Using insulin to manage diabetes can be challenging. It requires blood glucose monitoring, the use of insulin pens or a pump, dose titration, responses to hypoglycaemia or hyperglycaemia, and consideration of diet and physical activity. People with learning disabilities (LD) may require additional support to manage their diabetes with insulin and, in accordance with the Equality Act (2010), reasonable adjustments to their care. Nurses working in primary care and specialist services have an important role in supporting people to learn the skills required for optimal diabetes management.
Health inequalities faced by people with learning disabilities
The World Health Organization (2022) defines learning disability as: “…a significantly reduced ability to understand new or complex information and to learn and apply new skills (impaired intelligence). This results in a reduced ability to cope independently (impaired social functioning), and begins before adulthood, with a lasting effect on development.” Multiple long-term conditions are more prevalent in people with learning disabilities (Hanlon et al, 2018), which raises questions about how to make reasonable adjustments and provide appropriate support.
One of the main long-term conditions disproportionately affecting people with LD is diabetes. In a systematic review, the average diabetes prevalence in people with LD was 8.3% (Macrae et al, 2015). According to data, 0.8% of people with LD in England have a diagnosis of type 1 diabetes, compared with 0.4% of the general population. For type 2 diabetes, 6.8% of people with LD have type 2 diabetes, compared with 4.8% of the general population of England (NHS Digital, 2019). People with LD experience poorer health outcomes than those without LD (Cooper et al, 2018; LeDeR, 2021) and are at increased risk of developing diabetes complications due to barriers accessing healthcare (Macrae et al, 2015; Hanlon et al, 2018). The NHS Long Term Plan includes in its goals improving understanding of the needs of people with disabilities and reducing health inequalities (NHS, 2019).
While there is growing awareness of these issues, some aspects of diabetes management require further attention. These include the use of insulin to manage both type 1 and type 2 diabetes. People with diabetes need support, knowledge and skills to use insulin effectively and safely, but those with LD face inequitable access to healthcare and diabetes education (Brown et al, 2017; Smith and Phillips, 2018). Constrained services compromise insulin administration leading to people with LD not receiving their insulin as often as required, missing their glycaemic targets and developing diabetes complications (Brown et al, 2017). Therefore, it is important to outline the current guidance to increase confidence in the diabetes clinical community and highlight the need for further improvements.
Optimising insulin therapy in people with learning disabilities
The principle of person-centred care should be at the forefront when managing insulin therapy in people with LD. Another core principle in diabetes treatment, supported self-management, should be considered within the context of their abilities and their environment. Reasonable adjustments, adapted structured diabetes education and collaboration are key resources in achieving a workable solution.
Person-centred support
The literature reflects the immense importance of person-centred support for people with LD in managing their diabetes (Maine et al, 2017; Holden and Lee, 2021). This can be extended to facilitation of diabetes management with insulin through encouraging the person and enabling them to learn in an accessible way to check their glucose level and administer injections (Whitehead et al, 2016).
At times the need for support to manage diabetes with insulin may be frustrating. Interviews with people with LD about their diabetes have described their mixed feeling about needing help from other people (Dysch et al, 2012). A balance is needed between supporting the person appropriately and facilitating their autonomy (Whitehead et al, 2016). A quandary exists between encouraging self-care and access to services for people with LD, while avoiding care that is paternalistic (Hanlon et al, 2018).
Reasonable adjustments
Under the Equality Act (2010), people with LD have a legal right to reasonable adjustments when accessing healthcare. These include flexibility with appointments, being able to have a supporter at their consultation, access to Easy Read information and person-centred care planning.
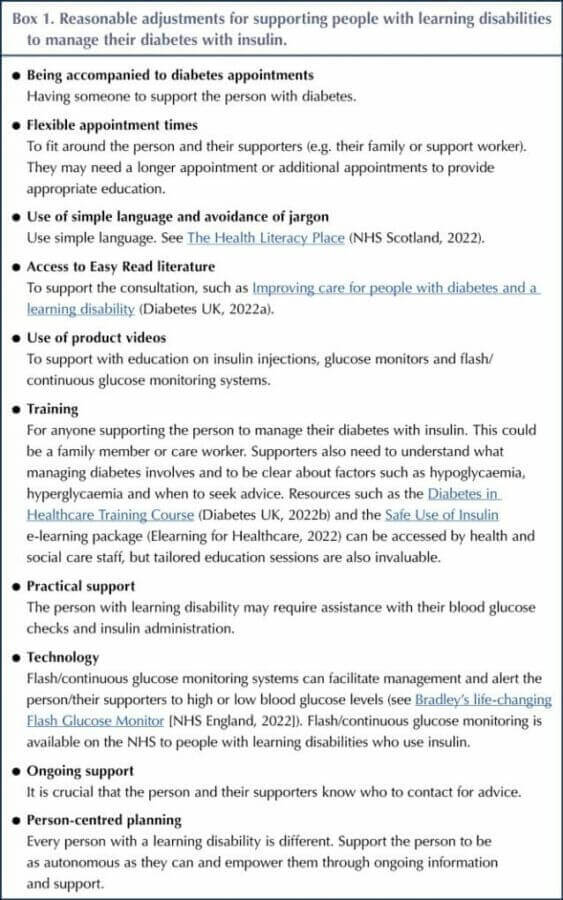
The NHS RightCare Pathway for diabetes emphasised the importance of making reasonable adjustments for people with LD to enable equitable access to optimal diabetes care (NHS RightCare, 2017). The benefits include a reduction in diabetes complications and in hospital admissions, and fewer visits to the GP and missed appointments (NHS, 2017). Systems that do not allow for reasonable adjustments reduce optimal diabetes care in people with LD (Holden and Lee, 2021). Reasonable adjustments are particularly important when supporting people to use insulin because of the safety issues; insulin is one of the top high-alert medicines internationally (Cousins et al, 2011). Box 1 illustrates reasonable adjustments that can facilitate diabetes management with insulin for people with LD. It was adapted by the author from the NHS RightCare Pathway following a focus group in 2019 of people who have LD (and use insulin) and through ongoing discussion with patients, carers and colleagues.
Access to education
Access to structured diabetes education for people with diabetes is an important part of empowerment, self-management and improved health outcomes (Deakin et al, 2006; Walker et al, 2018). However, barriers to accessing diabetes education for people with LD have been identified (Macrae et al, 2015). People with LD may be perceived as being unable to learn the skills required to manage their diabetes with insulin, such as carbohydrate counting in type 1 diabetes (Brown et al, 2017). Conversely, there have been projects to adapt mainstream type 2 diabetes education for people with an LD (Taggart et al, 2015), and research into supportive self-management of type 2 diabetes (Walwyn et al, 2015). However, there is little discussion in the literature of adapted type 1 diabetes education or of education on insulin use specifically. People with LD have expressed the desire for information about their diabetes (Hale et al, 2011; Dysch et al, 2012), so it is crucial for healthcare professionals (HCPs) to find ways of making insulin education accessible. Nurses have a central role in this.
Ability and self-management
A practical consideration for supporting people to use insulin to manage their diabetes is who checks the blood glucose and administers the insulin. Depending on their mental capacity, a person may be able to do it themselves, may require supervision or may need someone to do it for them. Whilst the cognitive ability of an individual with LD may be a barrier to self-management (Brown et al, 2017), to some extent it may be the perceived ability of the person that is the barrier to autonomy. Research into the attitudes of caregivers supporting people with LD who have diabetes found that caregivers were quite negative at times (Cardol et al, 2012a). Some expressed the view that laziness, dependence, lack of intelligence and inability to learn were factors affecting the ability of the person with diabetes to manage their condition.
However, in a study of how people with LD perceive and manage their diabetes, a relationship was found between a better understanding of diabetes and more self-management (Cardol, 2012b). Motivation, confidence and support from others were more important than disability in using knowledge and developing self-management skills. Similarly, Maine et al (2017) described confidence and competence in diabetes self-management for people with LD being closely linked with knowledge, experience and appropriate strategies to overcome barriers.
There are gaps in research focusing on how people with LD manage their diabetes with insulin and in studies that include people who cannot participate in conventional verbal interviews. Some people with LD have, therefore, been excluded from research and their experiences have not been explored. Studies that include participant observation could allow for more inclusive research.
Technology
With advances in diabetes technology, it is appropriate to facilitate access to flash/continuous glucose monitoring systems for people with LD. Changes to NICE (2022) guidelines mean that such technology is more accessible to people with diabetes generally and, for those with LD, this is already a way of supporting them, their families, and carers to monitor blood glucose and respond appropriately. There are challenges to using technology, so reasonable adjustments, such as one-to-one education and more frequent reviews, are important for individuals with LD to fully benefit.
Collaboration
Research focusing on people with LD and diabetes frequently cites collaboration as being a vital part of supporting diabetes management (Trip et al, 2016; Brown et al, 2017). This is particularly in relation to the person with diabetes, their families and their support workers, but extends to HCPs. Decisions about insulin regimens and care plans may take place with the multidisciplinary team, and joint working between diabetes and LD teams has been advocated (Brown et al, 2017). Responsibility for insulin may be shared between people with LD and the staff who support them (Rouse and Finlay, 2016); the importance is working together to facilitate diabetes management. Where there is inadequate collaboration and communication with HCPs, people with LD are less likely to engage with diabetes services (Cardol et al, 2012b) and are more likely to miss appointments (Whitehead et al, 2016).
Practical considerations
For people requiring practical support to use insulin, care needs to be tailored but there are constraints to facilitating this. If the person can check their own blood glucose level and self-inject insulin, it may be straightforward, provided they receive appropriate education, information and support. However, for individuals requiring additional help with these skills, it depends on who they live with and what one-to-one support they have access to.
For people who cannot inject their own insulin, it can be especially challenging to ensure that the right level of care is received. If there is no family support, the responsibility may lie with district nurses. Depending on how services are commissioned locally, it can be difficult to provide daily visits, especially if the person requires insulin more than once a day (such as in type 1 diabetes). Compromises with the insulin regimen are often made (Brown et al, 2017) and can be a barrier to optimal diabetes management (Holden and Lee, 2021).
Despite resource challenges, a project to improve service standards for people who are housebound and need insulin has demonstrated that providing appropriate support is feasible (Gregory, 2019). The Delegation of Insulin Administration project is a voluntary framework giving expanded capacity to health and social care workers who administer insulin to people living with diabetes (Diabetes UK, 2022c). This is an effective way of managing service demands and improving patient care (Castro et al, 2021), but it does not cover the administration of insulin in individuals whose diabetes is unstable. More work needs to be done to explore the experiences of people with LD requiring a higher level of support with their insulin management.
Conclusion
People with LD may need additional support to manage their diabetes with insulin. It is important to strike a balance between the provision of appropriate support and information to facilitate self-management, and tailored care to ensure that individuals with additional health needs have the right level of practical support. HCPs must work in a collaborative, flexible and person-centred way to ensure that reasonable adjustments are made, but there are resource barriers to providing optimal support to people who need help to administer their insulin injections. The Delegation of Insulin Administration project is likely to play an increasingly important role in facilitating diabetes management in people with LD who use insulin. The ongoing provision of information and training to people living with diabetes and their supporters is crucial to encouraging effective diabetes management with insulin. Research should focus on how people with LD manage their diabetes with insulin, and should be inclusive for people who cannot participate through conventional verbal interviews, to ensure their needs are addressed.
This article was written as part of an Integrated Clinical Academic Internship (HEE/NIHR) at Oxford Brookes University.






Developments that will impact your practice.
26 Jun 2025