at ward level.
Specific pilot outcomes/improvements
- Increased staff engagement – staff were enthusiastic about delivering correct hypoglycaemia treatment and improving diabetes care in their area.
- The DISN bite-sized education was well received, with positive verbal feedback given.
- An out-of-date hypoglycaemia guideline which was still in use, rather than the Trust’s current one, was replaced.
- Out-of-date blood glucose monitoring charts were still in use. These charts did not have the hypoglycaemia treatment synopsis or the extra blood glucose monitoring section on them to aid treatment and management of hypoglycaemic events. Old stock was removed and the Trust’s current glucose monitoring chart was obtained and stocked.
- Orange juice cartons have been placed in the medicines fridge and labelled for hypoglycaemia treatment. This will aid access to prompt, correct treatment choice and quantity.
- Via general Q&A at the bite-sized education sessions, the types of diabetes and their importance for treatment decisions in practice were discussed. Via a change to practice, the patient’s type of diabetes will now be identified at morning handover to aid diabetes management.
- Via the general Q&A at the bite-sized educational sessions, staff knowledge in other areas of diabetes management was updated (e.g. correct use of as-needed insulin and pre-investigation advice).
Limitations of the pilot
The initial pilot did not have additional funding attached for DISN or administrative time. However, due to the low number of hypoglycaemic events identified during the pilot, the following limitations were manageable:
- DISN time to generate reports and undertake ward patient reviews – this was additional clinical activity.
- DISN time for the bite-sized educational intervention – this was additional unplanned educational activity.
- Completion of Datix – this was a resource issue as the DISNs do not have any administration support, so was additional non-funded activity.
Ongoing considerations
Summative evaluation of the project via an exit questionnaire to formally verify outcomes is required. In addition, considering staff turnover in ward areas, further bite-sized education for new staff members will be needed. This could be approached via a cascade system, with sessions delivered by existing ward staff members or the ward’s diabetes link nurse. A toolkit-type educational resource would need to be developed to enable this.
For the hypoglycaemia care bundle label to be piloted in other ward areas that have a higher proportion of inpatients with diabetes, or rolled out throughout the Trust, additional DISN funding would need to be agreed.
Considering this resource requirement and the successes of the initial pilot, Kernow Clinical Commissioning Group and our Lead DSN bid for extra funding via the NHS England Diabetes Transformation Fund (NHS England, 2017). The funding included an element for DISN teams specifically linked to patient safety quality outcomes. Our bid included using the hypoglycaemia care bundle label, along with reducing medication/insulin errors (identified from our NaDIA results) by 10%. The bid was successful and has subsequently increased our DISN whole time equivalent by 0.8 (30 hours) for a 12-month period.
The initial pilot has now evolved and has been renamed as “The Diabetes Improvement Project”, to include diabetes medication/insulin administration and prescribing errors along with the established hypoglycaemia care bundle initiative. Four medical areas with high rates of medication, insulin and prescribing management errors and hypoglycaemia events have now been identified to be implemented and continued for the next year. Our expectation is that we will meet the key performance indicators of the project.
Acknowledgments
The authors would like to thank Ian Moyle, Clinical Matron (Cardiology), and the Staff of the Cardiac Investigation Unit, Royal Cornwall Hospital NHS Trust.





Empowering nurses to tackle inequities in access to technology.
22 Jul 2025