Hypoglycaemia is described by the American Diabetes Association (2022) as any low blood glucose level that exposes the individual to harm, with a defined threshold plasma level of <3.9 mmol/L. Although most people with diabetes are admitted to hospital for reasons not directly related to their diabetes, adequate management of their diabetes whilst admitted, including timely recognition, treatment and prevention of hypoglycaemia, will help reduce morbidity and prevent lengthy inpatient stays (Joint British Diabetes Societies for Inpatient Care [JBDS-IP], 2022).
Nursing staff are at the forefront of health service delivery, forming the largest group of healthcare professionals, and they play a pivotal role in the prevention, early detection and treatment of hypoglycaemia in the hospital setting. Unfortunately, hypoglycaemia is not always treated successfully by nursing staff despite the availability of guidelines and protocols (Ndebu and Jones, 2018; JBDS-IP, 2022). Possession of sufficient knowledge of diabetes can positively influence nurses’ attitudes towards the management of this condition.
The aim of the present pilot study was to assess levels of knowledge regarding hypoglycaemia among ward-based nurses in a single hospital in County Cork, Republic of Ireland, and the impact of a bite-sized educational intervention on nurses’ knowledge of hypoglycaemia and its management.
Methods
A quasi-experimental, pre-test/post-test, quantitative approach with one group was deemed appropriate. The pilot study drew on the Knowledge, Attitudes, Practice – Outcomes (KAP-O) research framework (Wan et al, 2016).
Ethical approval was sought from the Clinical Research Ethics Committee of University College Cork Teaching Hospitals. The anonymity and confidentiality of the participants was ensured and maintained throughout the study.
Knowledge questionnaire
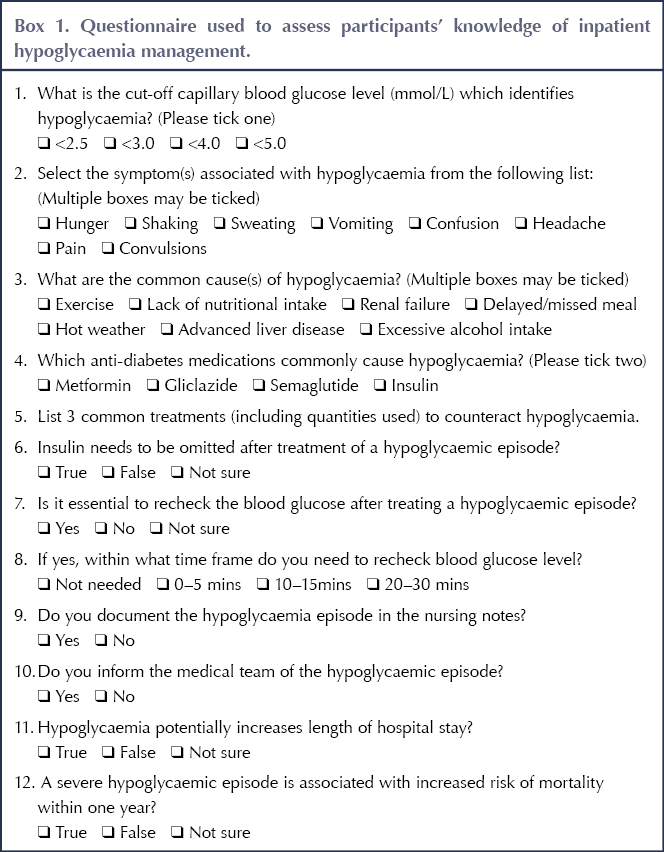
An anonymous questionnaire previously developed by Chinnasamy et al (2011) and later used by Ndebu and Jones (2018) was utilised with consent to assess the knowledge of ward nurses at Bantry General Hospital, County Cork. The questionnaire was adapted to suit the current healthcare system. The questions are detailed in Box 1.
Participants filled in the questionnaire before receiving the education package detailed below, and repeated it immediately after the intervention. They were also asked how many years of nursing experience they had; whether they had cared for a person with diabetes in the previous 3 months; whether they were aware of the hypoglycaemia policy at the hospital; and whether they had received hypoglycaemia training in the previous 5 years.
Educational package
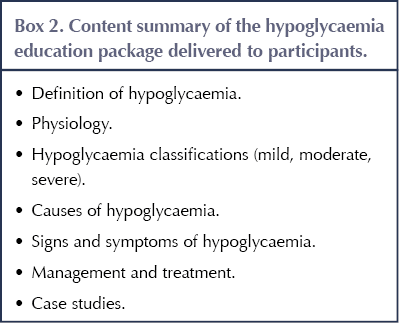
The Hypoglycaemia Knowledge and Management (H-KAM) intervention was delivered via Microsoft PowerPoint and consisted of an evidence-based, standardised education package on hypoglycaemia management and treatment, as per local, national and international guidelines and policies (NICE, 2015; SIGN, 2017; Department of Health Ireland, 2018). The content of the education package is summarised in Box 2. The full slides are available in Appendix 1.
The co-investigator delivered bite-sized education sessions from November 2020 to February 2021, inclusive. The H-KAM intervention was provided in the ward setting during nurses’ contracted work hours and lasted approximately 10 minutes.
Participants
A total of 77 participants out of an approximate 88 whole time equivalent nurses working on the medical ward, high dependency unit, rehabilitation/stroke unit and medical assessment unit in Bantry General Hospital took part in the pilot study. Bantry General Hospital is an acute, rural and remote hospital. The researchers utilised a non-probability convenience sample.
Statistical analysis
The data obtained from the questionnaire were analysed using descriptive and inferential statistics. Data were coded and entered into SPSS version 26 (IBM Corp, Armonk, NY, USA) for analysis.
Univariate analysis with McNemar’s test compared pre- and post-intervention knowledge scores. A paired t-test compared two sets of data from one group of people of a continuous dependent variable. A P-value of 0.05 was considered significant.
Results
The pre-test questionnaire mean knowledge score was 20.35 (SD 3.174), out of a maximum possible 33. The post-test mean knowledge score increased to 28.71 (SD 2.305).
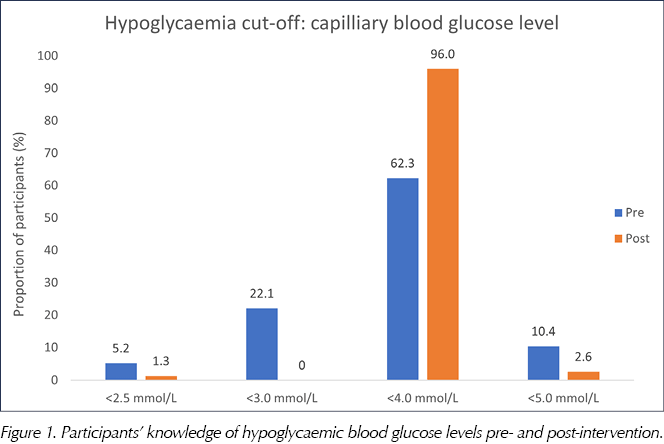
The proportion of participants who knew the correct capillary blood glucose level to identify hypoglycaemia increased from 62.3% to 96.0% post-intervention (P<0.001; Figure 1).
Furthermore, knowledge of the correct timing to re-check glucose levels improved. Pre-intervention, 65.8% of participants confirmed the correct time to re-check was 10–15 minutes after treatment. Post-intervention, this figure increased to 98.7% (P<0.001).
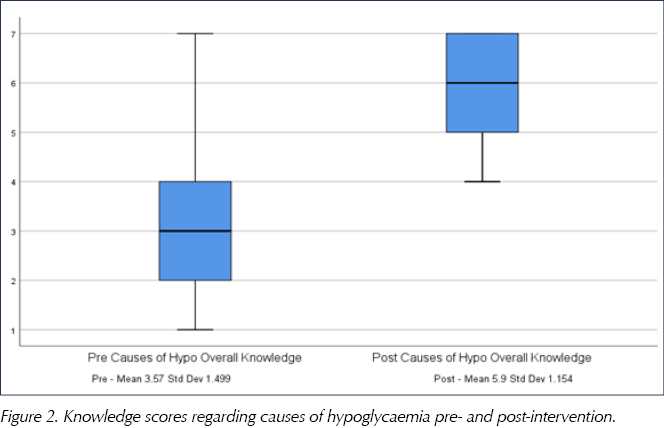
Nurses also had a significant increase in knowledge pertaining to potential causes of hypoglycaemia (P<0.012; Figure 2). The mean knowledge score regarding hypoglycaemia symptoms improved post-intervention; however, the change was not statistically significant.
Alarmingly, pre-intervention, only 31.2% of participants ascertained that gliclazide can cause hypoglycaemia (one of its main side effects). Post-intervention, 96.1% explicitly identified gliclazide as a risk factor for hypoglycaemia. Strangely, the proportion of participants who identified insulin as a risk factor for hypoglycaemia decreased (although not significantly) from 88.3% to 83.1% post-intervention.
One open-ended question required nurses to list three common treatments (including quantities) to counteract immediate mild hypoglycaemia. Pre-intervention, the mean score was 2.05 (SD 0.42) out of a possible 6; post-test, this increased to 4.44 (SD 0.158; P<0.001), and 23 participants achieved the maximum score of 6.
Worryingly, prior to the intervention, 56.8% of participants would have omitted insulin after a hypoglycaemic episode; this could have devastating consequences, especially if the patient has type 1 diabetes, as it runs the risk of causing diabetic ketoacidosis. This result demonstrates that nursing staff were not familiar with the local hospital guidelines. Encouragingly, post-education, 93.5% of nurses correctly identified that insulin should not be withheld.
All participants, both pre- and post-test, correctly identified the need to document a hypoglycaemic episode in the nursing notes and inform the medical team of the episode.
Discussion
This pilot study drew on the KAP-O research framework, which implies that educational interventions improve knowledge; improved knowledge enhances practice; and improved practice leads to improved outcomes (Wan et al, 2016).
The results suggest that a bite-sized educational intervention enhanced overall hypoglycaemia knowledge and management. The pre-test questionnaire identified significant gaps in knowledge among some nurses in areas such as definition, causes, signs and symptoms, and management of hypoglycaemia. Nurses’ overall knowledge scores significantly increased post-intervention. Similar studies have also demonstrated improvements in knowledge and treatment of hypoglycaemia (Engvall et al, 2014; Araque et al, 2018).
Pre-intervention, 22.1% and 5.2% of nurses considered a hypoglycaemic episode to occur at <3.0 mmol/L and <2.5 mmol/L, respectively. This is alarming and may be a reason why hypoglycaemia treatment is often delayed in hospitals. These results are similar to those of Chinnasamy et al (2011) and Strider and Phillips (2011). However, in contrast to these results, Lange and Pearce (2017) established that 75% of nurses correctly identified the correct hypoglycaemia level, with similar findings in studies by Holmes and Dyer (2013), Ndebu and Jones (2018), and DeSousa et al (2018). One possible interpretation of the difference in scores between studies is that there is wide variation in nurses’ knowledge; this would underscore the importance of assessing knowledge among staff. An international, longitudinal, multicentre randomised control study to assess hypoglycaemia knowledge would be beneficial to determine this.
The pre-test knowledge scores in this study are more closely aligned with the findings of Chinnasamy et al (2011), in which knowledge of the correct blood glucose level for hypoglycaemia was relatively poor. The-post education results showed an improvement in knowledge in this area, making the results more comparable with those of Holmes and Dyer (2013), Ndebu and Jones (2018), and DeSousa et al (2018).
A deficiency in nursing knowledge regarding the causes and risk factors of hypoglycaemia was identified. This can endanger patient safety and reduce nurses’ ability to provide advice to patients on how to avoid hypoglycaemia in the future.
Participants had an overall poor knowledge of the common hypoglycaemia treatments. This result is similar to findings from Coats and Marshall (2013), in which only 40.4% of respondents were able to correctly treat a hypoglycaemic episode. In contrast, in the study by Lange and Pearce (2017), 97.1% of respondents were able to select the correct treatment.
The present study also revealed that only 22.1% of nurses had received hypoglycaemia management training in the past five years. Nurses’ knowledge on this subject needs to be reinforced and regularly updated through continuing professional education and training.
Study limitations
This pilot study was conducted in a single small hospital and hence the results may not be generalisable to other nursing areas. The study also used a non-probability, convenience sample of nurses, thereby lacking representation of the entire nursing population. There was also a lack of a control group – many threats to the internal validity can be ruled out with the inclusion of a control group and, ideally, the intervention should be examined within a randomised control trial.
Future considerations and changes made post-study
This study led to a reflection on current diabetes education practice: in particular, how the training offered can address the knowledge gap. The brief, bite-sized education has been rolled out to all nurses within the hospital. It is also included as part of the orientation programme for new nurses. The provision of accessible educational diabetes programmes is essential, and ongoing assessment of their effectiveness is a vital consideration. It is not sufficient merely to highlight a shortfall in knowledge; there is a duty to develop training and support networks to increase the knowledge of colleagues and also to prevent staff from becoming de-skilled (Holmes and Dyer, 2013). A re-audit of inpatient hypoglycaemia will be carried out in the future.
This pilot study also identified poor treatment of hypoglycaemia; for this reason, the co-investigator rolled out “Hypo boxes” across the wards. These orange boxes contain the correct initial treatments for mild, moderate and severe hypoglycaemia. The boxes contain cartons of orange/apple juice, bottles of Lift (a glucose shot), GlucoChews, Glucogel and intramuscular glucagon. They will assist all ward-based nurses in the correct treatment and management of hypoglycaemia.
Ideally, the H-KAM educational intervention should focus not only on nursing staff but also on the medical teams, as they prescribe diabetes medications for the inpatients. The co-investigator aims to develop online education training so that all staff will have easy access to this information at a time that suits them.
Conclusions
The findings of this pilot study clearly emphasise the positive impact of an educational intervention to influence and enhance nurses’ management of hypoglycaemia. Nursing staff are at the forefront of health service delivery, conducting the highest proportion of direct patient care. Hypoglycaemia poses a significant health burden to individuals, their households, communities and the healthcare sector. Therefore, the role of the nurse becomes pivotal in providing safe, effective and evidence-based care to achieve optimal clinical outcomes.
Acknowledgement
This article is based on research undertaken at the National University of Ireland, Cork, in 2020/2021 for Marion O’Donovan’s Master’s degree in Advanced Nursing Practice. The dissertation was submitted and completed in May 2021.






Quick links to the best resources, publications and research for all nurses with an interest in diabetes.
20 Jun 2025