Successful management of chronic conditions such as diabetes requires individuals to learn a great deal of information about the condition, its management and treatment strategies to prevent further complications. Improved self-management of diabetes leads to improved clinical outcomes such as glycaemic control (Khairnar et al, 2019). Self-management can be supported through diabetes education; however, individuals with lower health literacy have poorer diabetes self-management and higher rates of complications (Yale et al, 2018). To date, multiple health literacy tools have been developed, some of which are specific for diabetes assessment; however, their applicability in clinical use is questionable.
Diabetes and self-management
Diabetes self-management is about empowering individuals to take control of their lives and improve their health. Supportive education to promote a better understanding of diabetes management is required to meet patients’ needs (Pal et al, 2018). Reduced participation in self-care could negatively impact the individual’s awareness of their health, lead to worse health outcomes, increase preventable healthcare costs and have a financial impact on society (Docteur and Coulter, 2012).
Biomedical technologies such as telemedicine, telemonitoring and home care exist to improve health; however, it is important to consider the individual’s needs, based on their beliefs, to help with gradual knowledge transfer and empowerment (Storni, 2015). Diabetes self-management requires active participation, and the modern medical philosophy of separating the client from the disease is not a method to succeed.
Diabetes self-management is an open path to multiple methods and ways of acquiring knowledge, as every individual and their experiences are different (Storni, 2015). It is essential to adapt education to personal needs and levels of understanding. If their knowledge of the information is enhanced and support is provided based on their needs, patients can be empowered. Due to the complexity of diabetes, two individuals living with this condition cannot be treated the same way, and they cannot be expected to live the same way because their education level and understanding of the educational information are different.
Barriers to diabetes self-management
Studies reveal significant barriers to accessing diabetes education. For example, when people travel long distances to their primary care clinic for face-to-face appointments, diabetes management may be more difficult (Strauss et al, 2006; Zgibor et al, 2011). Additionally, physical access to healthcare services (Zgibor et al, 2001) and access to transportation (Saunders, 2019; Zgibor et al, 2001) can be further barriers to diabetes management. In particular, older adults experience challenges travelling to clinics, especially during the winter months or when regular and intense follow-up is needed.
Virtual visits and telehealth can remove travel and transportation barriers while creating an accessible means for delivering care to individuals with chronic conditions (Kelley et al, 2020). The need to move face-to-face clinic visits to a virtual modality has become more pronounced during the COVID-19 pandemic. Many healthcare and other providers are examining distance delivery of services, which is particularly important for people with diabetes, who are at higher risk of complications if they contract COVID-19.
Lack of individualised care by diabetes educators can be a barrier to diabetes management (Brämberg et al, 2012; Saunders, 2019). Understanding every patient’s unique healthcare needs and adapting the educational information to meet their health literacy level is essential (American College of Obstetricians and Gynecologists, 2016).
Health literacy is defined as a collection of capabilities, including to perform basic reading and numerical tasks that are essential to function in the healthcare environment, such as reading and comprehending the necessary health-related materials (Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, 1999). Lower health literacy can negatively affect diabetes self-management (Yale et al, 2018). A lack of consideration for individuals’ existing health literacy levels can prevent them from following medical advice related to nutrition and medication, thereby worsening their medical condition (Nam et al, 2011). For instance, people can learn diabetes management techniques such as insulin injections more easily than insulin titration because the latter requires complex problem-solving skills involving self-management (Bonnet et al, 1998). Self-management requires understanding and maintaining information to perform proper self-care.
Person-centred care creates a safe environment for people to exchange information with the healthcare provider (Inzucchi et al, 2012). Understanding a person’s health literacy can help healthcare providers tailor education to the individual’s needs, which also improves patient satisfaction (Watts et al, 2017).
Critical pedagogy offers one approach to assessing health literacy. Three fundamental elements of critical pedagogy are dialogue and reflection, problem posing, and problem solving (Dawkins-Moultin et al, 2016). Dialogue and reflection focus on determining precise health literacy needs, problem posing aims to explain the reasons underlying problems and problem-solving investigates resolutions (Matthews, 2014). These fundamental elements provide a broader view when assessing a person’s health literacy. Healthcare professionals need to understand health literacy to properly assess it in their patients in order to support self-management (Saunders et al, 2019). Therefore, an initial assessment of the person’s health literacy serves as a first step to change the clinician’s behaviour (McNeil and Arena, 2017).
Virtual visits
Information communication technologies such as the telephone have been around since 1876. The medical profession was the first to adopt the phone to communicate, monitor and deliver healthcare information services from a distance (Zundel, 1996). For continuity of care, virtual visits by telephone and video conferencing can support patients if they cannot make face-to-face visits to the clinic (Hakim et al, 2020). Due to the COVID-19 pandemic, the number of virtual visits has increased significantly in order to protect vulnerable communities (Triana et al, 2020). The pandemic has created a more challenging time for diabetes management in general and especially for the elderly (de Lima Filho et al, 2020).
Video conferencing
Video conferencing offers a biopsychosocial model of health (Triana et al, 2020), which looks at illness and healthcare in a complete view and considers the influence of psychological and social factors (Wade and Halligan, 2017). Through video conferencing, healthcare providers can connect and communicate with clients in real time and address their concerns. Additionally, video conferencing provides an opportunity to connect to the patients within their home environments (Triana et al, 2020). Technologies increase accessibility and quality care by allowing individuals to communicate with healthcare providers, helping clinicians manage the continuously increasing workload at a lower cost to the system (Schwamm, 2014).
Despite the availability of various platforms, the reality is that video conferencing is not accessible to everyone. Virtual visits requiring audio and video could be challenging for some clients even if they make the necessary arrangements (Triana et al, 2020). Existing worldwide telehealth implementation may increase healthcare access inequalities for those with limited access, including people who live in rural areas, those from minority groups, those with a low income and those with low health literacy (Nouri et al, 2020). Even though older people may have access to a smartphone or computer, not all use email or text messaging or have internet access (Gell et al, 2015; Bulman et al, 2020). In addition, smartphone features are not always accessible for the elderly (Anam and Abid, 2020). Therefore, despite health and e-health programs, the lack of access puts the elderly at a disadvantage (Gell et al, 2015). The literature suggests that the telephone can provide greater access to care (Bulman et al, 2020).
Telephone visits
Providing education via the telephone can empower self-management of a person’s diabetes (Zamanzadeh et al, 2017). Telehealth creates a more person-centred approach by providing an alternative to existing traditional ambulatory and hospital-based practices (Schwamm, 2014). Diabetes nurse educators providing coaching via telehealth can improve individuals’ health behaviours in diabetes management, especially in rural areas (Young et al, 2014). Evidence shows that telehealth can improve glycaemia and other health-related outcomes sustained in a longer duration compared with in-clinic visits (McDonnell, 2018).
Improving virtual visits
Having access to both telephone and video visits provides a greater selection for patients (Nouri et al, 2020) and allows them to choose the method of delivery of care (Bulman et al, 2020). Understanding the individuals’ needs will help them feel that they are an integral part of the care team (LaDonna et al, 2017). Continuity of care, the relationship between patients and providers, and having clear communication and understanding during the virtual visit are crucial to effective chronic disease management (Nouri et al, 2020). Unfortunately, due to health literacy barriers, many people cannot understand and implement the education provided to them during the visit with their healthcare provider (Batterham et al, 2016).
Intermittent pausing during in-person visits with patients creates an opportunity to observe facial expressions, gestures or body language, and is necessary to developing understanding and connection (Partida, 2007). Virtual visits are feasible, cost-effective and appealing compared with face-to-face, in-clinic visits (Robb et al, 2019); however, the lack of visual cues during telehealth visits can make it more challenging to understand patients, especially those in marginalised groups and those with lower health literacy (Glauser, 2020). Additionally, it is difficult to assess if healthcare providers are missing important information through the virtual visit (Glauser, 2020).
Health literacy assessment
The COVID-19 pandemic has amplified the need for a shift from physician-centred, face-to-face diabetes management to patient-centred teleconsultation (Banerjee et al, 2020). Even though client education through virtual visits is not new, modifications to these visits will help providers offer better education. Specifically, integration of health literacy assessments in a virtual environment may offer unique opportunities to improve care.
Health literacy is evident in the steps that people take to manage their health (Dawkins-Moultin et al, 2016). Most health literacy evaluations emphasise reading skills instead of functional assessments such as navigation, communication and decision-making (D’Eath et al, 2012). Easton et al (2010) pointed out that one of the largely used and adapted health literacy tools, the Rapid Estimate of Adult Literacy in Medicine (REALM), mainly focuses on an individual’s reading skill and does not assess motivation, understanding or capability to access or use health-related information; therefore, the REALM’s assessment of health literacy is closely associated with assessments of functional literacy. Consequently, individuals who score high on functional literacy are most likely to receive a high score on the existing measures of health literacy even though their actual health literacy level may be low. This phenomenon is described as the “hidden population” of adults who can communicate and converse well with their dominant language but whose health literacy issues may not be detected by healthcare providers.
Research shows that health literacy can be improved through health education (Cho et al, 2008; Ntiri and Stewart, 2009; Walters et al, 2020). When diabetes self-management education is being provided, the person’s health literacy needs to be assessed and accommodated because people with inadequate health literacy may not be able to translate the information into appropriate action (Budge and Taylor, 2020). A systematic review by Walters et al (2020) has identified a number of health literacy interventions that offer to improve health literacy, health behaviours and outcomes in people with health inequality risk. Additionally, associations between health literacy and medication engagement have been identified (Chima et al, 2020). Therefore, there is a need for a health literacy tool that can address people’s informational needs (Altin et al, 2014).
Health literacy is essential for client engagement (Coulter and Ellins, 2007). If individuals cannot acquire, process and comprehend basic health-related information, they will not be able to perform self-management or make appropriate decisions regarding their health. Kim and Xie (2017) identified that “barriers to access to and use of online health information can result from the readability of content and poor usability of eHealth services. We need new health literacy screening tools to identify skills for adequate use of eHealth services” (p. 1073). Improving health literacy is necessary for reducing health inequalities (Coulter and Ellins, 2007). It is established that lower literacy levels result in poor health outcomes and inappropriate use of healthcare services (Berkman et al, 2011). Consequently, individuals with lower health literacy are considered “heavy users” of healthcare services (Watson, 2011). Hence, there is a link between lower health literacy and increased risk of mortality and shorter life expectancy (Peterson et al, 2011).
Scoping review on health literacy tools
Drawing from existing research and my experience as a diabetes educator, I identified the lack of a standardised health literacy tool to help practitioners to better understand the needs of their patients. In this scoping review, I focus on exploring health literacy assessment tools related to diabetes management and consider their impact within a virtual environment. This review aims to improve the resources available to clinicians, with the ultimate aim of improving diabetes education and care.
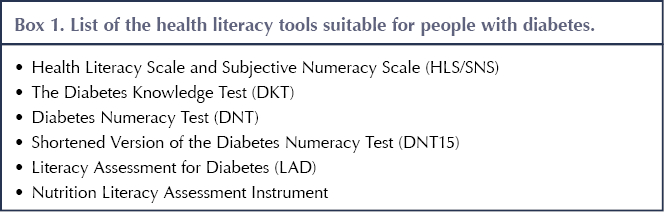
Several health literacy assessment tools have been developed. The Health Literacy Tool Shed (https://healthliteracy.bu.edu) has created an easy-to-access database of all the validated health literacy tools (Harnett, 2017). I reviewed the Health Literacy Tool Shed and noted it to contain 200 validated and reliable health literacy tools. I found 12 tools that were specific for diabetes health literacy. Of these, six were excluded because they were optimised for specific countries and one because it was for adolescents only; thus, they were not generalisable. A further scoping review and assessment of the Discovery database and Google Scholar identified one additional diabetes health literacy tool that was not noted in the Health Literacy Tool Shed. Therefore, the tool was added to the list of tools to be included in the present review of diabetes health literacy tools (Box 1).
Composite Health Literacy Scale and Subjective Numeracy Scale
The Health Literacy Scale and Subjective Numeracy Scale (HLS/SNS) is a two-part scale, the first part of which (the HLS) includes multiple-choice questions while the second part (the SNS) includes a narrative questionnaire allowing users to share their subjective view. A literature search of the HLS/SNS revealed eight articles, of which three were duplications, one was not diabetes-related and one was about a different test. Koonce et al (2015) included the SNS and Diabetes Knowledge Test (see below) as a health literacy scale and adapted educational materials for US grades five and eight (ages 10 and 13 years) reading levels. The study concluded that adapting the educational materials to a patient’s health literacy level will improve their diabetes knowledge.
Luo et al (2020) revealed that, together, higher health and numeracy literacies resulted in higher self-management, but the SNS did not show improvement in self-management when tested individually. One study modified the HLS/SNS and incorporated a medication scale for diabetes, and concluded that in order to encourage medication adherence, health literacy and numeracy skills should both be considered when designing education materials for the person with diabetes (Nandyala et al, 2018). Additionally, Luo et al (2018) assessed the composite HLS/SNS and concluded that the instrument is reliable and valid to measure diabetes literacy.
Diabetes Knowledge Test
The Diabetes Knowledge Test (DKT) has 23 multiple-choice questions. Of six articles that related to the DKT, one was in Korean, one was a duplication and one was a letter to the Editor. The tool was deemed culturally appropriate when adapted to the specific culture (Hasan et al, 2020). As previously mentioned, Koonce et al (2015) assessed the combination of the SNS and the DKT as health literacy scales, and showed improvement in participants’ diabetes knowledge. The DKT was also assessed and modified for nursing personnel and not patients (Haugstvedt et al, 2016).
Diabetes Numeracy Test
The Diabetes Numeracy Test (DNT) is a questionnaire with 43 questions. A shortened version has also been developed, reducing the number of questions to 15 (the DNT15), and another has reduced the number of questions to five (the DNT5). A few questions have multiple choice answers, but some (including one in the DNT5) have illustrated parts such as nutrition facts.
Out of 17 articles identified, six were duplications, one was in Chinese, and one studied adolescents only. Two articles adapted the literacy tools for the Arabic language and tested its validity, demonstrating it to be valid and reliable (Alghodaier et al, 2017; Hasan et al, 2020).
Numeracy assessment is essential, and the DNT is a validated and reliable tool that can be used in people with diabetes (Huizinga et al, 2008; Vacher and Chavez, 2009). The DNT was noted to be stronger than subjective tools when tested in people with diabetes from minority ethnic backgrounds in the US (Chakkalakal et al, 2017). Omar et al (2020) administered the DNT via the WhatsApp instant messaging app and found no correlation between DNT score and diabetes improvement through blood work results. Another study revealed that better glucose control was associated with higher DNT15/DNT5 scores, and lower numeracy can be a barrier to adequate diabetes management (Zaugg et al, 2014). Bowen et al (2013) showed that participants with lower numeracy consumed a higher percentage of calories from carbohydrates and lower percentages from protein and fat; however, the results were not significant after adjustment for other confounding variables. Turrin and Trujillo (2019) revealed that people with lower diabetes numeracy knowledge, as assessed by the DNT15, had higher HbA1c and worse self-described diabetes self-care.
Literacy Assessment for Diabetes
The Literacy Assessment for Diabetes (LAD) is a modified version of the Rapid Estimate of Adult Literacy in Medicine (REALM), which is used to assess health literacy in people with diabetes; however, participants are asked only to read a series of words. Individual literacy levels are assessed based on pronunciation of the terms.
In this literature search, four articles were found that discussed the LAD. The LAD was one of the literacy tools adapted for the Arabic language by Hasan et al (2020). Nath et al (2001) established the validity and reliability of the LAD in older people, prisoners and employees of a primary care clinic through comparison with the REALM and the Wide Range Achievement Test 3 (WRAT3). Ntiri and Stewart (2009) assessed transformative learning with health literacy tools and questioned the effectiveness of using only word recognition in assessing health literacy. They pointed out that pronunciation of words alone might not reflect the health literacy of the individual.
Nutrition Literacy Assessment Instrument
The Nutrition Literacy Assessment Instrument (NLAI) is based on a series of questions with multiple-choice answers, but some questions are based on pictures and visual images. Of five articles identified that were related to the NLAI, two were conducted only in children. In the other three, the developer of the NLAI sought to test, retest and improve the tool’s validity and reliability (Gibbs and Chapman-Novakofski, 2013; Gibbs et al, 2017; Gibbs et al, 2018).
The gap in existing health literacy tools
This literature review shows that several health literacy measures have been developed based on previously considered standardised health literacy tools; therefore, many of these tools have a solid connection or similarities to each other (Jordan et al, 2011). While many of these tools are based on reading comprehension, the majority have poorly defined scoring. Moreover, a tool based on reading comprehension lacks transferability for use with people who speak English as a second language.
A more comprehensive tool needs to be developed that is more practical in the clinical setting (Jordan et al, 2011). A practical tool would be short, reliable and valid, and could be used by healthcare providers in any clinical setting (specialised or primary care clinics). Despite the growing body of research on the need to improve health literacy, a standard measure is yet to be developed in Canada to help healthcare providers better assess their patients’ health literacy levels. While there is a lack of standardised health literacy measurement methods or tools both nationally and internationally, many health literacy tools are available to support healthcare providers in assessing an individual’s health knowledge.
To date, the majority of the research that links low health literacy with health status has included many minority groups, whose difficulties with literacy are more easily recognisable by healthcare providers (Easton et al, 2010). Since the focus of existing research has primarily focused on these “visible minorities”, it can create significant variance in the methods in which literacy can affect health because of “hidden health illiteracy” discussed earlier.
The future
A diabetes health literacy assessment that is adapted for virtual visits can be used at the initiation of the first visit with a patient, and can be reassessed after education has been provided in order to see if the individual’s health literacy has improved. Health literacy education can lead to health-related empowerment and personal autonomy (Grace and Bay, 2011) by allowing clients to be better engaged in their care.
The internet is a source of information for some people; however, finding reliable information and credible sources can be challenging. Even though educational materials are available online, without health literacy it is difficult for people to differentiate between valuable and false information.
Diabetes management is challenging because it requires education that considers a variety of factors (Meng et al, 2016). Smartphone interventions are useful in helping individuals with diabetes to perform self-management (Aminuddin et al, 2019). However, readability and unsuitable usability issues interfere with individuals’ accessibility of online information; therefore, there is a need for a health literacy screening tool that will allow for adaptation of information or education based on a person’s needs and health literacy level (Kim and Xie, 2017). If a health literacy assessment tool that can meet various needs becomes standardised, not only can it be used for virtual visits but it can also be used with individual health applications available online to adapt to patients’ learning needs.
Conclusion
Living with and managing diabetes requires significant effort, from monitoring blood glucose and food intake to taking the proper amount and dosage of antihyperglycaemic medications. Virtual visits to receive education regarding diabetes self-management are essential but require the necessary tools to improve delivery of education. Research reveals that health literacy can play an essential role in diabetes self-management. Even if the information provided does not lead to behaviour change in an individual, a healthcare provider has to ensure the person understands the information provided to them. Deciding not to follow the information is different from not understanding the information.
There are many existing health literacy tools, including some specific to diabetes, but none have been used consistently in practice settings or added to diabetes management guidelines. There is a need for a tool that can be easily used in multiple methods of education delivery, including face-to-face and telephone visits. Ultimately, the development and evaluation of a health literacy tool centred within a virtual environment offers the opportunity to improve the care and overall health of those living with diabetes.
Suggestions for further research
This scoping review has demonstrated numerous areas for research development. Further research is needed on assessing the effectiveness of health literacy tools in virtual environments and the development of diabetes-specific resources relevant for telehealth care services.




How a new model of care has improved outcomes for people with diabetes.
2 Dec 2025