An increasing number of people need support to manage their diabetes. This can be because of other conditions, such as dementia and arthritis, that affect their ability to self-care, or to circumstances, such as living in a care home and relying on community nursing teams to deliver insulin (Evans et al, 2021; Trend Diabetes, 2021). Many such people have a once-daily insulin regimen, as there has been a focus on analogue basal insulins to attempt to reduce the burden of care (Evans et al, 2021), and it is often believed that these insulins are more stable and safer to use in this cohort – even though a lack of glucose monitoring can make dose adjustment challenging.
The community nursing workforce is already under pressure, with the planned number of registered nurses below target for 40% of nursing shifts (Senek et al, 2020). In the authors’ location, the number relying on community teams to administer insulin has increased significantly. This can impact on the quality of care and would be compounded by asking for more visits to monitor blood glucose to be made.
This article outlines the process that Medway Community Healthcare (MCH) implemented in order to use flash glucose monitoring (FreeStyle Libre) in those who rely on community nursing teams for insulin administration.
MCH has 19 community and neighbourhood nursing teams, covering a total of 46 GP surgeries, and is commissioned by the CCGs to provide a service, including the administration of insulin, to those patients who are housebound. Most patients are either on a once-daily or twice-daily insulin regimen, with blood glucose levels only being checked at time of insulin administration.
MCH is currently undertaking a transformation project to align the Buurtzorg principles of nursing (www.buurtzorg.com) to the community teams. MCH has been involved in Transforming Integrated Care in the Community (TICC) since 2018, with the aim of creating teams that are nurse-led, self-directed and non-hierarchical.
TICC is about promoting nursing teams to be autonomous practitioners, with an approach to care that looks at the person as a whole and moves away from “tasks”. Adopting the view that clinicians build trusting relationships with patients enables the patient to take ownership of their own care and feel that they are involved. It also gives teams the potential to increase their workforce, providing a better work–life balance, a reduction in caseload numbers and enabling the provision to be about the patient and safe, quality care.
The teams are supported by locality coaches, to encourage staff to look at healthcare from “outside the box”, enabling patients to be concordant with their care plan and the experts in their own care – a model well suited to those living with diabetes.
Changing demands during the pandemic
During the current COVID-19 pandemic, there has been an increase in people being discharged from hospital newly diagnosed with diabetes and/or new to insulin, and relying on community nursing teams to administer insulin and to monitor glucose levels. This workforce is struggling with the demands of trying to balance patient safety and timing insulin administration correctly with the provision of high-quality visits that are not rushed, but which should be considered high risk.
Two recent reviews of community nursing caseloads have similar findings – many patients who have sporadic or limited blood glucose monitoring often experience episodes of hypoglycaemia between community nursing visits, which often go unidentified (Gregory, 2019; Rowney and Lipscomb, 2019). The use of a once-daily basal analogue insulin did not reduce the number of hypoglycaemic events.
Identification of problem
In January 2021, during the peak of the second wave of the COVID-19 pandemic, the community nursing teams within MCH were supported with insulin administration by other specialist teams, including the community diabetes team. It was during this time that it was highlighted that the reviews of these patients were inconsistent and scant, and many were having insulin administered at varying times, not always within the recommended timings. Many had not had a medication review or annual review, so care planning and target setting were not in place, and community nursing teams were very much working to a task model.
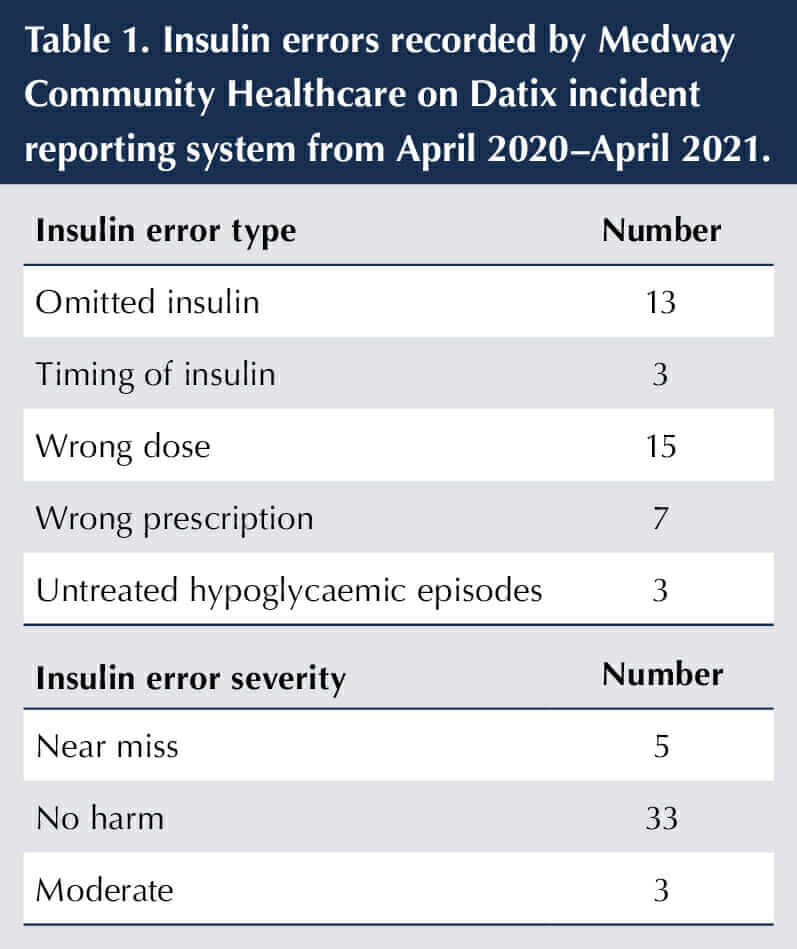
A Datix report for insulin errors was generated to include inappropriate timing, omitted or missed insulin, wrong dose given, poor prescription and incorrect needle use. Table 1 shows the number of reported insulin errors, but this is probably an under-representation, particularly around timing of insulin administration.
The cost of these teams administering insulin is open for debate – many teams are commissioned on a block contract. However, if we were to cost each visit at £31.25 per visit (excluding petrol costs), this equates to £11,406.25 per annum (Goodman et al, 2017). At the time of writing, there were a total of 102 visits for insulin administration per day, which, following Goodman’s calculations, would total £3,187 per day.
However much the financial cost to the organisation and workforce, the biggest implication is that of patient safety – maintaining standards when administering a high-risk drug, such as insulin, and the practicalities of administering it in a timely manner with an overstretched workforce.
There have been three incidents reported in Datix of hypoglycaemic episodes that were untreated. The incidence of hypoglycaemia is difficult to assess in any community caseload because of the frequency of blood glucose testing – it is usually carried out only at the time of insulin administration, which may only be once daily, and varies between pre-meal and post-prandial testing. This not only increases the risk of hypoglycaemia, but also makes insulin adjustment challenging as HbA1c tests are also scant and do not always give a true picture of glycaemic control on a daily basis.
The work carried out in other areas was set to be duplicated within MCH, with the aim of embedding flash technology within the community nursing service. The diabetes service approached Abbott, the manufacturer of FreeStyle Libre (the only currently licensed flash device), for initial support and to discuss the use of the sensors in this population. MCH purchased five sensors to trial within a particular team but, with Diabetes Technology Network (DTN-UK) recommendations being published in June 2021 (Choudhary et al, 2021), the team felt that this was an opportunity to use flash glucose monitoring in the people for whom “insulin administration or glucose monitoring must be undertaken by a third party”. These guidelines have been endorsed by Diabetes UK and are now in the draft NICE guidelines on flash and continuous glucose monitoring.
The Diabetes Team also set up virtual training for community nursing teams – and, indeed, anybody who was working with patients. To ensure a high-quality, patient-focused service, the workforce needed to understand diabetes, and have the knowledge and competence to administer insulin, coming away from the traditional “task” model.
A 10-point training was developed by Ruth Miller (Diabetes Consultant Nurse) to deliver the key points of diabetes care within a particular setting – in this case, the community. It can be delivered face-to-face or virtually; for the purpose of the work in Medway, it was delivered virtually by the diabetes team to give all staff the baseline requirements for managing those patients with diabetes. It is now part of the induction programme for all new starters.
A small cohort of staff also attended a national programme (CARES), which was adapted for the community teams in Medway to give those staff an enhanced knowledge, and those “link” staff who potentially could take the FreeStyle Libre work forward were identified.
This training has been delivered in conjunction with Abbott, in a similar way to how they provide patient webinars currently. This has led to stronger links between the community nursing leads, and to the wider community teams developing a process of education that can be easily attended, whilst being supported by the diabetes team.
Initial findings
A small neighbourhood nursing team took part in the first phase of the work. Five patients, who were identified as having the potential to benefit from the sensor, agreed to it being applied and to their data being uploaded. These data were jointly reviewed with the diabetes team providing education and support to those staff, as well as advice on care planning and target setting.
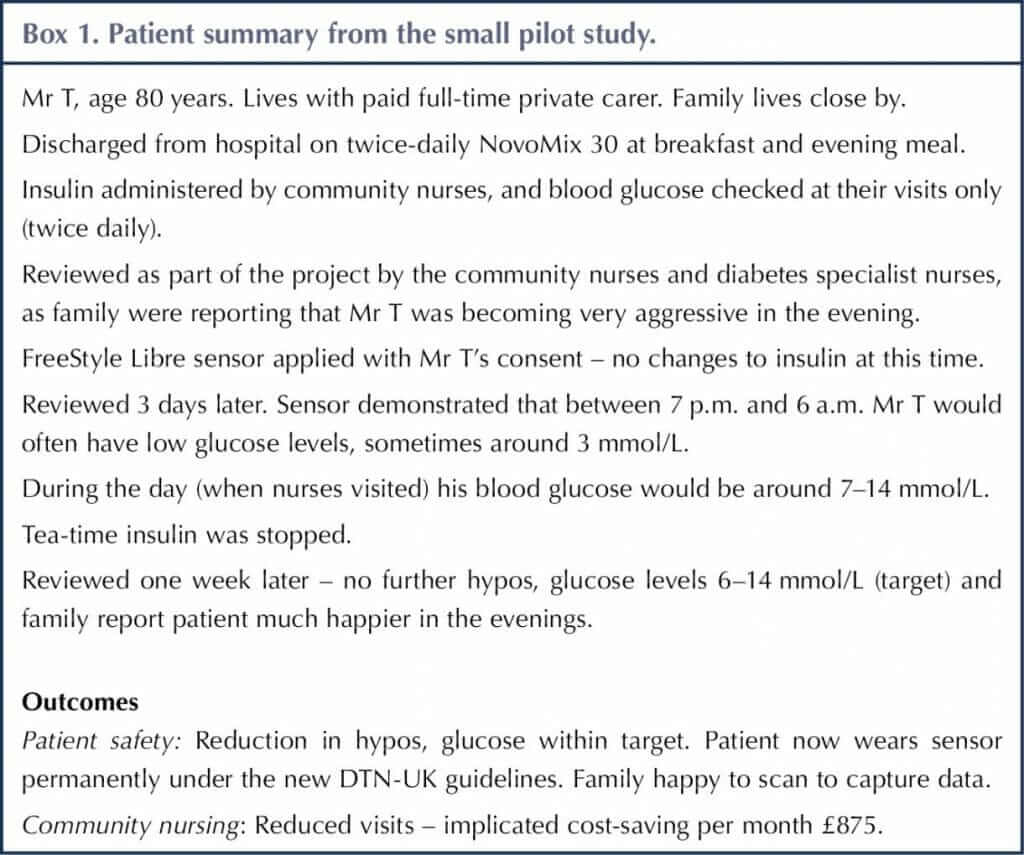
Of the five patients, three were found to have had at least one episode of hypoglycaemia during a 24-hour period, and at times when neighbourhood nurses would not have been monitoring their blood glucose (particularly overnight). A summary for one participant is shown in Box 1.
Embedding technology into community nursing
The success of this small, five-patient cohort confirmed outcomes from previous studies – that is, that many patients are at risk of hypoglycaemia when they cannot monitor their own glucose levels, leaving them vulnerable and at risk of admission to hospital. We worked very closely with Abbott, who supported our work and have since helped with account set-ups and ongoing training.
When the data was shared with senior managers and other community nursing teams, interest in the technology grew very quickly. At the time of writing, the number of patients on the FreeStyle Libre is 22 – just under one third of the total who rely on the community nursing teams for insulin administration.
The demands for the sensor – all based on clinical need and the DTN-UK guidelines (Choudhary et al, 2021) – meant that the diabetes team could not physically review each patient. The training programme, therefore, was key to the project’s success. There was some “hand-holding” to encourage confidence in the technology, as well as troubleshooting, before eventually the skills to upload the data directly to the clinic code were acquired.
Many community nurses are not familiar with flash technology. In time, however, it will become part of diabetes care, reducing risk and enabling some patients to manage their diabetes by giving them confidence in self-adjustment and self-monitoring.
Support for the project from the Executive Board was key. It meant that clinicians, who were assessing the patients, were supported to review and change their practice with very little red tape for what is a large undertaking.
Process
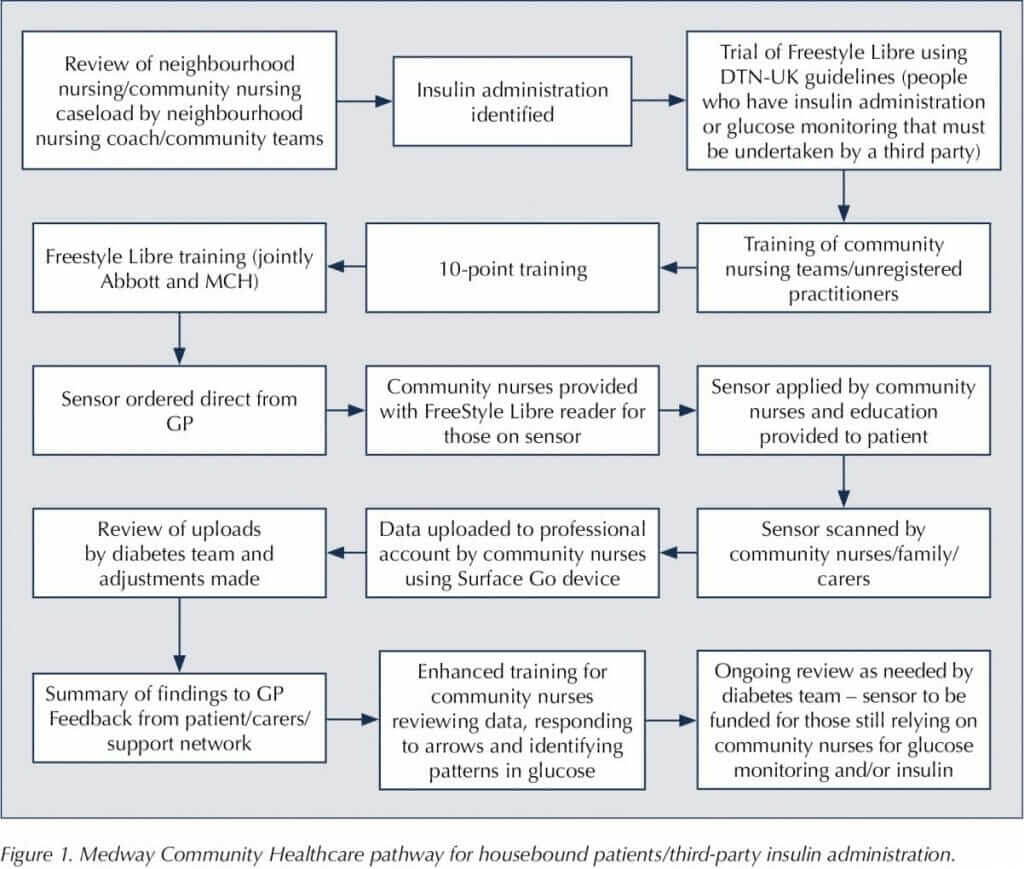
Following feedback from community nursing teams and practicalities around uploading data, the process went through several changes. It is now in a simple form, so that community nursing teams are able to identify those individuals who meet the criteria, and the diabetes team are still the primary HCPs in the management of the sensor and data (Figure 1).
Challenges
As with any major change to ways of working, there were challenges. This is a big piece of work to implement across a whole community service. There are always valid reasons to delay such work – staff shortages (and ensuring adequate skill mix), IT support, and time to explain the process to patients and their families and/or carers. As leads for the diabetes and community nursing teams, we felt that we could not delay implementation – patient safety was a priority, and adequate reviews of insulin regimens and glucose monitoring relied on having the technology to make them safe and robust.
It had already been identified that there were issues with insulin timing, because of the number of patients relying on community nurses to administer it, and the limited time to do what was seen as a “task” safely and effectively.
IT support should not be overlooked when implementing such a large change – the IT systems used by community teams need to support uploading of data and the recording of reports. The IT lead for MCH proved invaluable throughout the process.
Summary
There is little doubt that using the FreeStyle Libre sensor in its most basic capacity has not only allowed safer practice within community nursing teams when administering insulin, but has the potential to reduce the number of people on insulin as they can now be reviewed properly. Flash glucose monitoring will continue to be embedded within the teams, so that it becomes “standard” care for those who are vulnerable and rely on others to keep them safe.
Housebound patients often “slip through the net” – not intentionally, but because of a poor discharge process or communication, and no one person or team taking overall responsibility for their diabetes medication review, glucose monitoring, and subsequent care planning and target setting.
The new NICE draft guidelines are reviewing the way glucose levels are monitored. In these high-risk groups, the authors would argue that the only safe and effective way of carrying out a review of an insulin regimen is by having several glucose readings a day. Without flash glucose monitoring this is not achievable for most community nursing teams.
The insulin errors reported represent a drop in the ocean. The timing of insulin administration is a challenge when the community nurses have so many patients. Hence, it is very much seen as a task, rather than an opportunity to review the insulin being administered.
Encouraging patient autonomy and potential self care is more achievable using flash glucose monitoring. It gives the patient and family more confidence and provides those HCPs responsible for their care with a full picture, rather than a snapshot.
The success of the model has relied heavily on stakeholder involvement – community nursing teams, the community diabetes specialist team, the executive team within MCH, and residential and care home staff – and will be used as an example of good practice to the CCG.






Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024