Type 1 diabetes is a complex metabolic condition the management of which involves daily monitoring of glucose levels and multiple daily injections of insulin or continuous insulin administration via an insulin pump. People with the condition are advised to keep glucose levels within a target range to help reduce the risk of its associated short- and long-term complications.
Real-time continuous glucose monitoring (rtCGM) measures interstitial glucose levels continuously through a small sensor that sits under the skin. Its data can be sent to a continuous subcutaneous insulin infusion (CSII) device, rtCGM receiver or phone, depending on the device used. While some rtCGM devices require calibration with blood glucose testing, many, such as the Freestyle Libre, are now factory calibrated.
CSII therapy involves a device, commonly known as an insulin pump, that continuously delivers insulin via a cannula inserted through the skin. It can be tethered, with an infusion set (tubing) linked to the cannula, or comprise a fully enclosed pod/patch device with no tubing. CSII therapy offers the advantage of adjusting basal settings to better match circadian requirements, providing more precise treatment compared to the flatter basal rates achievable with multiple daily injection (MDI) insulin therapy (Nimri et al, 2020). Additionally, CSII can calculate bolus doses to address high glucose levels and track insulin activity, reducing the risk of insulin overdose and hypoglycaemia. People treated with CSII therapy have lower HbA1c and increased time in range (TIR; the percentage of time glucose levels stay within target range) compared to those treated with MDI (Ross and Neville, 2019; Scott et al, 2019).
Since 2022 in the UK, all insulin users with type 1 diabetes should have access to wearable diabetes rtCGM technologies (NICE, 2022). Some of these devices can communicate through Bluetooth technology with an insulin pump. From the rtCGM data, an algorithm works out how much insulin to deliver from the pump. This is known as hybrid closed-loop (HCL) technology, and it is effective in further increasing TIR.
These advances in diabetes technology aim to reduce the burden of managing diabetes and improve quality of life.
There is limited research on the impact of wearable technology on sexual activity in insulin users. However, difficulties with cannulas, infusion sets, disconnection and body image have been reported.
Three studies have reported difficulties with infusion sets. In one study, 10% of 271 participants viewed CSII as an obstacle during sexual activity, particularly because of the cannula (Riveline et al, 2010). Another reported difficulties with infusion sets, but there were no details of these problems (Santos et al, 2020). A further study reported the practical problems of sex with an electronic device attached (Cleal et al, 2021).
Studies have reported that up to 75% of users disconnect pumps for sex (Riveline et al, 2008; Robertson et al, 2019). Another suggested that discomfort for CSII users was higher during sex than for other activities of daily living (Joubert et al, 2014).
Problems with body image related to wearing devices have been reported in several studies (Quintal et al, 2020; Santos et al, 2020). One found that 26% of participants did not like how devices looked on their body, with almost half indicating that wearing devices all the time was a hassle (Naranjo et al, 2016). In another study, 10%–25% of participants said that sex was a reason for not adopting the technology (Robertson et al 2019).
To date, no research has been conducted in the UK into the impact of wearable diabetes technology on sexual activity. This study aimed to qualitatively investigate the effects of wearable diabetes technology on sexual activity for individuals with type 1 diabetes in the UK.
Methods
Study design, setting and participants
This qualitative study was conducted between January 2022 and January 2023. After receiving ethical approval from King’s College London, recruitment began through social media sites, such as Facebook, Twitter, LinkedIn and Instagram.
The main inclusion criteria were adults with type 1 diabetes using wearable diabetes technology who were willing to be interviewed. Eligible individuals received consent forms and interviews were scheduled. This convenience sample was chosen owing to the sensitive nature of the topic, without specific sampling criteria being employed.
Interviews
Data were collected using individual semi-structured interviews via Zoom, using an interview topic guide (see Appendix 1). The guide, developed from existing literature, was piloted in the first two interviews. As no changes were necessary, subsequent interviews were included in the main sample and analysed. Conducted by AE (an advanced nurse practitioner and diabetes specialist nurse), interviews lasted 30 to 60 minutes. AE had no prior relationship with participants. All interviews were recorded and transcribed verbatim. Demographic data were collected at the interview’s onset. The guide covered the impact of type 1 diabetes on sexual activity and relationships, support from healthcare professionals (HCPs) regarding wearable diabetes devices and sexual activity, and discussion of device design.
Qualitative data analysis
Transcripts were imported into NVivo software and analysed using an inductive approach using framework analysis (Bettany‐Saltikov and Whittaker, 2014). The steps of framework analysis included meticulous revision of all transcripts to align with the original recordings. Additionally, similar quotes were categorised under respective headings and subheadings, allowing for the extraction of the most recurrent themes. It is noteworthy that these thematic clusters correspond closely to the questions posed to all participants, ensuring consistency and comparability across responses.
Credibility
To bolster credibility, multiple participant quotes were integrated into the findings. The research process was supervised by academics from King’s College London as part of a dissertation module, ensuring thorough documentation of all research aspects for evaluation of the study’s probity.
Results
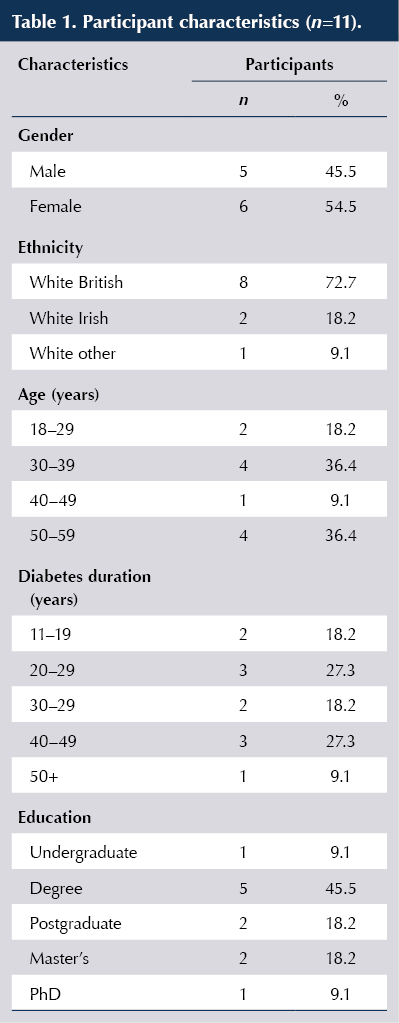
Twenty-one people expressed interest in the study, and 11 adults with type 1 diabetes consented and took part in the interviews. The main demographic information of the sample is presented in Table 1. There were slightly more females than males, all participants were of white ethnic background, and represented a range of ages and diabetes duration.
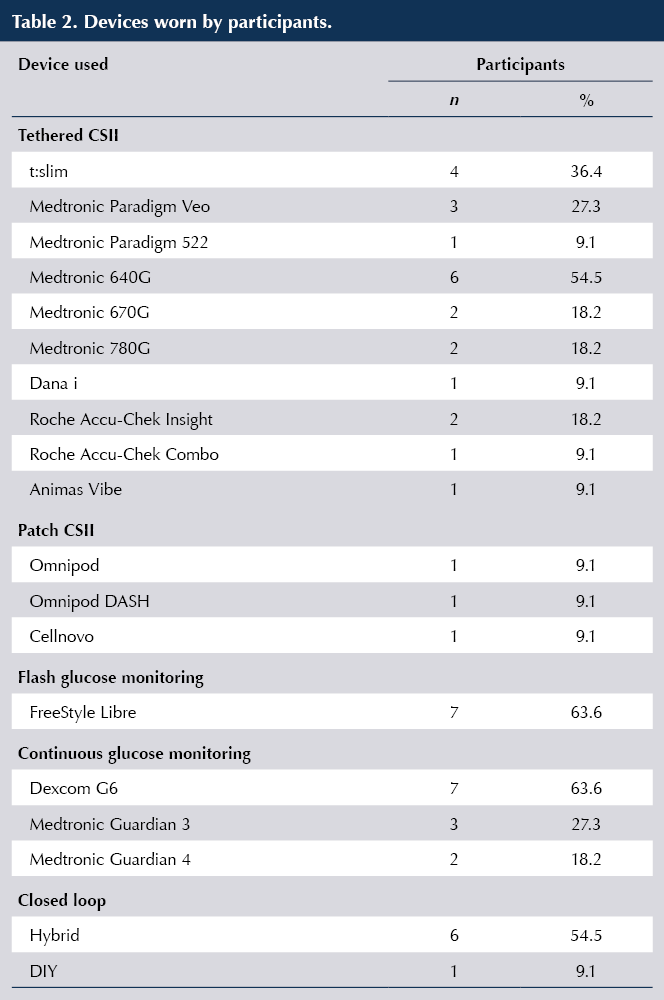
The majority had worn tethered CSII, and more than 50% of the sample had used a closed-loop system (Table 2).
Emerging themes
Four main themes emerged from the data analysis and, within each theme, there were numerous subthemes. The first theme related to the impact of wearable diabetes devices on relationships with partners. Subthemes included: establishing new relationships; and awareness of diabetes within the relationship. The second theme, related to the impact of wearable devices on sexual activity and blood glucose levels. Subthemes included: hypoglycaemia; spontaneity; diabetes as a distraction; diabetes as a turn-off; scratchy cannulas; and dislodging devices or removal during sex. The third theme was strategies to improve knowledge of wearable diabetes devices and sexual activity from HCPs. Subthemes included: importance of sex; and HCPs’ responsibilities. The fourth theme was technological improvements to address the negative impact of wearable devices on sexual activity. Subthemes included: size matters; cannulas and tubing choice; device alarms; and linking to CGM.
Impact of wearable diabetes devices on relationships with partners
Wearable devices significantly influenced participants’ relationships with their partners, particularly regarding sexual activity. The primary reason cited for this impact was the necessity of disclosing their diabetes diagnosis, prompting many to take measures to avoid such discussions. This challenge was more pronounced in new relationships, with participants expressing greater comfort in long-term relationships where devices were less of a concern. Building the confidence to disclose their diabetes status to new partners was difficult for many, leading some to disclose prematurely. One participant highlighted the mental effort required to manage diabetes without affecting new relationships. Some participants refrained from casual sex owing to their diabetes, while others found discussions about their devices disrupted the atmosphere and delayed sexual activity:
“Especially with new people. I always disclose my diabetes beforehand, but back in uni, it felt awkward bringing it up during intimate moments, disrupting the mood.”
[Participant 1, aged 35 years]
Participants were aware of the impact of diabetes on their relationships. Concerns arose about partners’ commitment, owing to their long-term medical condition. They noted a distinction between short- and long-term relationships, with type 1 diabetes having a greater impact on the former, but with more support in the latter.
“I’m in a long-term relationship, and she’s known right from the outset that I have it and, therefore, it hasn’t impacted this relationship. I would imagine if we were to break up and I were to go dating again, I’d find it relatively tough.”
[Participant 6, aged 28 years]
Impact of wearable devices on sexual activity and blood glucose levels
All participants acknowledged the impact of type 1 diabetes on sexual activity, citing fluctuating blood glucose levels as the primary reason. Many highlighted hypoglycaemia as a significant hindrance and “mood killer”, necessitating treatment to either address or prevent it. Additionally, experiencing a hypo can pose physical challenges, with male participants hinting at difficulties related to erectile dysfunction:
“I can think of a few occasions when I had bad hypos during sexual activity; that’s a bit of a passion killer.”
[Participant 4, aged 54 years ]
“Once you’ve stopped to treat a hypo and allowed your blood sugar to come up, there’s not much getting things started again after that.”
[Participant 9, aged 30 years]
The second most frequent impact when managing type 1 diabetes and sexual activity was on spontaneity, or perceived lack of it. Two participants compared sexual activity to exercise and spoke about the advice they were given to manage that – such as planning or having a snack – and how this is very difficult to follow with unplanned sexual activity:
“Spontaneous activity is challenging, and sexual activity should be spontaneous. I don’t think it is normal behaviour to sit there and plan two hours in advance ‘I think we might have sex tonight.’”
[Participant 5, aged 50 years]
“You’re having sex, you probably need to have a snack beforehand and blah blah blah, check your blood sugar and come on, like who’s actually gonna say ‘okay I know we’re getting into it now, let’s just wait, let me just check my blood sugar?’ Let me just eat a cereal bar or a banana and I’ll be with you in two minutes. That’s a mood killer for you, isn’t it?”
[Participant 9, aged 30 years]
Another subtheme arose was that of diabetes as a distraction during sexual activity. People with diabetes are continuously distracted by thoughts on management of their condition:
“I think having diabetes, full stop. Not least because, again, you’re just always thinking about it. Therefore, there’s a portion of your brain that’s working on something that’s not sexual activity.”
[Participant 6, aged 28 years]
Most participants did not mention the impact of wearable devices had on sexual partners. However, one believed that the impact of the devices they wore had contributed to a relationship ending:
“I think the fact that I had got wearable devices kind of almost meant that when we were intimate, particularly, it sort of reminded him that, you know, in his mind I had a medical issue.”
[Participant 10, aged 58 years]
By contrast, another said their partner was not at all interested in the devices they wore:
“…obviously much more interested in having a naked situation, than caring I had this machine on my body.”
[Participant 7, aged 37 years]
A few participants who wore tethered pumps mentioned how, when detached from the pump, the cannula can be scratchy for their partners. Some had been advised by HCPs to put the cap on to reduce the issue:
“She was the first person who ever said to me about basically putting the cap on the cannula and she said, and this is really useful you know if you shower, but also for if you get intimate.”
[Participant 10, aged 58 years]
Alarms were mentioned by a few participants. They discussed how they can be quite intrusive when they go off during sexual activity. Some have built-in safety functions that mean the alarms cannot be turned off.
“Alerts that will sound after 15 minutes, even if you set it to vibrate. 15 minutes is not enough! It’s a loud sound, it’s an alert and it’s designed to take you out of a situation and, therefore, it takes you out of a situation very effectively.”
[Participant 3, aged 34 years]
Most of participants would not remove their rtCGM routinely for sexual activity. Reasons included that they cannot be reattached if taken off, so this would be very expensive to replace if self-funding.
However, most participants said they would remove the tethered CSII during sexual activity. Reasons given included the potential for the tubing on tethered pumps to get tangled, leading to the device getting dislodged. Only one participant said they would not normally take a tethered pump off as they may forget to put it back on, and they were worried about falling asleep and waking up with high glucose levels or in diabetic ketoacidosis. Some of the participants who did remove the pump also had concerns that disconnection would cause hyperglycaemia. One patch pump user consciously planned sexual activity around patch changes to avoid wearing the device during sexual activity.
Many of the participants said they removed the pump, as they didn’t really know what else to do with it. This was more common in those using HCL technology, as they have not been advised on what to do during disconnection for sexual activity. One suggested they would disconnect and not suspend the pump, as the alarms go off after 15 minutes. Another said they would disconnect and leave it running, hoping that the exercise during sexual activity would make up for lost insulin delivered by the unconnected pump.
“I guess when you’re having sex and you take your pump off, you’re always conscious about how long you’ve had your pump off for because you’re going to have to deal with the after-effects anyway.”
[Participant 9, aged 30 years]
“I think because you’re active during that time, even if you take it off and you’re not getting the insulin that it thinks it’s given you, you kind of compensate for that with activity. Unless you’re not as active as we are.”
[Participant 11, aged 28 years]
Most participants said they had dislodged a device during sexual activity. Just under half had dislodged a cannula, some had dislodged a sensor and a small number of participants had dislodged both at some point during sexual activity:
“I think if I’ve dislodged the Dexcom or something, it’s probably already been a sweaty day and it’s starting to come loose, and I haven’t bought the tape thing that goes over it.”
[Participant 7, aged 37 years]
Participants generally seemed relaxed about dislodging the devices. Many said they would carry on with sexual activity and put another one in afterwards. One mentioned that if they do dislodge a device, they can call the company for a replacement, but this can be embarrassing:
“They make you ring up and explain what you were doing, but I just hate ringing places up and trying to email and you’re told ‘no, you have to ring this line’ and you’re like, arrghh! How do you tell them how it came off? I’m not telling them why.”
[Participant 7, aged 37 years]
Most participants said that their sexual behaviour does not change depending on where their diabetes device is situated. Generally, this is because they use the same place for devices based on comfort or clothing choice. The small number of participants who said sexual behaviour does change device placement all used their leg as an example, either to avoid injury from the steel cannula or to avoid the cannula scratching their partner:
“So, if it’s on my leg, I will avoid any positions that means like I’m on the side. So I don’t end up lying on it, especially the steel ones. My legs are not as fatty as my tummy so, when it’s there, it can hurt if I push on it.”
[Participant 3, aged 34 years]
“Say, for example, if I’ve got a cannula or a sensor in my leg. And say… say my wife is on top and then, if we’re having sex, then it tends to be uncomfortable for me because I could feel my cannula on my leg or it would be uncomfortable for her ’cause she’d end up getting scratched on my cannula, you know, which will be on my leg.”
[Participant 9, aged 30 years]
Strategies to improve knowledge of wearable diabetes devices and sexual activity from HCPs
All participants said their HCP did not mention sexual activity when discussing device choice. Participants suggested that sex is a big part of life and needs to be addressed at device start, as it can impact on choice. The guarantees on some pumps mean that once chosen, you will not get to upgrade for 4 years. They suggested that all aspects of living with the device should be discussed by an HCP before starting it. Many alluded to the sensitive nature of discussing sexual activity, both for HCPs and people living with type 1 diabetes:
“Well, nobody’s ever discussed sexual activity on devices with me, ever. But, then again, nobody’s ever discussed sexual activity and diabetes, with me. Ever. It seems to be a taboo topic.”
[Participant 5, aged 50 years]
“I don’t think there’s enough kind of emphasis on the fact they wear it all the time, including when they’re having sex, thinking about that as part of the device choice is quite important because, you know, once you’ve got it, you’re stuck with it.”
[Participant 1, aged 35 years]
Some participants have had discussions about sex, but this was after CSII or rtCGM choice was already made. Suggestions on how HCPs could discuss the subject of sexual activity and wearable technology included educational days or leaflets on frequently asked or unasked questions. They also suggested HCPs could discuss management of sexual activity and diabetes, such as signs of a hypo and what to tell partners if something goes wrong.
Technological improvements to address the negative impact of wearable devices on sexual activity
Many of the participants said devices should be made smaller or lightweight, and that designers need to improve cannulas or tubing to avoid issues with entanglement and device placement. Some suggested the need to make more tubeless pumps or provide different tubing lengths.
“Why do they have to be so humongous? I mean, you know, we can get mobile phones down to stupid sizes. There must be a way of reducing it.”
[Participant 4, aged 54 years]
“I think ease of unclipping and clipping your cannula back in again, I think that could do with some work. And then, on the other hand, you want it secure, you want it in place and you don’t want to accidentally pull that cannula out.”
[Participant 9, aged 30 years]
Some participants mentioned reducing the alarms as a potential improvement, while another suggested linking the pumps to rtCGM to improve glucose control, as they felt that people are more likely to have sex if their glucose is in target range:
“Yeah, the alerts. It’s not even just for sex. Sometimes you want to have a long bath and you don’t want to take your insulin pump into the bath because it will expire because baths are hot.”
[Participant 3, aged 34 years]
“I think that the manufacturers can be too prescriptive as to what the alarms are.”
[Participant 5, aged 50 years]
Discussion
This research aimed to qualitatively investigate the impact of wearable diabetes technology on sexual activity for adults with type 1 diabetes. The main themes arising included the impact of wearable diabetes devices on relationships with partners; the impact of wearable devices on sexual activity and blood glucose levels; strategies to improve knowledge of wearable diabetes devices and sexual activity from HCPs; and potential technological improvements to address the negative impact of wearable devices on sexual activity.
When it came to relationships with partners, one of the main impacts was that devices took the choice away about disclosing their condition. Type 1 diabetes is relatively uncommon, which may contribute to a lack of understanding of it in society. Diabetes stigma is also common (Liu et al, 2017) and some people feel ashamed of managing their type 1 diabetes in public (Jeong et al, 2018), making them feel isolated (Basinger et al, 2020). In this research, participants had a reluctance to discuss their condition with a potential new partner.
Sexual experiences may take place before relationships become committed. In our study, participants discussed the challenges of educating new partners on the condition during times where they would prefer to be engaged in sexual activity, and how devices removed the option of concealment until a more appropriate time. One participant went as far as disconnecting the pump and risking hyperglycaemia to avoid conversations about diabetes with a new partner, and another would not fully undress to keep devices concealed. However, most participants did not try to conceal devices from new sexual partners, a similar finding to a cross-sectional survey study by Pinhas‐Hamiel et al (2017).
Hypoglycaemia during sexual activity was an important consideration for participants in this study. Views of the technology in relation to this were mixed. Some wearable diabetes technologies reduce hypoglycaemia by suspending or reducing insulin infusion when glucose levels are dropping. Furthermore, the alarms on some rtCGM and flash glucose devices can promote a proactive approach to managing falling glucose levels and reduce the occurrences (Miller and Midyett, 2021). In our study, some participants reported how increased TIR resulting from wearable technology led to more sexual activity. For others, however, hypoglycaemia was a “mood killer”.
Many participants in this research had experienced or had concerns about hypoglycaemia during sexual activity, yet this was never discussed by HCPs during diabetes appointments, even though sexual activity can be considered as significant physical activity (Pinhas‐Hamiel et al, 2017). In this study, participants stated that sexual activity is usually spontaneous, and the management strategies that HCPs advise for exercise, such as reducing insulin or having a snack to avoid hypoglycaemia, are often not transferable to sexual activity. One qualitative study showed that hypoglycaemia interrupted or discontinued sex, impacted on the ability to enjoy sex and caused participants to have concerns about disappointing their partner (Chatwin et al, 2021). Participants in this study suggested that sex is a significant part of life and should be considered when choosing a wearable device. Sex is important to quality of life (Flynn et al, 2016) and should be discussed by HCPs during consultations.
Living with diabetes can be complicated, demanding and often confusing. This research shows that type 1 diabetes can be a distraction during sexual activity, with participants commenting that a part of their mind is constantly thinking about the management of their condition.
Alarms can be intrusive when they go off during sexual activity, as reported by some in this study. Alarm fatigue has been investigated in many studies surrounding medical devices (Mitka, 2013), with a some focusing on alarm fatigue with diabetes devices (Shivers et al, 2013; Mariani et al, 2017). Until this study, however, there has been no research on alarms and the impact on sexual activity. A strategy to reduce alarm fatigue in relation to diabetes wearable devices was reported by Miller and Midyett (2021), and included options to turn off alarms. This could work for sexual activity, although, in our study, participants highlighted that there was no option to disable the alarm on their devices.
Of the small number of participants who reported that they had changed where they wore their device, all used their leg as an example. Siting on the leg can result in pain and discomfort during sexual activity. This could be discussed with people who are starting devices to avoid them experiencing the same issues.
Potential solutions mentioned included the need to make devices smaller or lightweight. Other potential targets for improvement included cannulas and tubing length, and making them easier to unclip for sexual activity. Participants also wanted to be able to alter settings on alarms, to avoid them going off and ruining the mood or causing their partner distress. Participants suggested more pumps need to link to rtCGM to improve glucose control, as people are more likely to have sex if their glucose level is in target range.
Strengths of study
This is the first qualitative study to explore the impact of wearable type 1 diabetes technology on sexual activity in a UK setting. The sample covered a wide age range, with varied duration of diabetes. Most participants used multiple devices and so were able to identify which features impacted most in terms of sexual activity.
The lead researcher who conducted the interviews lives with type 1 diabetes, and has personal experience of many of the issues being discussed, reducing potential misunderstandings, encouraging open conversation and establishing trustworthiness.
Limitations
All of the participants were of white ethnicity, which limits the transferability of findings. Ethnic disparities in access to CSII therapy (Willi, 2015) could have impacted the recruitment of volunteers from other ethnicities.
All the participants were over 28 years of age – no young adults (aged 18–24) volunteered. This could be due to the sensitive nature of the topic or the method of recruitment. In future studies, alternative recruitment methods could be introduced, such as advertising on Snapchat or TikTok.
Nearly all the study participants were educated to degree level and above. People from lower socioeconomic backgrounds are less likely to complete a degree programme (Crawford, 2014), so this research may not be reflective of participants from more deprived communities. Furthermore, all participants had had diabetes for over 10 years, potentially bringing greater confidence in managing their condition. Some factors that impact newly diagnosed participants may not have been raised.
The lead researcher lives with type 1 diabetes, is a HCP, a director of a large online diabetes specialist nursing group and is known on social media for being an advocate for people living with the condition. To avoid bias, the researcher did not discuss their own experiences. However, this may have had an impact on data collection, as some participants may not have fully explained their points, assuming that the researcher understood what they meant.
Implications for practice
People with type 1 diabetes may need more support from HCPs to address stigma in relationships and to work out how to approach the subject of sexual activity and diabetes devices. This would mean HCPs overcoming their reluctance to discuss sexual activity in clinical situations.
Conclusion
Whilst wearable diabetes technologies have improved health outcomes for people with type 1 diabetes, they have introduced some barriers in establishing long-term relationships, concerns about body image and stigma. Users may be put at risk of acute diabetes complications when disconnected during sexual activity. The findings from this study highlight a need for open dialogue with HCPs, who may require training to provide specific advice on wearable diabetes technology and sexual activity. This research also offers device manufacturers factors to consider when designing future wearable technology.
Further research should consider investigating this topic amongst non-white individuals, young adults, people with a new diagnosis and those from deprived communities.





Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025