Type 1 diabetes is a lifelong autoimmune condition requiring insulin therapy to manage glucose levels (Holt, 2021). Technologies such as continuous glucose monitoring (CGM) and hybrid closed-loop (HCL) systems have transformed diabetes care by improving glycaemic outcomes and providing real-time data to support medication optimisation (Battelino et al 2019; Sherr et al, 2022). Their use is expanding across the NHS and, owing to the recent update to Saving Babies’ Lives, they are becoming more common in antenatal care (NHS England, 2024).
Methods
Design
This service evaluation aimed to explore the confidence levels of registered nurses and midwives in the UK in the use of CGM and HCL technologies within their clinical practice. Approved by University Hospitals of North Midlands (UHNM), the project did not require ethical approval under Health Research Authority (HRA) guidance, as it involved no randomisation or changes to clinical care (HRA, 2023).
Data collection
An anonymous online questionnaire was distributed in May 2025 via professional social media channels, targeting registered nurses and midwives involved in diabetes care in the UK. The survey was developed by diabetes specialist nurses (DSNs), reviewed by peers, and piloted with 10 multidisciplinary team (MDT) professionals for clarity and relevance. It included multiple-choice, Likert-scale and open-ended questions covering:
- Confidence in CGM and HCL.
- Education and training received.
- Perceived safety and workload impact.
- Organisational support.
Responses were collected via Microsoft Forms and stored securely in line with local organisation policy. No personal data were collected. Data will be retained for 2 years for service development purposes before secure deletion.
Data analysis
Quantitative data were summarised as frequencies and percentages using Microsoft Excel. Likert responses were grouped into “confident”, “neutral” and “unconfident” for reporting. Free-text responses were thematically analysed by two reviewers. No inferential statistics were applied owing to the exploratory nature of the evaluation.
Results
Confidence in using CGM and HCL systems across staff groups
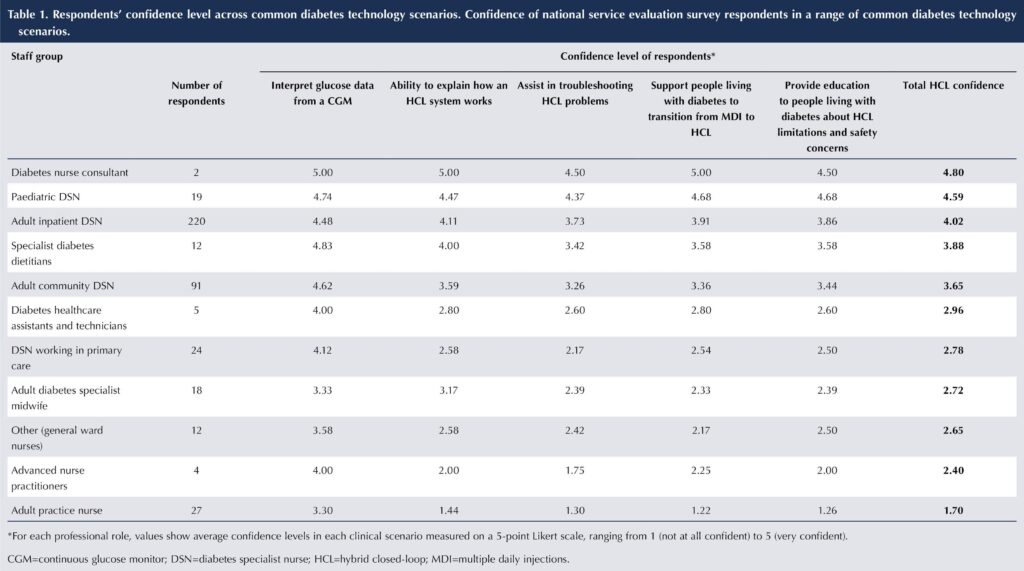
A total of 434 responses were received across the four home nations. Table 1 presents average confidence scores reported by nurses and allied health professionals in supporting people living with diabetes using CGM and HCL systems, grouped by professional role. Confidence was rated on a 5-point Likert scale, ranging from 1 (not at all confident) to 5 (very confident).
Average confidence in CGM and HCL by staff group
Table 1 highlights a clear role-based divide, with confidence linked to exposure to diabetes technology. CGM is more established in both primary care and secondary care practice, whereas HCL remains less familiar despite national policy support. These findings emphasise the need for targeted training, especially in non-specialist and maternity settings, to ensure safe and equitable technology-supported care.
Confidence by role
Adult diabetes nurse consultants
Nurse consultants reported the highest confidence (CGM, 5.00; HCL, 4.50–5.00), reflecting their advanced expertise and leadership roles. Though a small group (n=2), they often provide key points of support within organisations.
Paediatric DSNs
Paediatric DSNs (n=19) also reported very high confidence (CGM, 4.74; HCL, 4.37–4.74), attributed to early adoption of technology and structured training embedded in paediatric care pathways.
Adult inpatient DSNs
The largest respondent group (n=220), inpatient DSNs, showed high confidence (CGM, 4.48; HCL, 3.73–4.48). While many expressed confidence, several inpatient DSNs raised concerns about limited responses to training for HCL systems. This is often restricted to pump-specific nurses, reducing broader team exposure. They also highlighted a lack of understanding among ward nurses, which further impacts safe and effective care.
Adult community DSNs
The second largest respondent group, adult community DSNs (n=91), reported adequate confidence levels in managing diabetes technologies. Their average confidence score for CGM was relatively high at 4.62, reflecting strong familiarity and competence with this aspect of care. In contrast, confidence scores for HCL systems were more moderate, ranging from 3.26 to 3.59 across different aspects, suggesting a need for further training and experience in this area. These findings indicate a solid foundation in CGM use within community settings, with an opportunity to strengthen skills and support around the more advanced HCL systems.
Diabetes specialist dietitians
Although dietitians were not specifically invited to respond, some chose to share their insights (n=12). They reported strong confidence in using CGM (average score 4.83) and moderate confidence with HCL systems (ranging from 3.42 to 3.88), particularly in the context of patient education. However, some highlighted gaps in their ability to troubleshoot device-related issues and expressed a need for more hands-on, practical training.
Diabetes specialist midwives
Diabetes specialist midwives reported the lowest confidence of the specialist MDT (CGM, 3.33; HCL, 2.39–3.17). Respondents described anxiety, limited training and a lack of antenatal protocols. This is particularly concerning given national policy promoting HCL in pregnancy. The qualitative responses showed many relied on people living with diabetes or diabetes nurse teams for troubleshooting. These findings reinforce the urgent need for maternity-specific training and clearer multidisciplinary guidance.
Adult primary care DSNs
The confidence levels reported by DSNs working in primary care were mixed (CGM, 4.12; HCL, 2.17–2.58). Many felt unprepared to interpret CGM data or support HCL use, noting it was often seen as secondary care-led, rather than shared care. Despite this, there was strong interest in training and clearer referral pathways to enhance their role in integrated care.
Advanced clinical practitioners
The advanced clinical practitioner (ACP) role is typically associated with general practice or emergency care, making it challenging to determine the specific settings of the respondents in this group, all of whom were nurses (n=4). They reported relatively high levels of confidence with CGM (4.0), but notably low confidence with HCL systems (ranging from 1.75 to 2.25). This suggests limited exposure or training in more advanced diabetes technologies within their current roles.
Practice nurses
Practice nurses (n=27), who work within primary care settings, reported moderate confidence with CGM (average score 3.3), but very low confidence with HCL systems (ranging from 1.22 to 1.44). As they are often the first point of contact for people with diabetes attending GP surgeries, it is essential they have clear guidance on how to respond in emergencies, manage sick days and provide basic troubleshooting support. These results highlight a critical need for targeted training and accessible resources to support practice nurses in safely managing patients using diabetes technology.
Implications for training and safety
These findings reveal a mismatch between confidence and structured training. While overall confidence in diabetes technology was high, particularly among inpatient, paediatric and consultant nurses, it was notably lower among midwives and primary care teams. This variation poses risks to safe, consistent care, especially in maternity and community settings.
As CGM and HCL technologies rapidly become standard across the NHS, formal preparation must match this pace. The receipt of formal training in CGM was reported by 73.5% of respondents, while 57.6% had received it in HCL technologies. Although these figures are encouraging, free-text responses suggest that the quality, depth and consistency of training vary considerably. Many staff rely on peer support or industry medical-device representatives, rather than structured, NHS-led programmes. Without accessible, role-specific training embedded across services, inconsistencies in practice and technology-related safety risks may persist.
Organisation support and adequate funding
The survey explored perceptions of workload, and time, funding and resource availability associated with the implementation of HCL systems. Overall, the introduction of HCL has had a marked impact on clinical workload. Respondents reported an average score of 4.05 (on a 5-point scale, where 5 represented “significantly increased”), indicating that most healthcare professionals have experienced a notable rise in workload since HCL became more widely adopted.
When asked whether they had sufficient time during routine appointments to support people using HCL, the average score was 2.67, suggesting that many respondents do not feel adequately resourced in terms of time. This mismatch between workload and available time likely contributes to the broader pressures faced by diabetes teams, particularly when trying to offer equitable care across diverse patient populations.
Funding was also identified as a key challenge. Respondents rated the adequacy of funding for the additional time required to support HCL with an average score of 2.27, and the organisational provision of resources to support HCL implementation scored 2.44. Both scores fall below the midpoint of the scale, reflecting widespread concern about the lack of financial and structural support within organisations. This aligns with qualitative comments calling for improved admin support, better training pathways and fairer funding models across Integrated Care Boards (ICBs).
Together, these findings suggest that while the clinical benefits of HCL are widely recognised, the infrastructure and investment needed to support its safe and sustainable implementation remain inadequate across many parts of the UK.
Key themes from free-text comments
Survey respondents shared a wide range of insights highlighting significant challenges and opportunities in the implementation of hybrid closed-loop (HCL) systems. A dominant theme was the widespread issue of insufficient staffing, with many teams at or beyond capacity and lacking dedicated administrative support to manage the increased workload.
Training gaps were also evident, particularly for ward staff and inpatient teams, with limited opportunities for upskilling or shadowing. Respondents raised serious concerns about inconsistent funding processes across Integrated Care Boards (ICBs), contributing to a postcode lottery in patient access and audit participation. Despite these systemic issues, many reported that HCL has been life-changing for patients, improving quality of life and reducing the burden of diabetes management. However, services are struggling to maintain broader care provision due to the resource demands of HCL rollout.
Equity concerns were frequently mentioned, particularly for patients with language barriers, digital poverty or additional vulnerabilities. Technology-related issues, such as inconsistent device compatibility, brand-specific terminology and limited IT infrastructure, further complicated implementation.
Emotional strain and burnout among staff were also reported, with some nurses considering leaving the specialty due to lack of support and escalating patient expectations. Collectively, the responses emphasised an urgent need for a national strategy that includes equitable funding, workforce investment, consistent guidance and greater inclusion of diabetes specialist nurses in planning and policy decisions.
Discussion
This national service evaluation highlights encouraging levels of confidence among many UK nurses and midwives in supporting CGM and HCL use, but also reveals persistent disparities in preparedness and support across clinical roles and settings. Confidence in CGM was high (86.6%), reflecting its more established integration into clinical practice. However, confidence in HCL was lower and more variable (65.2%), particularly among midwives and primary care teams, groups crucial to the success of widespread technology adoption.
Although more than half of respondents had received formal training in CGM (73.5%) and HCL (57.6%), the quality and consistency of this training remains a concern. Many professionals continue to rely on informal peer learning or industry-led sessions, rather than structured, NHS-endorsed programmes. This creates a concerning gap between perceived confidence and actual competence, especially in complex or high-risk scenarios, such as pregnancy. The gap between informal learning and clinical expectations suggests an urgent need to review how diabetes technology is addressed in both pre- and post-registration education.
Midwives were the least confident specialist group overall, despite national mandates promoting HCL for eligible pregnant women (NICE, 2023; NHS England, 2024). This lack of confidence is compounded by insufficient antenatal guidance and reliance on patients or specialist teams for device troubleshooting. It emphasises the urgent need for targeted, maternity-specific training and multidisciplinary collaboration to deliver safe, technology-supported antenatal care. This mirrors earlier challenges with insulin pump rollout, where inadequate staff training contributed to variation in uptake and outcomes (National Diabetes Audit, 2017). To avoid repeating this pattern, HCL deployment must be paired with coordinated education, clinical governance and workforce monitoring.
Workforce strain was another dominant theme. The majority of respondents reported increased workload due to HCL implementation, with average ratings indicating that most do not have sufficient time or funding to meet the associated demands. This aligns with qualitative feedback describing unsustainable pressure, rising patient expectations and a lack of administrative support. Notably, some respondents reported burnout and an intent to leave diabetes care altogether, raising concerns about staff retention at a critical time of technological transition.
Equity also emerged as a major issue not only for people with diabetes, but also for healthcare professionals. Staff working in under-resourced settings are less likely to have access to training, mentorship or clinical protocols. Postcode variation in ICB policies further exacerbates this, creating inconsistent access to funding and support across regions.
While the clinical value of HCL is widely acknowledged, many describing it as a “game changer” for patients, the infrastructure to support its rollout remains fragile. The success of NICE TA943 (NICE, 2023) and similar initiatives depends not only on device availability, but on preparing the workforce to use these technologies safely, confidently and equitably. This evaluation highlights the need for national investment in training, role-specific protocols, clear escalation pathways and stronger clinical governance. Without these, the promise of digital diabetes care risks being undermined by gaps in preparation, inequity and staff exhaustion.
Addressing health inequalities
Technology-driven care must not deepen existing disparities. The National Diabetes Audit (2021–22) documents lower uptake of diabetes technology among people from ethnic minority and socioeconomically deprived backgrounds. Without targeted investment, the digital transformation of diabetes care risks leaving behind both people living with diabetes and professionals.
Saving Babies’ Lives
The AiDAPT trial provides strong evidence for HCL in pregnancy, showing improved glycaemic outcomes and reduced maternal weight gain without increased hypoglycaemia (Lee et al, 2024; Buschur et al, 2025). National guidance now supports its use in antenatal care, yet this ambition is not matched by workforce preparedness. Midwives in this evaluation reported low confidence, limited training and inconsistent access to antenatal protocols. Without urgent investment in maternity education and structured support, national targets risk falling short in practice.
Implications for practice and policy
To ensure the safe and equitable implementation of CGM and HCL systems, we recommend the following national and local actions:
- National training programme. Commission a standardised, accredited training framework for all nurses and midwives likely to encounter CGM or HCL. This should combine e-learning, simulation and supervised practice. Stakeholders, such as the DSN Forum UK, TREND-UK and NHS England, should lead its development and delivery.
- Standardised clinical protocols. Implement evidence-based protocols across inpatient, community and maternity care, aligned with NICE TA943. Clear escalation pathways must be included to support non-specialist staff.
- Digital diabetes champions. Fund named leads in each Trust or Integrated Care System to provide local expertise, troubleshooting and staff support, linked through national peer networks.
- Safety monitoring. Establish a national system to track technology-related safety incidents and share learning. Local audit should feed into national thematic reviews to inform policy and improvement.
- Curriculum integration. Embed diabetes technology education into nursing, midwifery and allied health undergraduate and postgraduate programmes to prepare the future workforce.
- Equity and co-design. Involve people with diabetes in designing education and care pathways. Conduct equity audits to monitor access and prevent disparities in CGM and HCL uptake.
- Maternity workforce investment. Prioritise HCL-specific training for midwives, including antenatal protocols, emergency planning and interprofessional support. This is essential to meet national policy expectations and safely implement technology in pregnancy.
If frontline staff are expected to deliver increasingly complex diabetes care, they must be supported by robust infrastructure, training, protocols, escalation routes, and leadership. Without this foundation, confidence and safety will remain fragile.
Limitations
This evaluation has several limitations. The use of a convenience sample distributed via social media may have introduced selection bias, favouring those with strong views or experiences related to diabetes technology. As a self-reported survey, responses may also reflect response bias – either over- or underestimating confidence and training.
While the questionnaire was reviewed for content validity, it was not psychometrically validated. The lack of detailed demographic data (e.g. clinical banding, years of experience and ethnicity) limits subgroup analysis. Participation from Scotland and Northern Ireland was lower, which may reflect the absence of a national HCL rollout in those regions. However, other factors, such as recruitment reach, may also have contributed.
No inferential statistics or longitudinal follow-up were conducted, so causal conclusions cannot be drawn. Nonetheless, the consistency of responses across varied roles and settings supports the relevance of the findings and their implications for workforce development.
Conclusion
This national service evaluation highlights a growing confidence among UK nurses and midwives in supporting people with diabetes using CGM and, to a lesser extent, HCL systems. Whilst the widespread adoption of CGM is now underpinned by relatively high staff confidence and training access, HCL implementation remains inconsistent, particularly outside of specialist diabetes teams.
The findings underscore a critical gap between the NHS’s ambitions for digital transformation in diabetes care and the preparedness of the nursing and midwifery workforce tasked to deliver it. Confidence in HCL was lowest among midwives and those working in primary care. These groups often lack structured training, protocols and access to escalation pathways, despite being at the frontline of patient care.
Workforce strain was a major concern, with many professionals reporting increased workload, limited administrative support, and a lack of time and funding to deliver the education and follow-up required for safe HCL use. This pressure, coupled with disparities in training access and regional funding models, risks undermining the equitable implementation of NICE TA943 and other national initiatives.
To realise the full benefits of CGM and HCL technology, workforce development must be prioritised. This includes investment in formal training, standardised clinical protocols, digital diabetes leadership roles and inclusive support strategies that account for equity and resource variation. Confidence alone is not enough; competence, supported by system-wide infrastructure and policy, is essential to ensure that advanced diabetes technology can be implemented safely, sustainably and equitably across all areas of care.
Future research
Further research is needed to evaluate the impact of structured workforce training on people living with diabetes outcomes, and staff confidence in using CGM and HCL systems. Prospective studies examining insulin error rates, near-miss events and technology-related incidents, before and after training interventions, would provide valuable insights. Qualitative research should also explore the lived experiences of midwives, primary care staff and generalist inpatient nurses, focusing on the challenges they face and the support they need to deliver safe, technology-enabled care. A particular priority should be understanding the needs of maternity services, where policy ambition is high, but workforce readiness remains low.
Acknowledgements
We thank all participating registered nurses and midwives for their time and honesty. The evaluation was conducted in accordance with HRA guidelines as a service evaluation and did not require ethical approval.






Developments that will impact your practice.
29 Aug 2025