UK nutrition guidelines for people with diabetes emphasise an individualised approach to dietary management, with low-carbohydrate diets being recommended as an option since 2011 (Dyson et al, 2011; 2018). A recent position statement from the British Dietetic Association (2018) draws the same conclusions.
The aim of this study was to explore the views and practices of UK Registered Dietitians (RDs) regarding dietary carbohydrate restriction as a management strategy for adults with type 2 diabetes. The results will further inform the debate within the dietetics profession and beyond concerning the appropriateness of this dietary intervention, and will provide insight as to how patients can be best supported to follow a low-carbohydrate diet.
Methods
This qualitative study used electronic questionnaires to collect data from RDs with clinical experience in type 2 diabetes management. Data were analysed using summative content analysis (Hsieh and Shannon, 2005). Bradford Teaching Hospitals NHS Foundation Trust acted as a sponsor for this study. Health Research Authority (HRA) approval was granted for this study (REC reference: 18/HRA/0014). Further ethical approval was not required for this study.
Subjects and sampling
Convenience sampling was used to access participants for this study. Eligible participants were RDs with clinical experience in managing adults with type 2 diabetes. Those who were ineligible included dietitians not registered to practise in the UK and RDs who only offered general dietary advice to adults with type 2 diabetes in group settings. RDs who were employed by the study sponsor (Bradford Teaching Hospitals NHS Foundation Trust) were also excluded.
Study invitations were sent to 340 members of the British Dietetic Association’s Specialist Diabetes Group via email. Participants confirmed that they met the eligibility criteria and gave their voluntary and informed consent to participate in the study prior to questionnaire completion. No incentives were offered to participants.
Survey design and administration
A pilot questionnaire was designed based on discussions in current literature (van Wyk et al, 2016; McArdle et al, 2017; Dyson et al, 2018; Huntriss et al, 2018), and sent to Specialist Diabetes Dietitians at Bradford Teaching Hospitals NHS Foundation Trust. Following a review of the process and questions, a final version of the questionnaire was agreed by the authors. The final version of the questionnaire was sent to participants via SurveyMonkey in May 2017.
The open-ended questions were developed with no pre-judgement and there were no leading questions. Participants could respond in free text to the questions. The questionnaire was available to complete for three weeks, as was communicated in the participant information sheet. No data were collected after this point.
Data analysis
Data were analysed using summative content analysis. This involves counting and comparing keywords or content (Hsieh et al, 2005). This act of assigning numerical values to a set of data may be used to quantify both manifest and latent content. Manifest content is evidence that is directly seen, such as the words written down in response to questions asked. Latent content refers to the underlying meaning of content, such as the interpretation of the answers to the questionnaire. This methodology is commonly used to analyse open-ended survey questions (McKenna et al, 2017).
Each completed questionnaire was read through several times to allow the lead researcher (RH) to become familiar with the data. All questionnaires were printed out. Each question was analysed in turn. Codes from each question were identified and highlighted. Once codes from a question had been identified from all questionnaires, this process was repeated to ensure no codes were missed. Codes within each question were then counted and underlying context was interpreted through the generation of categories and themes. This process was done for each question individually. A second researcher (RB) independently analysed the codes for each question and then determined categories and themes. The codes, categories and themes of each researcher were compared, and a consensus was agreed. Relevant quotations were extracted to promote the authenticity and trustworthiness of the data (Elo and Kyngäs, 2008).
Results
Three hundred and forty dietitians were invited to take part in the study. Of these, 33 (9.7%) met the eligibility criteria, gave informed consent and participated. The answers to each question are described below.
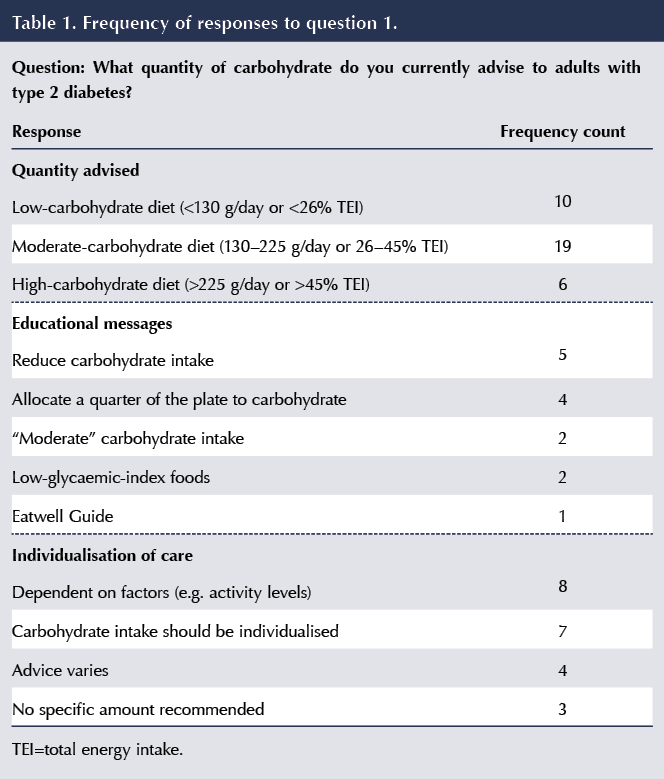
Q1. What quantity of carbohydrate do you currently advise to adults with type 2 diabetes?
Thirty-three participants (100%) responded to this question. The frequency of responses can be found in Table 1.
Quantity
Nineteen participants (57.6%) responded to this question quoting grams per day. Five participants (15.2%) responded to this question by using percentage of total energy intake (% TEI).
Within these responses, 19 participants stated they might advise a moderate-carbohydrate diet (57.6%), ten a low-carbohydrate diet (30.3%) and five a high-carbohydrate diet (18.2%). Sixteen respondents presented a range, so not all respondents were exclusive to one category.
Educational messages
Common educational messages included advising a reduction in carbohydrate intake (n=5) and filling one quarter of the plate with carbohydrate (n=4).
Individualisation
Several participants placed a strong emphasis on individualisation of care, suggesting their advice would depend on a number of factors, including the person, current intake, glycaemic control, weight, motivation, ability to make changes, medication, activity level and patient preference.
Q2. With regard to carbohydrate, how appropriate do you feel that the Eatwell Guide is in advising adults with type 2 diabetes (50% energy from carbohydrates)?
Thirty-three participants (100%) responded to this question.
Appropriateness of the Eatwell Guide for adults with type 2 diabetes
Sixteen participants responded that 50% TEI from carbohydrates, as promoted by the Eatwell Guide (Public Health England, 2016), is too high for adults with type 2 diabetes. An additional eight responded that the Eatwell Guide carbohydrate suggestion was inappropriate for adults with type 2 diabetes. Therefore, a total of 24 participants (72.7%) reported that the carbohydrate intake advised in the Eatwell Guide is either inappropriate or too high for adults with type 2 diabetes:
“[Type 2 diabetes] could be considered a condition of carbohydrate intolerance. We would not suggest to someone with coeliac disease to eat gluten, so why does the Eatwell Guide suggest to someone with [type 2 diabetes] to ensure their diet comprises 50% carbohydrate?” (Participant 9)
One respondent commented that the Eatwell Guide does not echo the stance of Diabetes UK that there is little evidence for an ideal proportionate macronutrient intake for people with type 2 diabetes. Six respondents commented that the Eatwell Guide does not individualise advice, something considered important by this cohort.
Four respondents highlighted the difficulty that this nutritional model presents to overweight adults with type 2 diabetes or those who have insulin resistance.
The Eatwell Guide as a public health tool
Two participants recognised that the Eatwell Guide is a public health tool as opposed to being designed specifically for adults with type 2 diabetes. One participant suggested that it is suitable for healthy people and not those with a chronic condition such as type 2 diabetes. It was suggested that the Eatwell Guide is a useful tool to illustrate health messages such as the promotion of fruit and vegetable intake and reduction of high-sugar foods and drinks. However, one respondent suggested that 50% TEI from carbohydrates is likely to be too high even for the general population.
Trustworthiness of the Eatwell Guide
Two respondents discussed how, as it is a widely used tool produced by Public Health England, the Eatwell Guide is trusted by both patients and clinicians. One commented that the Guide can be a starting point for healthcare professionals, but the other stated that patients might not want to decrease carbohydrate intake if they trust the recommendations of the Eatwell Guide.
What guidance would be appropriate for adults with type 2 diabetes?
Several respondents made suggestions as to how the Eatwell Guide could be adapted for adults with type 2 diabetes. Suggestions included reducing the TEI from carbohydrate to 25%, 40% or 25–50%, with one respondent suggesting the appropriateness of 25% TEI from carbohydrates as depicted on diet plates. Others suggested placing more of an emphasis on vegetables, salad and protein, and less on starchy carbohydrates.
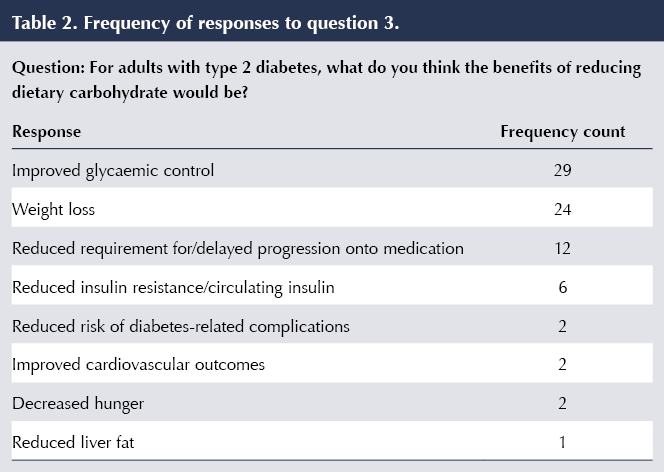
Q3. For adults with type 2 diabetes, what do you think the benefits of reducing dietary carbohydrate would be?
Thirty-three participants (100%) responded to this question. The frequency of responses can be found in Table 2.
Glycaemic control
Twenty-nine participants (87.9%) reported that a reduction in dietary carbohydrate would improve glycaemic control in an adult with type 2 diabetes. Additionally or independently, several respondents identified individual elements of glycaemic control that would be improved: blood glucose levels, HbA1c and postprandial blood glucose levels.
Nine respondents reported that a reduction in medication would be seen and three reported that the progression onto diabetes medications would be delayed.
Weight loss
Twenty-four respondents (72.7%) attributed weight loss to a reduction in dietary carbohydrate. Two respondents acknowledged the greater satiating properties of the other macronutrients.
Other medical benefits
Other identified advantages of reducing dietary carbohydrate included decreased liver fat, delayed progression or reduced risk of diabetes-related complications, and improved cardiovascular outcomes such as lipid levels and blood pressure.
Q4. For adults with type 2 diabetes, what do you think would be the disadvantages of reducing dietary carbohydrate?
Thirty-two participants (97.0%) responded to this question.
Nutrition
Commonly reported concerns of reducing dietary carbohydrate were lack of fibre (n=9), increased fat intake (n=9), increased protein intake (n=6) and increased calorie intake (n=5). Nutritional deficiencies were stated as a concern (n=4), as was an insufficient intake of vitamins and minerals (n=4).
Physiology
The risk of hypoglycaemia was a common concern (n=7). Other mentioned disadvantages were lethargy (n=6), hunger (n=3), decreased concentration (n=2) and stress (n=1).
Practicality
Practical disadvantages, such as the implications of meal planning (n=4) and increased cost (n=2), were suggested. One participant responded that patients could find this difficult to follow, and another highlighted that patients may simply be unwilling to follow this diet. One respondent suggested that advising patients to reduce dietary carbohydrate could cause confusion with regard to previous dietary advice (e.g. public health advice).
Three respondents raised questions about adherence to a reduced-carbohydrate diet.
No disadvantages
Three participants felt that, if managed appropriately, there would be no disadvantages to following a reduced-carbohydrate diet. One participant suggested setting a lower acceptable limit of carbohydrate intake. One participant did not respond to the question.
Q5. Do you think a low-carbohydrate diet (<130 g/day or <26% of total energy intake) is achievable for adults with type 2 diabetes? Please explain your answer
Thirty-three participants (100%) responded to this question. The frequency of responses can be found in Table 3.
Achievability
Twenty-eight participants (84.8%) felt that a low-carbohydrate diet is achievable for adults with type 2 diabetes, but there was a caveat attached to many responses, to include suitability, motivation and the need for support.
Barriers
Five participants (15.2%) felt that a low-carbohydrate diet would not be achievable for adults with type 2 diabetes, again offering some context.
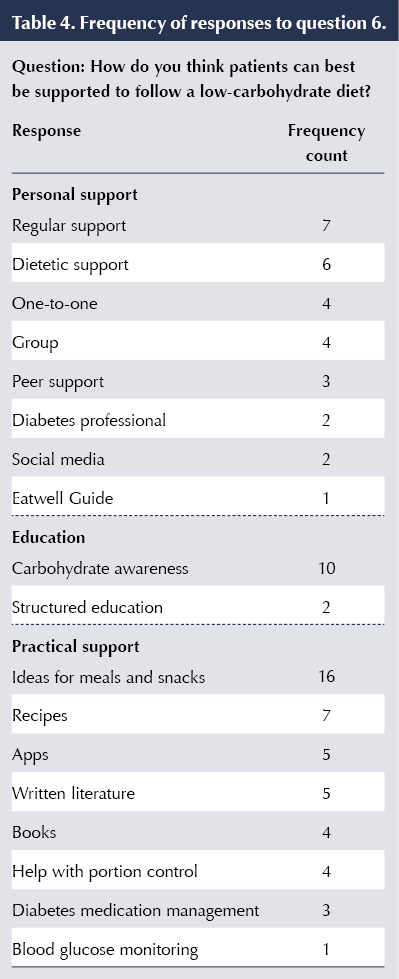
Q6. How do you think patients can best be supported to follow a low-carbohydrate diet?
Thirty-two participants (97%) responded to this question. Support was categorised into three broad headings: personal support, group education and practical support, to include meal and snack ideas, recipes, books and apps. The frequency of the various responses can be found in Table 4.
Health messages
Three respondents highlighted the importance of the alignment of messages from healthcare professionals regarding this topic. The need for consistency in messages was highlighted in addition to the need for well-informed and robust guidelines to guide healthcare professionals.
Four respondents stated it is important to advise low-carbohydrate eating within the context of a healthy diet.
Q7. Please share any other comments or views you have regarding dietary carbohydrate restriction within this patient group
Twenty participants (60.6%) responded to this question. The quotes below summarise the points made:
“The low-fat healthy eating diet has led to an increase in portion sizes of rice/pasta/potato and an attitude that these are healthy, so the more the better – this needs to be changed, and talking about reducing carbohydrate and explaining why really helps.” (Participant 30)
“Evidence suggests weight loss is key to management of [type 2 diabetes] but no evidence as to the best approach. Carb reduction not only offers opportunities for weight loss but reduces blood glucose levels as an added bonus.” (Participant 27)
“I think it would definitely be beneficial for diabetes management however the majority would struggle to achieve a low CHO diet. General CHO awareness is of importance.” (Participant 32)
“People with non-diabetic hyperglycaemia/pre-diabetes/impaired fasting glucose, however it is labelled, should be strongly advised to reduce their carbohydrate intake.” (Participant 32)
“Due to lack of long-term evidence regarding safety of low-carbohydrate diets (especially those that recommend 50–90 g per day) I am not comfortable recommending them for long term.” (Participant 7)
“Advice HAS to be individualised.” (Participant 13)
“Would like more research and evidence to be available as to benefits of this type of diet and sustainability long-term.” (Participant 25)
“Would value more support and resources from the BDA/Diabetes UK, etc., to support patients who wish to follow a low carbohydrate diet.” (Participant 26)
Discussion
This study used summative content analysis to explore the opinions of UK RDs regarding carbohydrate restriction as a management strategy in adults with type 2 diabetes. Thirty-three UK RDs from a diabetes specialist interest group took part. Participants were asked six focused questions and a final broad question inviting other comments on the topic.
The participants were overwhelmingly in favour of advising a restricted-carbohydrate diet to adults with type 2 diabetes, with 29 reporting they may advise low- or moderate-carbohydrate diets to adults with type 2 diabetes. Importantly, there was a strong emphasis around individualisation and there was acknowledgement that there is no one-size-fits-all approach.
A significant number of participants (n=24) also believe the current Public Health England dietary guidance, the Eatwell Guide, is either too high in carbohydrate or inappropriate for adults with type 2 diabetes. Some participants highlighted its purpose as a public health tool as opposed to one designed to support those with specific health conditions. Consequently, these data suggest that the RDs sampled believe the Eatwell Guide, and the message that 50% TEI should come from carbohydrates, should be interpreted with caution when advising adults with type 2 diabetes.
Most participants felt that a low-carbohydrate diet is achievable for adults with type 2 diabetes, but this conclusion requires further interpretation. Although participants felt it could be achieved, several raised important points and concluded that this diet would not be suitable for all adults with type 2 diabetes. Namely, an individual would likely need to be motivated and would likely need support. For RDs who felt that this diet is not achievable, cost and sustainability were the two key themes of concern, the latter of which is acknowledged in the published literature (van Wyk et al, 2016).
Participants were largely in agreement with respect to the perceived benefits of carbohydrate restriction, as almost all expected an improvement in glycaemic control with intentional weight loss where appropriate. A greater divergence of views was observed with regard to the possible disadvantages of reducing dietary carbohydrate. The overarching themes were potential nutritional concerns, health-related implications and practicality, with significant variation within the themes; the most commonly suggested disadvantages were lack of fibre, increased fat intake and increased risk of hypoglycaemia. Regular support, dietetic support and practical ideas for meals, snacks and recipes were cited by respondents as the key support needed by patients to follow a low-carbohydrate diet. Carbohydrate awareness was mentioned; however, despite being popular, this remains a poorly defined term among dietitians (McArdle et al, 2017).
Study strengths and limitations
Strengths of this research include the sampling from a population of RDs interested in diabetes through existing networks, and the rigorous analysis of the data using triangulation by a second investigator.
An obvious limitation to this study was the low response rate. Internet-based surveys are known to be time- and cost-efficient but can also have drawbacks such as selection bias and poor response rates (Fan and Yan, 2010). Sampling and sample size are important considerations for all research, and in a qualitative study such as this, where the response rate cannot be predicted, the validity and reliability of the data must be judged on factors such as saturation and replication of responses across themes (Elo et al, 2014). There was frequent replication and consistency of responses within themes in many questions, and these were identified by both authors involved in the data analysis, indicating the data were sufficiently saturated for these results to be reliable and trustworthy. The frequencies of all responses were reported in tables to promote transparency of the results.
Qualitative research does not claim generalisability, and these results are an exploration of the views of a UK-wide group of RDs with a special interest in diabetes. As previously referenced, online surveys can be subject to selection bias, and the relevance of the topic to the responders is also a major known factor in predicting the response rate for any survey (Dillman and Smyth, 2007). As a result, we are not claiming generalisability of these results but sharing the opinions of those clinicians who took part in the study. Equally, the study gave the opportunity for those who may have been against carbohydrate restriction to share their opinions, so we feel confident that the findings are valid. Furthermore, there were no incentives used in this study, a technique known to increase response rate (Fan and Yan, 2010).
Conclusions
In conclusion, UK RDs hold generally positive views of carbohydrate restriction as a management strategy for adults with type 2 diabetes, and their perceived benefits match the evidence base. There remains variation in clinical practice, but many RDs feel that UK public health guidance recommending a high-carbohydrate diet may not be suitable for adults with type 2 diabetes. Furthermore, consideration may need to be given as to how RDs may be supported in the provision of evidence-based low-carbohydrate dietary advice to adults with type 2 diabetes who choose to follow this approach over other dietary strategies, in a nutritionally balanced, acceptable and sustainable manner. The results of this study may not be generalisable but show important data regarding the opinions and practices of RDs supporting patients with type 2 diabetes in the dietary management of carbohydrate.
Acknowledgements
The authors would like to thank the sponsor of the study, Bradford Teaching Hospitals NHS Foundation Trust. In particular, we would like to thank the Head of Nutrition and Dietetics and Specialist Diabetes Dietitians. We would also like to extend our thanks to Julie Taplin and the BDA Diabetes Specialist Group.
Author contributions
RH was responsible for protocol development, study design and conduct, data collection, analysis and interpretation, and manuscript writing. RB was responsible for review of protocol and study design, validity checking of data analysis and interpretation, and manuscript writing. PM was responsible for review of protocol and study design, and manuscript writing.
Conflict of interest
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.






Carefully selected highlights of the recent EASD 2025 meeting.
24 Sep 2025