Healthcare professionals frequently ask people with type 2 diabetes about their weight and request to weigh them during consultations (NICE, 2014; Royal Australian College of GPs, 2020a). Indeed, body weight is an important aspect of type 2 diabetes management, and general healthcare. Approximately 90% of people with type 2 diabetes also have overweight or obesity. For those people, clinical guidelines recommend a 5–10% reduction in body weight. However, for many people with type 2 diabetes, discussions about weight are unwanted, unhelpful and/or stigmatising, making them counterproductive and potentially leading to disengagement from healthcare (Litterbach et al, 2020). Discussions about weight are also fraught for healthcare professionals, who describe feelings of pessimism, hopelessness and frustration (Dewhurst et al, 2017). Consequently, some professionals avoid discussing weight-related care, which may have detrimental health consequences for the individual (Talbot et al, 2021).
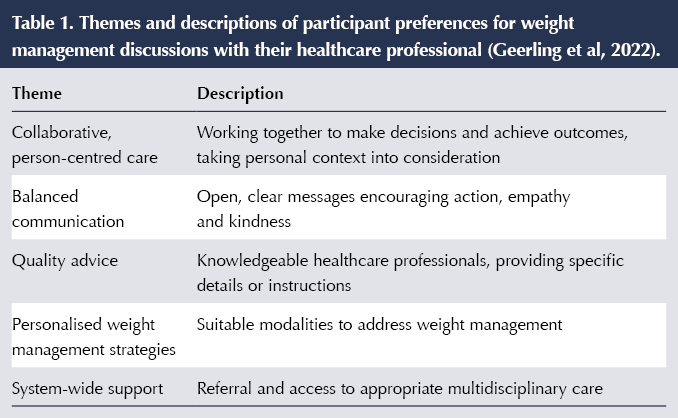
Acknowledging the above challenges, we previously investigated how adults with type 2 diabetes believe the discussion of weight in diabetes consultations can be best approached; that is, what makes a productive and acceptable discussion about weight management in a diabetes consultation, thereby supporting the delivery of effective and comprehensive clinical care (Geerling et al, 2022). We developed an online survey asking Australian adults with type 2 diabetes to describe (in free text) their weight story and, “in an ideal world”, how they would like their main healthcare professional to “broach the topic of weight management”. A total of 254 people responded. We organised the responses into five themes describing respondents’ preferences for weight management discussions (Table 1).
In this commentary, we draw upon our published study findings to propose five considerations to guide constructive weight management discussions with adults with type 2 diabetes.
1. Collaborative, person-centred care
Person-centred care was an overarching theme that unified all five themes. People want to be treated as a person first and for their individual needs and experiences to be respected and considered. Ideally, person-centred principles (Royal Australian College of GPs, 2020b) guide all aspects of care, including communication style, advice, weight management strategies and referrals. Indeed, guidelines for the clinical management of type 2 diabetes recommend a person-centred approach (NICE, 2015; Royal Australian College of GPs, 2020b).
In practice, this means that the healthcare professional should ask open questions and then listen for important contextual information to inform personalised management strategies. As one participant explained:
“Ask about my lifestyle, ask about who I live with and their lifestyle, give options to fit with mine and my partner’s lifestyle which also takes into account income and work–life balance, environment and other physical impairments.” Woman, 50–59 years
Thus, conversation about weight needs to begin with the rationale for broaching the topic and open-ended questions exploring a person’s level of comfort with discussing their weight, to guide the direction of subsequent discussions. For example:
- “We know that weight can affect diabetes management. How do you feel about us discussing this?”
If a person does not wish to participate in a weight-centric consultation, it is important to explore their preferences. While weight-loss goals (in the form of kilogram/pound reductions) may motivate some, others may find a shift away from numbers on the scale to a focus on healthful behaviours to be more suitable, and less stigmatising. There are numerous other metrics beyond kilograms and pounds for monitoring progress (Halton and Hu, 2004; Schneider et al, 2006; Jovanovski et al, 2020). Taking this approach may foster collaboration and provide the person with a sense of shared purpose (Ward, 2018).
2. Balanced communication
The participants in our study wanted their healthcare professionals to be understanding, kind and empathetic. Even those who sought a blunt or direct approach to weight management discussions wanted the message to be delivered with respect and compassion.
“They would be kind and say, ‘I know it’s hard to lose weight and that you probably don’t like the weight you are. Then we could work together to shed those extra kilos.’” Woman, ≥70 years
Ineffective communication may negate the impact of important clinical discussions and, in fact, may do more harm than good (Speight et al, 2021). Participants told us that some weight-related language used by healthcare professionals (e.g. body mass index) can be disparaging and traumatic. Indeed, recent studies have identified healthcare professionals as a source of both diabetes-related stigma and weight-related stigma experienced by adults with type 2 diabetes (Browne et al, 2013). Such stigma is associated with increased diabetes distress, depressive symptoms and lower-quality collaboration between the healthcare professional and the person with diabetes, as well as less frequent consultations and/or disengagement from healthcare (Puhl et al, 2020). This has been an important message in the #LanguageMatters movement in both the diabetes and obesity communities (Himmelstein and Puhl, 2021; Speight et al, 2021; Obesity Action Coalition, 2022).
“My previous GP had me in tears and feeling like my life was not worth anything because I hadn’t lost any weight. I had lost a small amount (3 kilos) and he was not satisfied that I hadn’t lost more. I felt useless and unworthy.” Woman, 40–49 years
Use of non-stigmatising language that avoids blame and shame is vital, and self-assessment of communication style and choice of language is recommended.
3. Quality advice
In addition to wanting their healthcare professionals to be experts in their field, participants wanted explicit and actionable advice. That is, not only what to do, but how to do it. This is consistent with behaviour change theory and research, and a commonly employed technique for increasing capability for change (Michie et al, 2011):
“[My healthcare professional would say] ‘I have a group walking around these [names] streets in the morning… walk at your own pace… and go around as often as you feel like… be sure to record your times and results at the starting pace [sic] before you leave. We start at 5.30 am.’” Man, 60–69 years
Examples of how health professionals can facilitate advice-giving include:
- “Let’s talk about what you are going to do to over the next few weeks.”
- “Let’s work out a plan that’s going to work for you.”
- “Together, let’s work out the specific steps you’re going to take to reach your goal.”
Whilst details and instructions were preferred, participants in our study gave numerous accounts of how, in their circumstances, good advice for someone else was not good advice for them. Similarly, prior qualitative research identified that this “one-size-fits-all” approach to diabetes management is perceived by adults with type 1 and type 2 diabetes as ineffective, inaccurate and inconsistent with person-centred care (Litterbach et al, 2020). Therefore, context is crucial. Weight-related advice is best tailored to individual circumstances, including financial, physical, social and emotional context.
4. Personalised weight management strategies
Participants wanted healthcare professionals to provide personalised strategies and interventions. Personalisation is achieved by taking into account an individual’s capabilities, opportunities and motivations (West and Michie, 2020). For example, it would be an error to assume that lack of motivation is the problem when lack of opportunity (e.g. access to safe walking tracks) may be the main barrier to increasing physical activity.
Reported negative experiences included healthcare professionals recommending a generalised rather than tailored approach to treatment, leading to dissatisfaction and missed opportunities for effective intervention, as illustrated by the quotes below:
“Discussion regarding what methods of exercise and activity work for me. Things that I can do on a daily basis to exercise that don’t take a lot of time.” Man, 50–59 years
“I would like to address the issue of my sore knees, but doctors usually dismiss that as an option ‘until you lose some weight’. The sore knees impair the ability to actually be as active as I want to be. Doctors don’t seem to realise this as an issue.” Man, 60–69 years
“As a vegetarian, I am constantly disappointed with the response of dietitians – replace the meat with tofu – thanks, that really helps!” Woman, 60–69 years
An effective intervention is one that is both acceptable and sustainable for the individual.
5. System-wide support
The participants in our study reported that they want to benefit from a multidisciplinary model of care, so if specific and detailed advice on a given issue is not possible, referrals to other specialists would be well received:
“[My healthcare professional would say] I would like to suggest you visit an endocrinologist to see if there is some way of finding out about your specific hormones and autoimmune issues that may provide some keys to improving your weight management.” Woman, 60–69 years
It is important to note that systemic issues may prevent timely access to specialist care (Greenwood-Lee et al, 2018), so managing expectations is needed regarding the wait-times for accessing specialist professionals.
Conclusion
Our published findings provide novel insights into the preferences of people with type 2 diabetes regarding weight management discussions in clinical care (Geerling et al, 2022). Informed by these data, we present five considerations for clinical care, with person-centred care underpinning individuals’ preferred approaches to weight management discussions. Showing respect, empathy and removing all judgement are important for building a trusting relationship to enable discussion of what can be a very sensitive issue. Asking for feedback and checking what has been understood signals to the person with diabetes that they are central to the care they receive, and provides an opportunity for healthcare professionals to ensure their communication is effective (Grocott and McSherry, 2018).
Acknowledgements
The authors thank the adults with type 2 diabetes who participated in the Your Story: Type 2 Diabetes and Weight Management study. We acknowledge Dr Jessica L Browne (formerly of The Australian Centre for Behavioural Research in Diabetes and Deakin University), who was responsible for initial project management, and Emerging Options Pty Ltd, who hosted the survey, collated the data and reported on the initial findings.
Funding
Ralph Geerling is supported by a Deakin University Industry PhD Scholarship, in collaboration with AstraZeneca Australia (unrestricted educational grant). AstraZeneca was involved in planning workshops that informed the design of the Your Story survey and data collection. The funding source had no role in the selection of the research question, data analysis or interpretation of the study findings, or in the decision to submit the manuscript for publication.
Elizabeth Holmes-Truscott and Jane Speight are supported by core funding to The Australian Centre for Behavioural Research in Diabetes (ACBRD) provided by the collaboration between Diabetes Victoria and Deakin University. Shikha Gray is supported by an unrestricted grant to the ACBRD from Diabetes Australia.
Conflicts of interest
No conflicts to declare.
Ethical approval
Ethical approval for the project was granted by the Deakin University Human Research Ethics Committees (research project number: 2015–074)






Case study outlining the complexities of managing glycaemia in a pregnant woman with type 1 diabetes.
30 May 2025