Nutritional management is well recognised as a foundation of care for diabetes (NICE, 2022). Children and young people (CYP) with type 1 diabetes are advised to follow the healthy eating guidelines that apply to the general population (Annan et al, 2022). Optimal growth, development and diabetes outcomes are dependent on a healthy diet that includes adequate energy and essential nutrients (Mendoza et al, 2018). To prevent the acute and chronic complications of type 1 diabetes, it is essential that CYP have a consistent supply of sufficient, accessible and nutritious food (Annan et al, 2022).
Food insecurity and rising cost of living
Owing to economic and social influences, a household may lack the resources or accessibility to provide a nutritionally adequate diet – a situation known as food insecurity (FI; US Department of Agriculture, 2022). The current rise in the cost of living has resulted in more households experiencing FI. In April 2022, the Food Foundation reported that it was experienced by 15.5% of all UK households. Those with children, receiving universal credit or from minority ethnic groups are most likely to be affected (Francis-Devine et al, 2022).
FI can be sub-categorised by its severity. “Low food security” is a reduction in the quality and diversity of food offered, while “very low food security” is a reduction of food intake secondary to a lack of money or resources (Francis-Devine et al, 2022). The level of FI is likely to determine the most appropriate intervention and support.
The effect of food insecurity on type 1 diabetes
FI has a significantly greater impact on families with children living with type 1 diabetes compared to the general population (Malik et al, 2021). The reasons are multifactorial, but centre around the requirement for high-quality food and supplies to avoid hypoglycaemia (Cox et al, 2021).
Studies have linked FI to lower quality diets and worsened glycaemic outcomes (Mendoza et al, 2018). It is associated with a greater consumption of foods with a higher calorie density (such as fats, oils and refined carbohydrates) and a lower intake of nutrient-dense foods (such as fruit and vegetables), which may increase dietary glycaemic load (Annan et al, 2022). Additionally, those who are severely food insecure are more likely to have a significantly higher than average BMI (Bawadi et al, 2012).
Hypoglycaemia fears may also be exacerbated by food scarcity and lead to the long-term elevation of glucose levels to reduce this risk (Reid et al, 2023).
Screening for food insecurity
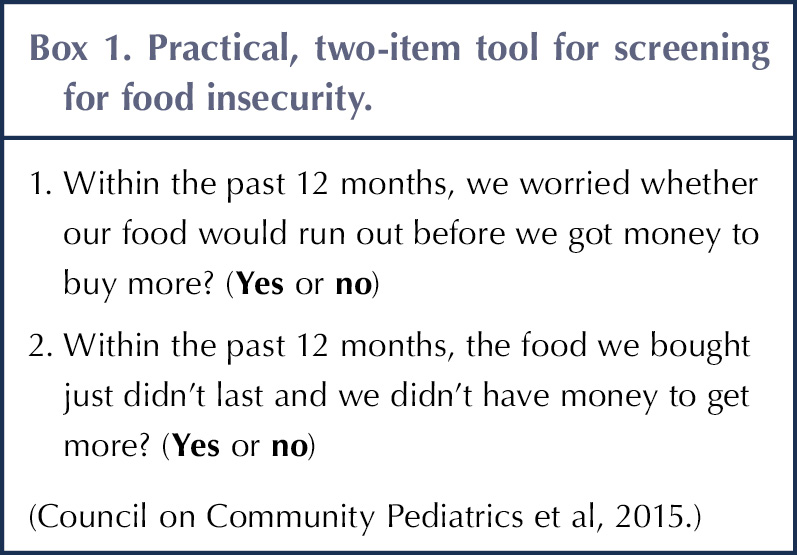
Paediatric diabetes clinicians should always consider FI, regardless of economic or social status (Annan et al, 2022). The American Academy of Pediatrics implemented two questions that can be incorporated into routine clinical assessment to screen for FI (see Box 1). An affirmative answer to at least one question is an indication of FI and should prompt additional questioning (Council on Community Pediatrics et al, 2015). Assessment of FI is also recommended by the American Diabetes Association and International Society for Paediatric and Adolescent Diabetes, although no specific screening methods are suggested (ADA, 2020; Annan et al, 2022).
Resources and support
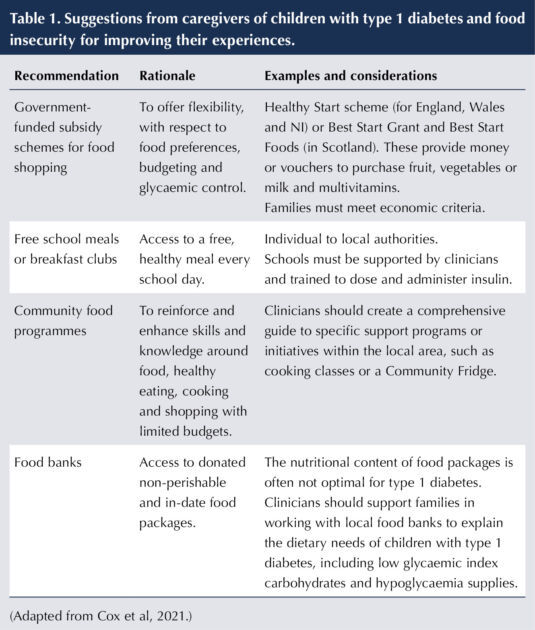
Appropriate resources and support should be offered to families living with FI to ease the challenges and pressures to which they are exposed, and to meet dietary recommendations. Clinicians should recognise that families of CYP living with type 1 diabetes may experience additional barriers to accessing standard support to combat FI. For example, free school breakfast programmes may require staff to carbohydrate count, dose adjust and administer insulin if a child is unable to do this independently, which is likely to require further assistance from the diabetes team (Cox et al, 2021).
Cox et al (2021) summarised suggestions from caregivers of children living with type 1 diabetes and FI to improve their experiences. These have been adapted in Table 1 to provide UK-based intervention examples.
Healthy eating with a limited budget
Clinicians should support families living with low food security in a person-centred way to improve the quality of their diet whilst remaining within their budget. Advice should be holistic and personalised for the individual family, and respect their living conditions, family relationships, income and cultural preferences (Annan et al, 2022). It is also important that clinicians consider the resources available for acquiring, preparing and cooking food (Annan et al, 2022).
Empowering families to plan meals in advance and create a shopping list can help to provide a healthy, balanced diet with a limited budget (British Nutrition Foundation, 2022). Research indicates that caregivers of children living with type 1 diabetes and FI would like access to comprehensive collections of recipes and weekly meal plans with shopping lists to encourage glycaemic management through the use of affordable ingredients (Cox et al, 2021).
Clinicians should recognise limited food budgets and provide appropriate advice around shifting patterns of dietary intake from inexpensive carbohydrates and fats towards nutrient-dense vegetables, fruits, protein and dairy products (Annan et al, 2022). Families could be encouraged to choose canned and frozen versions of fruit and vegetables, which cost less, require less preparation and usually result in less food wastage (British Nutrition Foundation, 2022). Economy ranges for starchy carbohydrates and dairy products are generally good value8 (British Nutrition Foundation, 2022). Lower-cost protein sources, such as beans or lentils (canned or dried) and eggs, can be used to add substance to recipes or substitute for meat, and are easily stored (British Dietetic Association, 2021).
Discussion and education on appropriate portion sizes of preferable foods are likely to be cost-effective and of equal value to recommending alternative affordable foods (Annan et al, 2022). Pictorial resources can improve caregivers’ recognition of developmentally appropriate portion sizes for CYP (Johnson et al, 2014).
The economic burden on CYP and their families of treating a hypoglycaemic episode can vary (Fidler et al, 2011). Diabetes clinicians should recognise the possibility of increased fear of hypoglycaemia associated with FI and provide innovative strategies to optimise glycaemic management and prevent frequent treatment for hypoglycaemia (Reid et al, 2023).
The value of diabetes technologies in reducing hypoglycaemia risk should be considered (McEwan et al, 2018). Continuous glucose monitoring (CGM) systems are widely available on prescription for CYP with type 1 diabetes. CGM can decrease time in hypoglycaemia, increase time in range and alleviate worries about hypoglycaemia (Tauschmann et al, 2022). Personalised CGM alerts for low glucose are available and recommended for those with recurrent hypoglycaemia (Tauschmann et al, 2022). In addition, hybrid closed-loop (HCL) systems can reduce HbA1c without increasing hypoglycaemia, and are recommended as an option for managing type 1 diabetes for CYP (NICE, 2023). However, effective use of insulin pump therapy is subject to a number of practical, psychosocial, behavioural and educational considerations, as well as funding arrangements within local health boards or trusts (Sherr et al, 2022).
Discussing low-cost ways to treat hypoglycaemia is important to include in routine clinical assessments (Cox et al, 2021). For example, glucose powder is affordable and readily available in large quantities. Depending on geographical area, it may also be appropriate to encourage uptake of glucose drinks available at no cost on prescription (British National Formulary, 2023).
Psychological support
FI can contribute to psychological distress in CYP (Leung et al, 2020) and their families (Liebe et al, 2022). For those also living with type 1 diabetes, this effect is intensified (Cox et al, 2021). A survey of food bank users in the UK highlighted that food aids are often only used as a last resort and are associated with considerable embarrassment, negative impact on self-worth and isolation (Purdam et al, 2016). Feelings of shame can result in people detaching themselves from society and potential sources of help, making engagement with families more challenging (Chase and Walker, 2012).
Clinicians should acknowledge this impact and tailor their approach to allow for open discussion surrounding issues of FI, whilst minimising distress (Cox et al, 2021). A person-centred approach to counselling should be prioritised, as it is likely to build trust and improve well-being (Ball et al, 2016). Demonstrating warmth and empathy can help to establish a quality relationship with the family, where they feel comfortable to express their concerns (Schultz et al, 2020). Questionnaires or agenda-setting tools filled out by families prior to consultations can help them to identify and articulate their priorities (Schultz et al, 2020).
Where psychosocial problems are identified, collaborative support should be provided by the multidisciplinary team and professionals with expertise in the mental health of children and adolescents, if appropriate (de Wit et al, 2022).
Conclusion
In light of the rising cost of living, paediatric diabetes clinicians should be aware of the complex challenges for families living with type 1 diabetes and FI, particularly for groups disproportionately affected by food insecurity. Owing to the multifactorial nature of FI, there is no single recommended intervention to optimise access to high-quality nutritious food.
Clinicians have a vital role in screening for household FI at routine clinical assessments, regardless of economic status. Where FI is indicated, intervention is highly dependent on the clinician’s evaluation of its severity, and should be tailored to individual family circumstances. For example, if low food security is indicated, nutritional counselling and advice around healthy eating with a limited budget would be a suitable intervention. However, when very low food security is suspected, supporting families in working with local food banks is likely to be more appropriate.
Local networks of clinicians should collate and share any resources and support that are relevant to geographical areas and population groups, to standardise and improve care.
Beyond its physical health consequences, there is strong evidence that FI impacts the mental health of young people and their families. This can present difficulty engaging with and accessing much-needed help and support. Holistic family well-being must be considered during all consultations, and clinicians should use advanced communication skills to ensure families feel comfortable to express their needs and concerns. Where psychological distress is identified, families should be referred to appropriate information and support.
Further research into the relationship between FI and adverse health consequences for CYP living with type 1 diabetes is needed. In addition, evidence-based strategies to optimise access to high-quality nutritious food should be prioritised. n
Acknowledgements
The author would like to thank the academic team on the Children and Young People’s Diabetes Care Module at Birmingham City University and the paediatric multidisciplinary team at Swansea Bay University Health Board.






Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024