In April 2022, we published an article in this journal about Medway Community Healthcare’s (MCH) work to embed flash glucose monitoring within community nursing teams in order to support those in care/residential homes who rely on them for insulin administration. By providing flash glucose sensors to this cohort, the aims were to encourage patient autonomy while improving care quality and reducing insulin errors (Gregory and Curtis, 2022). This follow-up article summarises the successes and challenges from this ongoing work, and presents some of the data from the first year of implementation.
The Community Diabetes Team within MCH was one of the first to implement this technology in such a cohort, following the Diabetes Technology Network UK (DTN-UK) recommendations (Choudhary et al, 2021). Even more recent NICE guidance (NG28; 2022) recommends that flash glucose monitoring is offered to “adults with insulin-treated type 2 diabetes who would otherwise need help from a care worker or healthcare professional to monitor their blood glucose.”
It has taken time to embed this work to reduce reliance on an overburdened community nursing workforce. There is no quick fix – transforming services and embedding this change required a lot of process mapping and dedication, plus a commitment from many services to ensure that this work was not lost or buried. As with any innovation, embedding flash glucose monitoring (also known as intermittently scanned CGM) within community nursing teams – including those patients who are housebound or who live in residential care – was a challenge. Such challenges are not unique to the author’s place of work, as acknowledged by Leeson (2022).
The work has been hindered by workforce shortages, an increase in demand on both the specialist diabetes team and community nursing teams, and training of community nursing teams.
Community nursing workforce
As with many areas nationally, the crisis in staff shortages across the NHS is having an impact on the recruitment and retention of qualified staff within the author’s area of work. Rogers (2021) recognises that, despite increasing and complex caseloads, there has been little increase in staff resources, and there is growing concern about the health and well-being of community nurses. Within MCH – as in many other areas – community services are often on a “block contract”, meaning there are no limits on capacity or referrals. All community services have seen a rise in both numbers of referrals, and the complexity of referrals and patient care.
Community nursing well-being
There has been a general concern around staff well-being within the NHS, particularly during and after the COVID-19 pandemic (Doyle, 2021; Rogers, 2021), a concern that is reflected in the NHS Staff Survey (2021). The survey found that within MCH around 60% of staff were unable meet the conflicting demands on their time, and almost 31% were feeling burnout because of the work they do. This survey does not apply only to community nursing, but is a reflection on all staff working within an NHS organisation.
Leeson (2022) highlighted that shortages of staff often lead to an excess of patients requiring insulin administration at the same time, and it is not unusual to see mixed mealtime insulins given long before or after meals to manage the demand. This is certainly the case for those community nursing teams within MCH who often have multiple insulins to be administered at the same time. This is not helped by a lack of knowledge regarding the range of insulins, or an inadequate incentive or lack of time to help patients become independent in insulin administration.
Limited time for training/education
Because of increasing caseload and workload pressures, staff education and training has taken a back seat. Flexibility around training has, therefore, had to be key in this work. It is difficult to see the long-term impact of the project on a daily basis, when the clinical load is high. However, education and training were essential. Staff need to learn new skills and develop their competencies, as well as having access to clinical supervision (Doyle, 2021). Supporting staff and potentially reducing workload has a positive impact on the daily management of caseloads and helps with staff retention, which is important when community nursing has seen a steady decline in staff (Chamanga et al, 2020).
Despite these challenges, the community nursing teams have embraced this technology. It is because of clear leadership within the specialist and community services that this work has continued, even when it might have been easier to postpone it.
Mandatory READ training (Recognise deterioration; Escalate; Act; Document), which took place within MCH in 2022, was pivotal in turning these challenges around. It helped staff recognise that the use of technology would not only save them time, but was improving patient safety and allowing appropriate review of those patients who would otherwise have unequal access to technology and diabetes review. These study days were organised by community nursing leads and supported by Abbott (the manufacturer of the FreeStyle Libre – the only currently licensed flash device). It delivered the technology training, with the community diabetes team addressing the clinical impact of the device.
All staff were invited to wear a sensor and set up an account to manage in LibreView (the cloud-based system for storing and sharing FreeStyle Libre glucose data) in order to know how the sensor works and the impact it can make compared to once- or twice-daily blood glucose testing. Data was for personal use and was deleted afterwards. Confidence in applying and setting up a Libre was one of the biggest positive messages from the training. Sharing and demonstrating the data that was available helped teams to understand the short- and long-term impact of using the technology.
Since the community nursing and neighbourhood nursing teams have developed their knowledge and skills in this technology, over 90 patients have used the Freestyle Libre and, although no longer on the specialist nurse caseload, continue to use it as part of their routine diabetes management.
Addressing health inequalities
The position statement on ethnicity, deprivation and diabetes inequality from Diabetes UK (2022) opens with, “Diabetes does not affect everyone equally”. Inequalities due to poverty, ethnicity, imbalances of economic and political power, age and physical/mental well-being are all causes of poor health outcomes or access to treatment and technologies.
The main focus of the report is on social economic factors and ethnicity. It does not give much attention to those vulnerable people who also have difficulty accessing the right services – those who are housebound, are elderly and/or frail and rely on others, and those who cannot access technology because they do not have the latest phones or their services do not have adequate staff to support them with this technology.
There is often some healthcare professional bias or, perhaps, ignorance around the use of technology in some populations. Bias is the conscious or unconscious attitudes or beliefs held without proof (Hekmat-Panah, 2019), and which may lead to assumptions on user understanding and ability relating to the benefit of diabetes technology. Hekmat-Panah (2019), although not diabetes technology specific, argues that we should not ignore the power of science or technology to achieve the goals of better health, and that potential harm can be avoided by appropriate use of technology.
Addressing the gaps
The key to the success of embedding the technology for these vulnerable patient groups came from the leadership within the community diabetes specialist team, as well as community nursing teams. Working together, and providing specialist support and training, community nursing teams identified those who would benefit from the technology, as well as providing an opportunity for a more robust review of their insulin regimen and medication.
These patients were identified on a separate caseload overseen by a senior diabetes nurse, but primarily reviewed face to face by members of staff in bands 4 and 5. These people are not registered nurses, but have developed competencies within this area and are able and confident to gather information, provide education for patients and families/carers, and work with the community nursing teams to apply the sensor, if needed, and upload data. Any changes made were within the prescribing guidelines and were the responsibility of the prescriber within the community diabetes team.
Roles and responsibilities were made clear within the community teams, and a flow chart was developed to identify each step of using FreeStyle Libre, from patient assessment to potential discharge from the community diabetes team.
The caseload of these patients also included those discharged from hospital new to insulin, for whom it was felt a “baseline” of results was needed, as well as identifying many who could potentially stop insulin post illness.
Unfortunately, because of community nursing shortages, these specialist practitioners were asked to provide support with insulin administration during the peak of winter pressures and had little time, therefore, to work solely on the FreeStyle Libre caseload. Keeping up with the increase in referrals for insulin, while also reviewing those patients with the potential to stop or reduce their insulin, means that community nursing caseload numbers remain resistant to being reduced.
Data collection and impact of FreeStyle Libre
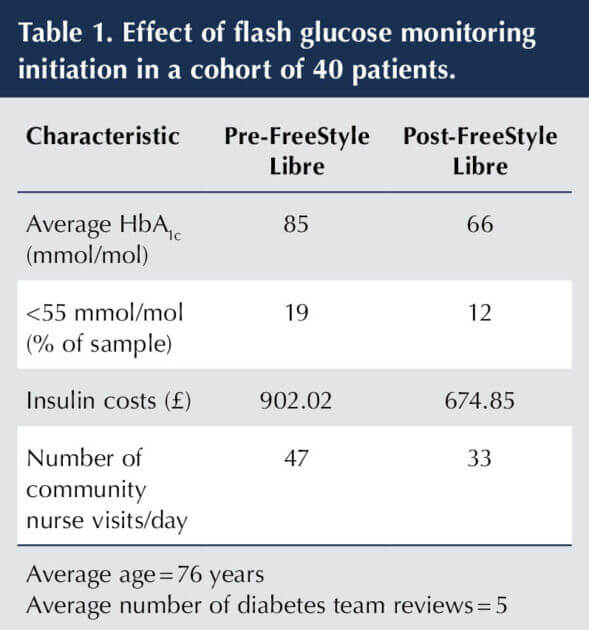
The data collection and analyses were carried out by the author, who is Clinical Lead for the Community Diabetes Team at MCH. The data was collected from the Freestyle Libre caseload for housebound patients, or those new to insulin needing education and support on discharge from hospital. The summary data in Table 1 shows the effects of FreeStyle Libre use on a number of parameters within the cohort.
Discussion of data
There are around 40 patients in the current cohort, including those on community nursing caseloads, in care or nursing homes, and new to insulin (discharge from hospital). This number fluctuates, depending on new referrals and those discharged.
Forty-eight people have been discharged from the caseload, either to manage their insulin and glucose monitoring independently, or to continue to be monitored by community nursing teams. Costs of community nursing visits were mentioned in the previous article (Gregory and Curtis, 2022), but within the author’s organisation (and as with many), community nursing services operate on “block contracts” – no financial savings are made by reducing or increasing caseloads in these contracts.
Out of these 48 patients, 12 have had their insulin stopped altogether. The main reason for stopping insulin was hypoglycaemia, associated with frailty and comorbidities (such as renal impairment or dementia). Insulin had generally been started in hospital, due to intermittently raised glucose levels when unwell, and had not been reviewed.
Insulin is likely to be required as a temporary choice for those people with type 2 diabetes who have severe hyperglycaemia (caused by infection or steroids), who have had a myocardial infarction or are post operative (Royal College of Nursing [RCN], 2022). However, when commencing insulin, consideration should be given to symptoms, ability to manage insulin, suitable insulin regimens and risk of hypoglycaemia.
A low HbA1c target (<53 mmol/mol) in a frail, elderly person increases their risk of hypoglycaemia (Ling et al, 2021), with age as a single risk factor impairing the adaptive response to hypoglycaemia (Selvin et al, 2021). Hypoglycaemia can lead to cognitive impairment that, in turn, leads to a higher risk of trips and falls, potentially resulting in hospital admissions owing to fractures (RCN, 2022).
Insulin administration following hospital discharge is the most common reason for referral to community nurses locally – either those new to insulin or those who can no longer self-administer since admission. An insulin regimen that is initiated or changed in hospital may not be practical on discharge, while some insulin choices will not be available (Cousins et al, 2011).
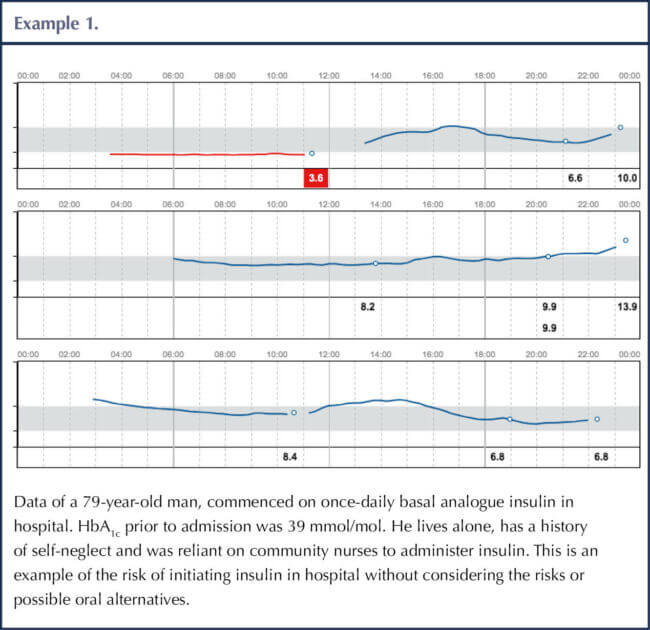
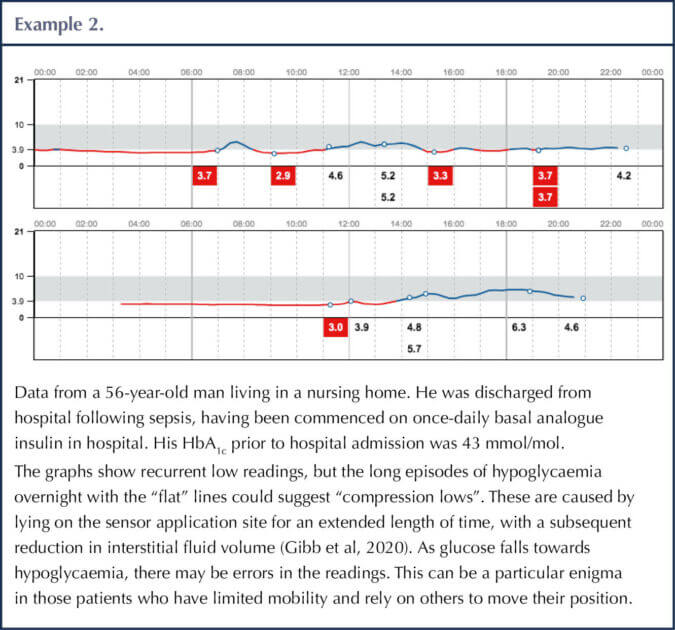
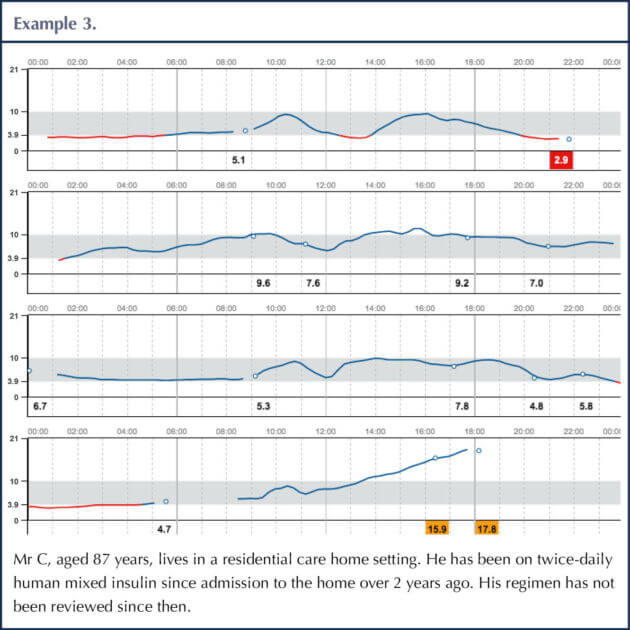
Twenty-three patients have had a change in the insulin regimen, primarily from a once-daily basal analogue insulin to either a once-daily isophane in the morning, or a mixed human insulin in the morning. Locally, many patients who are discharged from hospital are started on a once-daily basal insulin and, as discussed in the previous article, overnight hypos are not picked up owing to monitoring only taking place once a day.
Insulin requirements vary greatly after hospital discharge, depending on daily routine, diet and recovery. Such individuals therefore require frequent review and insulin adjustments to avoid hypoglycaemia after hospital discharge. If they are housebound or reliant on others to monitor their requirements, this adds to the burden on community caseloads.
Those patients for whom insulin was stopped continued on the FreeStyle Libre for up to 6 weeks to monitor the effect. They also had a final HbA1c test and a concise, clear plan for follow-up HbA1c within the community teams or via primary care.
When considering the data for this second article, we included the financial impact of changing or stopping insulin. Many patients are commenced on the more expensive basal or mixed insulins, when there may be safer, cheaper alternatives (particularly if relying on community nursing teams to administer them).
Although the aim of the work is not to reduce costs, this is a consequence of the appropriate review of insulin regimens, the safety around timing of insulin, and of not using the most costly insulin regimens available.
HbA1c was measured at the start of patients initiating FreeStyle Libre, and at the end of the review. We have not only seen an overall improvement in HbA1c, but the number at greatest risk of hypoglycaemia (with an HbA1c <55 mmol/mol) has reduced. At the start of the work, 1 in 5 of those patients had an HbA1c <55 mmol/mol, putting them at real risk of hypoglycaemia. Hypoglycaemia often goes unnoticed on a once-daily insulin as, by the time the insulin is administered, many patients have already had their meal, so the glucose appears to be within range.
The three examples shown within this article are representative of the data being provided, and the most common risks around insulin initiation, administration and review of regimens.
Next steps
The process of embedding FreeStyle Libre into community nursing is well underway, and is now regarded as the safe and cost-effective way of monitoring glucose levels, as outlined in the DTN-UK and NICE guidelines. Community nursing teams are receiving support from the diabetes specialist team for clinical reviews, and training and education support from Abbott.
Band 3–5 diabetes support workers and educators are an integral part of the diabetes specialist team. They work across the specialist and community nurse teams to review and educate patients on FreeStyle Libre, identifying patients who need diabetes specialist nurse support in monitoring and changing their insulin regimens.
Once the support workers and educators are fully established, the community teams within MCH will review those patients in care homes, initiating and supporting the delegation of insulin programmes.
A review of insulin administration documentation is being carried out with the pharmacy lead and community nursing leads, to enhance the recording of insulin administration. Because most documentation is still kept within the patients’ homes, and not always on electronic records, making adjustments can be difficult and unsafe (Leeson, 2022).
There is a real need for the community team to continue to liaise and work with the specialist diabetes team within our local secondary care service. Although secondary care and in-patient care provides a wide range of learning opportunities for junior doctors, their knowledge of diabetes and insulin regimens can be limited, and they may often use the insulin they are most familiar with (Pichardo-Lowden et al, 2017), as medical education around diabetes is so varied. Patients may not always have been reviewed by the in-patient diabetes team, depending on the day of admission and length of stay.






Quick links to the best resources, publications and research for all nurses with an interest in diabetes.
20 Jun 2025