The identification and management of hypertension in people with diabetes is of paramount importance because it plays a key aetiological role in the development of cardiovascular disease (CVD; including myocardial infarction and stroke). People with diabetes have a significantly higher frequency of CVD than those without diabetes. Hypertension is also an important risk factor for microvascular disease, notably diabetic nephropathy and retinopathy (Kenny, 2018).
This article is the first of two, highlighting the problems arising from hypertension, and its accurate measurement and classification. The necessary investigations and actions following the diagnosis of diabetes are discussed, including in the case of severe (accelerated) hypertension. Blood pressure targets, and the evidence supporting them, are reviewed. Finally, the specific situations of isolated systolic hypertension, postural hypotension and hypertension in pregnancy are discussed.
The second article in this series will discuss the treatment of hypertension.
The consequences of hypertension in diabetes
There is strong evidence that hypertension is a causative factor in atherosclerotic CVD (ASCVD; coronary heart disease, cerebrovascular disease and peripheral vascular disease), heart failure and increased mortality in both type 1 and type 2 diabetes (Fox et al, 2015; American Diabetes Association [ADA], 2024). Hypertension is also associated with greater frequency of microvascular complications of diabetes.
Diabetes (especially type 2 diabetes) and hypertension commonly coexist. Around two thirds of people with type 2 diabetes have hypertension (Pavlou et al, 2018). People with both diabetes and hypertension have a cardiovascular risk approximately three times that of those with either diabetes or hypertension alone (Shlomai and Grossman, 2014).
Measuring blood pressure
A clinic blood pressure (BP) reading should be taken with the person seated and resting, and their upper arm supported. The cuff should be at the level of the right atrium. The cuff size should take account of arm circumference, with the bladder encircling at least 80% of the arm, but not more than 100% (Diggle, 2024). If the cuff is too small, measured BP will exceed true BP. Too large a cuff will underestimate true BP.
People with diabetes should have BP measured routinely: at least annually. If hypertension is diagnosed, BP should be measured more frequently until stabilised (de Boer et al, 2017).
If hypertension is suspected, check BP in the other arm. If the difference in readings between arms is >15 mmHg, then any further readings should be taken in the arm with the higher reading (NICE, 2023a).
In the case of an irregular pulse, automated devices are inaccurate for measuring BP. Thus, people with atrial fibrillation should have BP measured manually with direct auscultation over the brachial artery.
Ambulatory or home BP monitoring (ABPM and HBPM) are used to achieve more accurate readings and to exclude white-coat hypertension. Less commonly, ABPM/HBPM may expose masked hypertension, a situation where BP is normal in the clinic (<140/90 mmHg) but is raised outside clinic. There is evidence that home monitoring is a better predictor of ASCVD than clinic BP readings (Banegas et al, 2017).
For ABPM, calculate the average value of at least 14 measurements during waking hours. For HBPM, two consecutive readings should be taken twice daily (in the morning and evening) for a week before calculating an average (NICE, 2023a).
Assessment and diagnosis of hypertension
For a comprehensive flowchart on diagnosing hypertension and the actions to take, click on Figure 1 (Diggle, 2024).
Hypertension has been defined as a sustained clinic blood pressure of ≥140/90 mmHg (de Boer et al, 2017). Whilst this is generally adopted in the UK, it is not universally accepted. The recent American Diabetes Association (ADA) Standards of Care re-defined hypertension as a BP of ≥130/80 mmHg due to evidence of increased cardiovascular risk at these levels (ADA, 2024). The stages of hypertension are summarised in Table 1 (NICE, 2023a).
- If clinic BP is ≥140/90 mmHg, repeat the measurement, taking the lower of two or more readings.
- If repeated BP is ≥140/90 mmHg and <180/120 mmHg, offer ABPM or HBPM to confirm diagnosis of hypertension.
- If average BP from ABPM or HBPM is ≥135/85 mmHg, hypertension is diagnosed.
- If repeated clinic BP is >180/120 mmHg, urgent clinical assessment is required to determine whether immediate referral to secondary care is required or rapid investigation and treatment in primary care is appropriate (see later).


Actions required
For the person with diabetes newly diagnosed with hypertension
If not already performed, measure height and weight and calculate BMI, as a raised BMI is strongly linked to raised BP levels. Check smoking status and alcohol consumption, and review the family history of hypertension, diabetes and CVD.
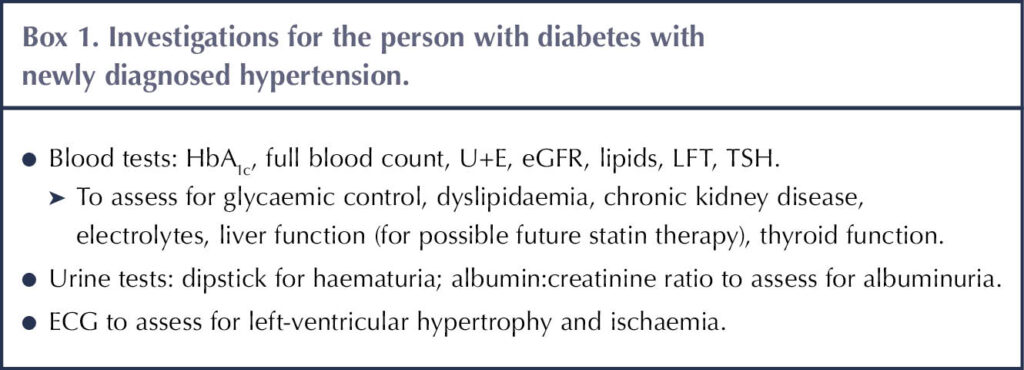
With examination and investigations, the emphasis is to look for end-organ damage (NICE, 2023a). Fundi should be examined for the presence of diabetic/hypertensive retinopathy, and cardiac auscultation should be performed. Relevant investigations are summarised in Box 1.
Cardiovascular risk assessment using the QRISK3 calculator (https://qrisk.org) is recommended for people with type 2 diabetes when results of investigations are known. Consider offering statin therapy for primary prevention of CVD if the 10-year risk of a cardiovascular event is ≥10% (NICE, 2023b). QRISK3 is not recommended for people aged 85 years or older, nor in those with pre-existing ASCVD, who should be offered atorvastatin 80 mg once daily for secondary prevention. For people with type 1 diabetes, QRISK3 should not be used; rather, statin therapy should be offered if subjects are >40 years of age or have had diabetes for >10 years. Atorvastatin 20 mg once daily is recommended for people with either type 1 or type 2 diabetes who have CKD, again without recourse to QRISK3 (NICE, 2023b).
For stage 3 (and accelerated) hypertension
If BP remains ≥180/120 mm/Hg on repeat measurement, the individual needs to be assessed for life-threatening complications (NICE, 2023a). Refer the individual urgently to secondary care if:
- Fundal examination shows signs of retinal haemorrhage or papilloedema (blurring of the optic disc margin, retinal haemorrhages around the optic disc or engorged retinal veins) – i.e. accelerated hypertension.
- Dipstick of the urine shows blood.
- There are severe symptoms (e.g. chest pain, palpitations, shortness of breath, signs of heart failure, severe headache, vomiting, altered vision, confusion or altered level of consciousness).
If same-day referral is not indicated, then carry out the investigations summarised in Box 1 as soon as possible. Should target-organ damage be identified from investigations, consider starting antihypertensive medication without waiting for ABPM/HBPM results. In the absence of target-organ damage, repeat clinic BP or facilitate ABPM/HBPM, ideally reviewing within 7 days (NICE, 2023a).
Evidence supporting blood pressure lowering in people with diabetes
The UKPDS (UK Prospective Diabetes Study) in people with type 2 diabetes revealed that tighter control of BP (mean 144/82 mmHg) compared to less tight control (mean 154/87 mmHg) was associated with a 24% composite reduction in macrovascular and microvascular complications (UKPDS Group, 1998). Subsequently, large randomised controlled trials have confirmed the benefits of BP lowering in diabetes with antihypertensive medication and have supported the BP targets discussed here (Hansson et al, 1998; Schrier et al, 2002; Patel et al, 2007; Cushman et al, 2010; Zhang et al, 2021).
Systematic reviews and meta-analyses of randomised controlled trials looking at antihypertensive treatment in people with diabetes similarly conclude that reducing BP to <140/90 mmHg reduces the risk of ASCVD, heart failure, retinopathy, albuminuria and mortality. Lowering BP to <130/80 mmHg can further reduce the risk of stroke, retinopathy and albuminuria, but without further benefit to other ASCVD or heart failure (Reboldi et al, 2011; Emdin et al, 2015; Ettehad et al, 2016; Xie et al, 2017; Thomopoulos et al, 2017).
A Cochrane review, whilst acknowledging that a lower BP target (<140/90 mmHg) could reduce the incidence of stroke, concluded that this benefit was offset by an increase in adverse side effects, including postural hypotension, falls, electrolyte disturbance and acute kidney injury. (Arguedas et al, 2013). The weight of evidence supporting BP reduction in type 1 diabetes is not as strong as for type 2 diabetes, but similar benefits and BP targets are identified.
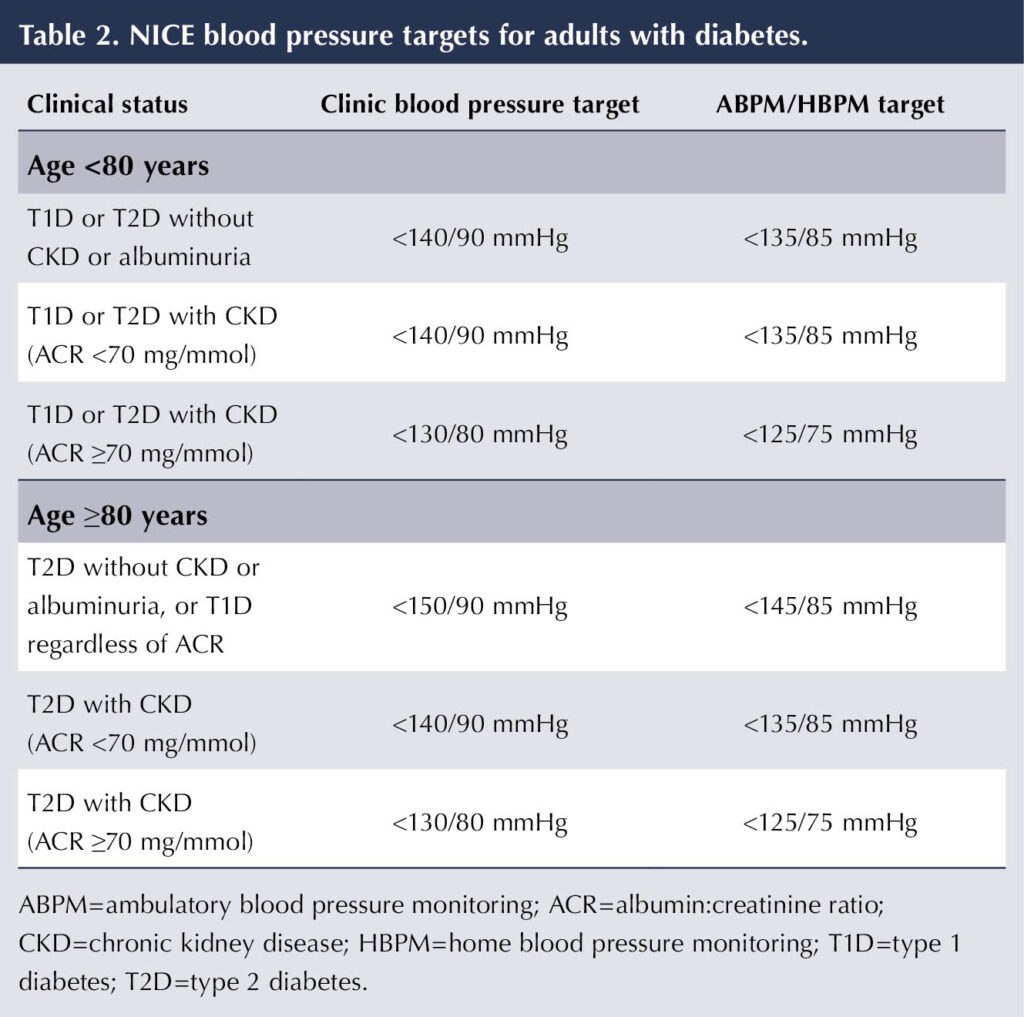
Blood pressure targets – guidelines for people with diabetes
Variation in interpretation of the evidence described above means that there is not consensus on the ideal BP targets for people with diabetes. NICE recommends a target of 140/90 mmHg in clinic or 135/85 mmHg on ABPM/HBPM – the same as for people without diabetes – on the basis that there is insufficient evidence to support aiming for lower targets and that more intensive treatment is more likely to induce unwanted side effects. These targets are irrespective of whether people have coexisting cardiovascular disease (NICE, 2023a).
Acknowledging the increased risk of side effects from using antihypertensive medications in the elderly, NICE advises less intensive BP targets in those aged ≥80 years: a clinic BP of <150/90 mmHg or ABPM/HBPM of <145/85 mmHg (NICE, 2023a).
A lower BP target of 130/80 mmHg is suggested for people with diabetes who have heavy albuminuria (albumin:creatinine ratio ≥70 mg/mmol; see Table 2) (NICE, 2021; NICE, 2023a).
Other guidelines have proposed BP targets lower than 140/90 mmHg, in particular for those with diabetic nephropathy, diabetic retinopathy and stroke. For example, recent ADA guidelines recommend that people with diabetes and hypertension should be treated to a target of <130/80 mmHg. The ADA emphasises that targets and treatments should, however, be tailored to individual circumstances, and that a target of <120/80 mmHg should be avoided because of the risk of side effects (ADA, 2024).
Isolated systolic hypertension
Whilst diastolic BP is an important predictor of morbidity in younger people (notably those aged <50 years without diabetes; de Boer et al, 2017), it becomes less important with age. It is accepted that systolic BP is generally a more powerful prognostic indicator than diastolic BP across age ranges (Arguedas et al, 2013).
Isolated systolic hypertension is common in the elderly. Whilst striving for well-controlled systolic BP, it is important to avoid lowering diastolic BP excessively (say, to <60 mmHg) because of the risks of postural hypotension and adverse cardiovascular events (de Boer et al, 2017; ADA, 2024).
Postural hypotension
Dizziness on standing, which may be associated with falls, is suggestive of postural hypotension and is particularly problematic in the elderly. The possible consequences of a fall in an older person include subdural haemorrhage and fractured neck or femur. While there may be multiple causes of postural hypotension, an important contributing factor in people with diabetes is autonomic neuropathy (Fleg et al, 2016).
It is important to ask about symptoms of postural hypotension in people with diabetes, especially the elderly, and to check BP sitting and standing. Postural hypotension is defined by a fall in systolic BP of 20 mmHg or in diastolic BP of 10 mmHg after the person has been standing for at least 1 minute, when compared with sitting or supine BP (NICE, 2023a).
Use of antihypertensive medications can trigger, or exacerbate, postural hypotension. Postural hypotension is a well recognised side effect of alpha-blockers (e.g. doxazosin), and volume depletion through use of diuretics is another predisposing factor (ADA, 2024).
An individualised approach is required in the setting of BP targets and selection of antihypertensive medication, and nowhere is this more crucial than in the elderly. If postural hypotension is diagnosed, the actions in Box 2 should be taken.
Pregnancy BP targets
Most of the evidence regarding BP targets and outcomes in pregnant women with either chronic hypertension or gestational hypertension comes from women without diabetes, and this evidence is extrapolated to women with pre-existing or gestational diabetes (ADA, 2024).
For women with existing (i.e. chronic) hypertension who are planning a pregnancy, medication should be reviewed for safety and, if necessary, changes made (more information will be available in Part 2). NICE (2019) recommends a target BP of 135/85 mmHg when using antihypertensive medication in pregnancy. If BP exceeds this, the antihypertensive regimen can be intensified. If women are not already receiving antihypertensive medication, this should be offered if BP is ≥140/90 mmHg.
NICE (2019) guidelines for gestational hypertension – new hypertension arising after 20 weeks of pregnancy without significant proteinuria – recommend offering antihypertensive treatment (see details of appropriate medication in Part 2) if BP is persistently >140/90 mmHg, aiming for a BP of ≤135/85 mmHg (NICE, 2019). Once- or twice-weekly monitoring of BP should be undertaken, along with urine dipstick tests for protein, a full blood count, and renal and liver function tests (looking for evidence of pre-eclampsia). Commonly, this will take place in secondary care. If BP reaches ≥160/100 mmHg, hospital admission is recommended.
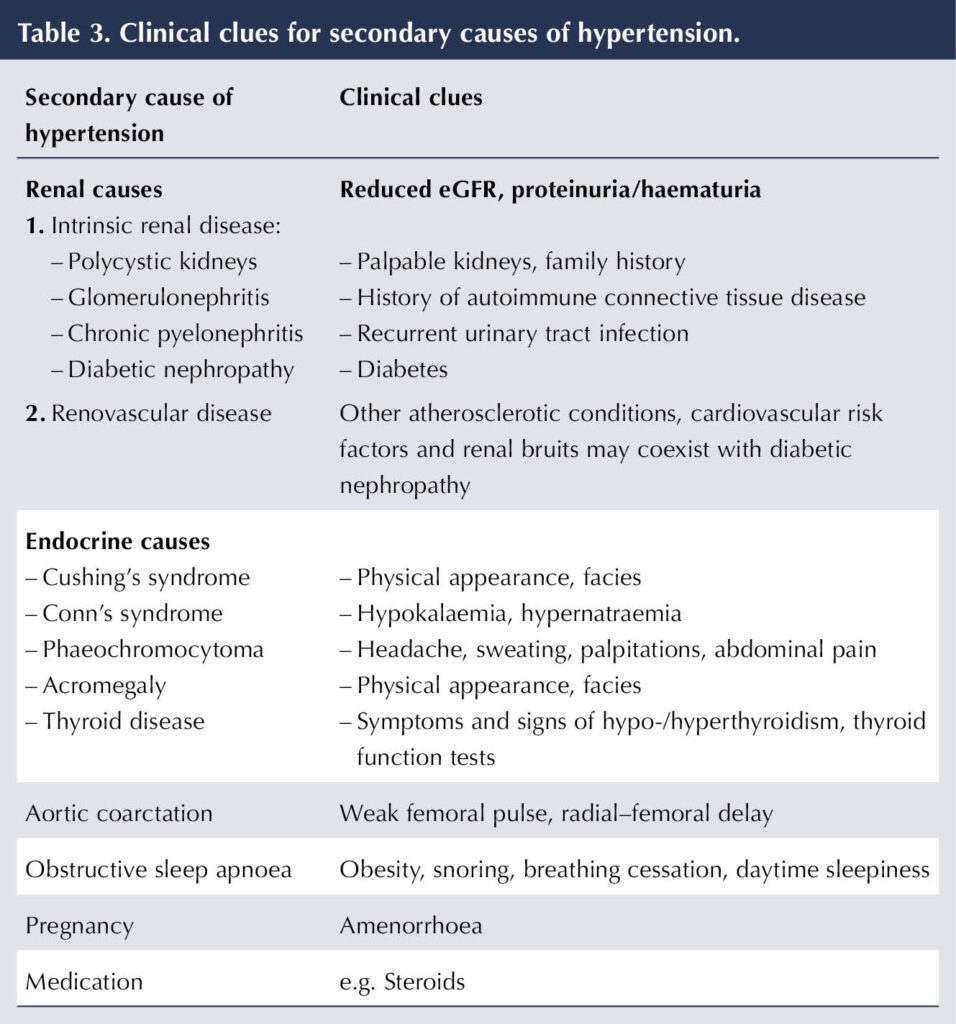
Secondary causes of hypertension
Whilst renal disease is a major complication arising in diabetes, diabetic kidney disease – quantified by eGFR and proteinuria – can itself drive hypertension. Rarely, there can be other secondary causes of hypertension in people with diabetes. Clues to their existence are outlined in Table 3. In adults aged <40 years, a secondary cause of hypertension is more likely, so further investigation and referral should be considered (NICE, 2023a).
Conclusion
Hypertension is a common finding in people with diabetes, and especially in those with type 2 diabetes. Accurate identification of hypertension is essential because of its association with macro- and microvascular complications of diabetes and mortality. Investigations for end-organ damage should be undertaken at the point of diagnosis of diabetes, and a cardiovascular risk assessment performed.
There is unequivocal evidence from randomised controlled trials that controlling BP to <140/90 mmHg in people with diabetes reduces the incidence of cardiovascular and microvascular complications. There may be additional gain from lowering BP to <130/80 mmHg to reduce the risk of stroke and complications from diabetic nephropathy and retinopathy, but these benefits need to be weighed against the increased risk of medication side effects. Targets should be individualised and, notably, a higher BP target of <150/90 mmHg is advised by NICE for people over the age of 80 years.






The risk factors and what might be done to address them.
24 Mar 2025