Due to the astounding spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), much interest has arisen in epidemiological factors underlying individual susceptibility to COVID-19, to explore effective preventative options. Nutrition is one of many factors that determine the immune response (Calder, 2021). The World Health Organization (2020) published nutritional guidelines in the context of the COVID-19 pandemic, emphasising the importance of dietary interventions to maintain an effective immune system and to reduce or eliminate chronic conditions and infections. The guidelines suggest eating fruits, vegetables, nuts and whole grains; drinking water every day; and limiting sugar, saturated fat and salt intake.
Type 2 diabetes is one such chronic condition. Hyperglycaemia has been shown to increase the risk of severe COVID-19 and is associated with increased mortality in people with diabetes (Mazori et al, 2021; Michalakis and Ilias, 2021). This review of the literature will describe the influence of nutrition as it relates to diabetes, immunity, and COVID-19, and provide evidence-based recommendations for strengthening one’s immune system.
Background
Early in the COVID-19 pandemic, it became clear that obese, frail, chronically ill and older adults were more susceptible to serious disease and mortality from SARS-CoV-2 infection than those who are young and those with a BMI within healthy limits (Williamson, 2020). Poor glycaemic control (HbA1c >59 mmol/mol [7.5%]) in people with diabetes is independently associated with poor outcomes (Williamson, 2020). Researching the relationship between type 2 diabetes, immunity, and COVID-19 can assist in formulating nutritional recommendations for nurses to inform patients on how to boost their immunity.
Type 2 diabetes
Insulin resistance, hyperglycaemia and impairment of insulin secretion are characteristics of type 2 diabetes (Robertson and Udler, 2021). Insulin resistance can be attributed to predominantly modifiable environmental factors, such as overeating and a sedentary lifestyle, which result in being overweight or obese. Less prominent are non-modifiable factors such as ageing and genetics. Impaired insulin secretion most often results from the programming of the beta-cell mass and function in utero and genetic influences. Hyperglycaemia alone can worsen the metabolic state by weakening pancreatic beta-cell function and exacerbating insulin resistance, causing a vicious cycle (Robertson and Udler, 2021).
Immunity
The human immune system’s primary role is to protect the individual against pathogenic organisms such as viruses, bacteria, fungi and parasites. The immune system has evolved to include an array of different cell types to meet the demand of providing protection against a variety of threatening organisms. Several components affect the immune response, including non-modifiable factors such as genetics, time of day, and stage of life (i.e. pregnancy, infancy and advanced age). Modifiable factors, such as physical fitness, body fat, stress, frailty and diet, influence immunity as well (Calder, 2021).
SARS-CoV-2
Coronaviruses are a group of large, non-segmented, positive-sense, single-stranded RNA viruses isolated from several species and have been known to cause respiratory illnesses, such as the common cold, and – less frequently – gastrointestinal infections in humans (Chen et al, 2020). In December 2019, a new coronavirus known as SARS-CoV-2 was identified in Wuhan, China. Although SARS-CoV-2, the seventh known human coronavirus, is similar to SARS-CoV, which caused an outbreak in 2002, the former is new to the human immune system and, therefore, humans have no existing immunity against it. This lack of immunity explains the rapid spread of COVID-19 and the severity of the disease. It has also exposed the importance of having a well-functioning immune system (Chen et al, 2020).
Review of the literature
The topic at hand focuses on the relationship between three elements: nutrition, type 2 diabetes and COVID-19. Since ample research has been conducted on the role of nutrition in diabetes management, far predating the outbreak of COVID-19, the attention in the present narrative review is on a limited number of articles within literature regarding two main ideas: the relationship between diabetes and COVID-19, and the effects of nutrition on contracting COVID-19.
The literature is arranged according to a logical progression below, suggesting that people with diabetes are at increased risk of contracting severe COVID-19, good nutrition bolsters the immune system and, therefore, good nutrition benefits someone who contracts COVID-19. Tighter connections between the tripartite relationship of type 2 diabetes, nutrition and COVID-19 can be drawn based on the representative literature under review. Access to nutrition during pandemic lockdowns was a peripheral issue but is a common thread in the literature, so it is also treated below.
Diabetes and COVID-19 risk
In studies exploring molecular and cellular mechanisms, angiotensin-converting enzyme 2 (ACE2), which is expressed by epithelial cells of the lung, intestine, kidney and blood vessels, is a receptor for SARS-CoV and SARS-CoV-2 (Marhl et al, 2020). Consequently, the increased expression of ACE2 could facilitate infection with COVID-19 and might be a link between increased risk of COVID-19 and diabetes. Marhl et al (2020) proposed that ACE2-stimulating medication, along with dysregulations such as stress, dietary concerns and decreased physical activity, might enhance the risk of contracting COVID-19 in people with diabetes. Early in the pandemic, Guo et al (2020) and Gupta et al (2020) found no evidence to connect type 2 diabetes with an increased risk of contracting COVID-19. Nonetheless, they went on to summarise that people with diabetes who contract COVID-19 had a poor prognosis and increased mortality in many reports.
Therefore, it remains to be demonstrated that type 2 diabetes increases the risk of contracting COVID-19; however, there is much evidence to suggest that it increases the severity of COVID-19 infection. Iacobellis (2020) reported that people with diabetes accounted for two-thirds of deaths from COVID-19 and 20% of Intensive Care Unit admissions in an early analysis in Wuhan, thus noting that diabetes is a major risk factor for unfavourable outcomes.
Muniyappa and Gubbi (2020) recognise overlapping factors between type 2 diabetes and COVID-19 prognosis. They questioned whether type 2 diabetes contributed independently to COVID-19, since cardiovascular disease, obesity and hypertension – all established risk factors for COVID-19 severity – are also commonly found in people with type 2 diabetes. They observed that plasma glucose levels and type 2 diabetes are independent predictors of mortality in patients with COVID-19.
As time passed after the onset of the pandemic, confidence grew about type 2 diabetes increasing the risk of severe COVID-19. Michalakis and Illias (2021) saw correlations between poor glycaemic control and severity of COVID-19 infection and mortality. Interestingly, they also observed an inverse relationship, with COVID-19 worsening glycaemic control in people diagnosed with diabetes. An area of further study is whether glucose levels return to normal after COVID-19 has resolved, remitting an initial diabetes diagnosis that arises from first contracting COVID-19. A global registry of patients with COVID-related diabetes, the COVIDIAB Project (https://covidiab.e-dendrite.com), could help to provide answers.
Nutrition and the immune system
Research reveals that overall health is improved and maintained by following a healthy lifestyle that includes a good diet and supplements. Consequently, good nutrition is a natural weapon in an individual’s fight against COVID-19. While Lange and Nakamura (2020) concede that no single food, nutrient or dietary supplement is capable of preventing COVID-19 infection, they imply that good nutrition does have a positive effect, and argue that a balanced diet is a prerequisite for an optimal immune system.
Calder (2020) discussed the main purpose of the immune system: to protect a body from outside negative influences such as bacteria, viruses and parasites. Daoust et al (2021) write (p 1075):
“Two decades ago, it was shown that the nutritional status of the host not only affects the capacity of the immune system to dampen the viral load but also can influence the virulence of a virus.”
Calder et al (2020) state that following a balanced diet would supply all of the nutrients that assist in supporting the immune system. Calder (2020) also mentions the need for a nutritious diet. He recommends consumption of a varied diet of plant- and animal-based foods that adheres to current healthy eating guidelines to support an optimal immune system. Zildic et al (2020) write that lifestyle and diet modifications including certain nutrients have been shown to improve the immune system.
In the absence of a diverse, well-balanced diet, Calder (2020) recommends supplementing with micronutrients of vitamins C, D and E, along with trace minerals of zinc and selenium.
The effect of nutrition on COVID-19 infection
Beyond the common wisdom that a healthy diet lowers risks of certain diseases, some authors have examined the role of nutrition in protecting against contracting COVID-19, or at least lessening its severity.
Mahluji et al (2021) undertook perhaps the most comprehensive investigation as to how several macro- and micronutrients affect COVID-19, with particular benefits of vitamins C, D and B12, folate, zinc and selenium identified in the prevention and treatment of COVID-19. The authors argue that people with type 2 diabetes, due to their higher risks associated with COVID-19 infection, should receive special attention during the pandemic. Although they recognise that further research is needed to recommended exact treatment doses, they conclude that supplementation with these nutrients can ameliorate COVID-19 symptoms.
Bornstein et al (2020) also discussed the influence of metabolic and glycaemic control on severity of COVID-19, albeit through the lens of medical and surgical solutions, rather than through nutrition. They also noted that their conclusions are based on their expert opinion, with outcomes of clinical trials awaited. Nonetheless, they stated that people with type 2 diabetes should focus on optimal metabolic control, with sustained good glycaemic control as primary prevention for severe COVID-19, with a recommended of HbA1c of <53 mmol/mol (7.0%). Presumably, nutritional strategies designed to control glucose levels would play an important role in this.
Access to nutrition during pandemic lockdowns
Although studies concerning nutrition and COVID-19 have not examined the outcome of lockdowns, this challenge is a common thread in the reviewed literature. Lockdowns and quarantines to suppress the outbreak of COVID-19 complicated the metabolic management of type 2 diabetes by limiting access to some nutritional foods, as well as physical activity. Since poor glycaemic control is an established risk factor for severe COVID-19, Unnikrishan and Misra (2021) stress the need for all patients with diabetes to maintain optimal glycaemic control during the pandemic. They recognise the inherent challenge in achieving such control, due to the difficulties in accessing care and certain medications, and adhering to diet and exercise guidelines during lockdown. Referring to a UK study by Barron et al (2020), which revealed a 2.86-fold increased risk of death from COVID-19 in people with type 1 diabetes and a 1.8-fold increased risk in those with type 2 diabetes, Unnikrishan and Misra (2021) argue that people with diabetes must have blood glucose levels controlled to minimise adverse outcomes of COVID-19.
Jayawardena and Misra (2020) took a regional look at how pandemic lockdowns affected the nutritional habits of people with diabetes. For example, a study of middle-class people in India showed a reduced consumption of fruits and vegetables, alongside an increased intake of other snacks (Mehta et al, 2020; not peer-reviewed). An Italian survey showed that over half of the participants changed their lifestyle, consuming more junk foods and sweets by about two-thirds (Di Renzo et al, 2020). Jayawardena and Misra conclude that a consequence of the lockdown period was a deterioration of dietary habits, which had a major impact on the health systems of developing countries.
Naturally, the situation is direr for those who struggled to access good nutrition even before the pandemic. Lockyer (2020) notes that compromised immune systems of the malnourished, such as children living in poverty in some low-income countries, leads to increased infection rates.
Evidence-based recommendations
Hyperglycaemia is shown to increase the risk of severe COVID-19 and is associated with increased mortality in people with diabetes (Mazori et al, 2021; Michalakis and Ilias, 2021). Therefore, individuals should be educated on a low-glycaemic diet and closely monitor blood glucose levels to achieve optimal control. Education should also focus on the promotion of a well-balanced diet rich in nutrients to promote immunity. This includes at least five servings of fruits and vegetables a day; diets rich in fruits and vegetables provide vitamins including A, C, D, E and B complex, and minerals such as zinc and selenium, all proven (Level 1a evidence) to improve immunity, in the form of reduced proinflammatory mediators and an enhanced immune cell profile (Hosseini et al, 2018). Adding two servings, 90 g each, of fatty marine fish per week provides the recommended levels of omega-3 polyunsaturated fatty acids found to boost immunity (Mendivil, 2021; Level 1b evidence). Salmon, mackerel, herring, sardines and smelt are excellent choices.
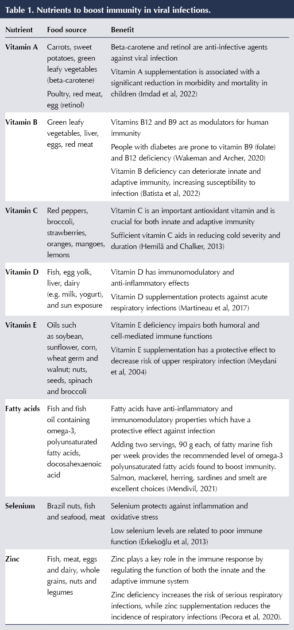
Micronutrients can slow down the processes necessary for viral replication (Calder, 2020). Research specific to COVID-19 and micronutrients is ongoing; however, research has been published regarding successful protocols for other viral infections (Table 1).
Conclusions
Nutrition aiming for optimal glycaemic control, with a focus on micronutrients, has been found to increase immunity and lower the risk of severe COVID-19 in people with diabetes. Nurses who provide care for people with type 2 diabetes are in the best position to educate their patients in ways to promote immunity and prevent infections that may result in serious complications. A diet rich in protein, essential fatty acids, zinc, selenium, and vitamins B9, B12, C and D has been linked to the prevention of infections, including severe COVID-19 (Mahlugi et al, 2021). Further studies on the relationship between nutrition, diabetes and COVID-19 would guide nurses in determining their course of action when teaching people with diabetes about their nutritional needs.





In her final editorial, Su Down reflects on her career and the remarkable progress in diabetes care she has seen.
11 Dec 2025