Having a child diagnosed with type 1 diabetes (T1D) can be a tremendous shock and is a life-changing event for the family (Madrigal et al, 2020). While 85% of children who are diagnosed have no family history of T1D (Juvenile Diabetes Research Foundation, 2022), some parents have the same condition. Through the experiences of four parents (two mothers and two fathers) whose children were diagnosed with T1D, this article explores and reflects on the themes that present when a parent with T1D has a child diagnosed with T1D, and how the paediatric diabetes team can meet the needs of these families.
Genetic predisposition
Research is yet to provide a definitive reason for why the immune system is triggered into attacking the pancreatic beta cells, leading to T1D (DiMeglio, 2018). It is, however, widely agreed that the person with T1D has a genetic predisposition to develop the condition and that an environmental trigger occurs prior to its onset (TrialNet, 2022). Statistically, a parent who has T1D having a child who develops it also is rare. According to Hämäläinen (2002), a child with a mother who has T1D has a 2% increased risk of being diagnosed with it. Interestingly, the risk increases to 8% if they have a father who has T1D. However, if both parents have a diagnosis, the risk of their child developing T1D increases to 1 in 4 (American Diabetes Association, 2022). Despite the infrequency of parental T1D, paediatric diabetes teams may encounter families in this situation.
The impact of diagnosis
Prior to their child being diagnosed with T1D, three out of the four parents in the study recounted that they had been informed of the increased chance that their child may develop the condition. However, owing to the low risk, they had not been concerned or thought about it until the day their child started to show symptoms. All of the parents discussed knowing their child had T1D before bringing them into A & E, where a diagnosis was made and their child’s diabetes journey began.
Nash (2013) suggested that following such a diagnosis, the family may go through the Kübler-Ross’s grief cycle (Kübler-Ross, 1997; Figure 1), as they mourn the loss of their healthy child and grow to accept their child’s new health condition. The grief cycle is sometimes referred to as the five stages of diabetes acceptance. It is proposed that the process of moving through the stages of the grief cycle allows the person to accept the diagnosis of diabetes over time, each person individually progressing through each step at their own pace (Bateman, 2018).
When discussing their child’s diagnosis, all of the parents appeared to describe going through the denial stage briefly, prior to bringing their child to hospital. This was followed by feelings of guilt that have stayed with them since their child’s diagnosis, and is something that they carry with them. One parent described feeling guilty that they had not noticed sooner that their child had T1D, whilst the other three felt guilty that they had passed on the genetic predisposition. One parent believed that they should have done more to protect their child from developing the condition, as they knew there was an increased risk.
Discussion of the grief cycle with the parents highlighted that some of the Kübler-Ross grief stages, such as anger, were not encountered. It appeared that they had moved to the final stage of acceptance more swiftly, compared to other parents who do not have T1D, which accords with the findings of Bowes et al (2009).
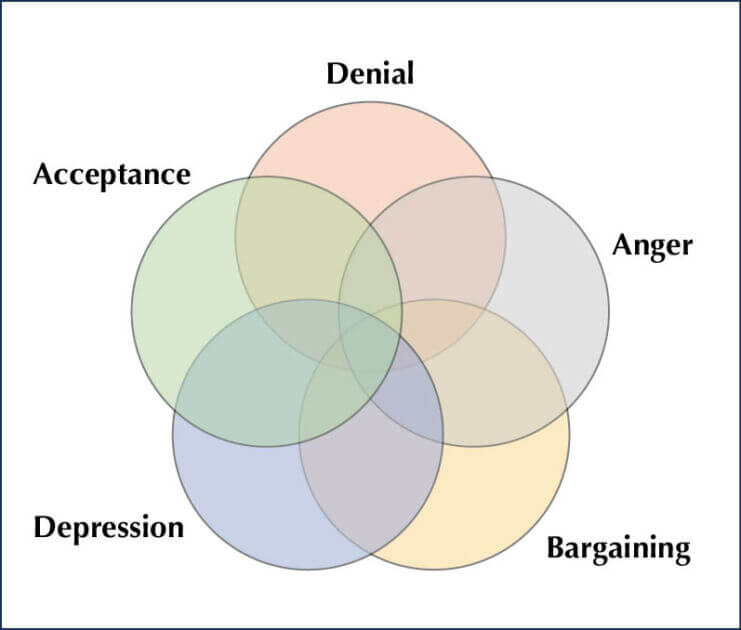
Figure 1. Kubler-Ross grief cycle stages.
Positive aspects for the family
The parents perceived that having a parent with T1D would make their child’s transition into their journey smoother, as their child already had some knowledge and experience of the condition. The parent’s viewpoint is reflected in a study by Hansen and Ersfjord (2021) that explored children’s experiences of parents with T1D.
Children can sometimes feel that those around them do not understand what it is like to live with T1D and can experience increased psychological distress compared to their peers (Delamater, 2018). Having a parent with T1D, however, can lead to a child feeling they have someone they can relate to and feel more understood (Freeborn, 2017). One parent felt that one of the benefits of their situation was that their child would not grow up feeling isolated by the condition like they had. Another affirmed that their child felt safe and secure knowing that their parent had the condition. A third parent expressed that their relationship had become closer since the diagnosis, and that they were in their own little diabetes bubble together.
When discussing the positives of their situation, one parent felt that their child having T1D made them improve their own diabetes management, as they wanted to be a positive role model for their child. Another echoed this sentiment, adding that it had improved their carbohydrate counting and that they were now, as a family, eating more healthily.
When reflecting on their child’s inpatient stay at diagnosis, each of the parents felt that they had a good baseline knowledge of T1D, which made the education from the diabetes team easier to understand. One parent felt the education they received acted as a refresher, such as for giving insulin injections (something they did not regularly do as they had an insulin pump), whilst they also learnt new information, such as how to administer glucagon.
While returning to school following a diagnosis of T1D can be an overwhelming and stressful experience for families and school staff (Bratina et al, 2018), one parent perceived that an added advantage of them having T1D was that they could give the school staff a greater insight into the condition. They could advise on appropriate responses to their child’s T1D, which enabled a smoother transition back to school.
Two parents believed their knowledge of the latest diabetes technology and the benefits associated with it provided an advantage for their child (Barnard et al, 2016). It enabled them to request glucose sensors and insulin pumps from the diabetes team quickly.
Challenges for the parents
Two parents reported that they had previously not allowed their diabetes to be the focus of their lives, but, following their child’s diagnosis, T1D now dominated them. One parent described themselves as “a bad diabetic”, while another stated that they had previously hidden their diabetes from people, highlighting that stigma and psychological complexities can be associated with the condition (Nishio and Chujo, 2017). One of the parents revealed that their child’s diagnosis was now a constant reminder that they had T1D, which was psychologically challenging for them.
Although the parents felt that they had accepted their child’s diagnosis quickly, they also perceived that it was harder to accept, as they knew the consequences and challenges of living with T1D. All the parents carried trauma from their own T1D journey, and they did not want their child to experience the same. Having a greater understanding of the daily challenges of living with T1D can lead to a greater negative psychological impact on the parent. One parent described themselves as “always being worried” about their child.
Since their child’s diagnosis, parents reported that their own T1D management had become more challenging and had been negatively impacted. This was attributed to the parent prioritising their child’s T1D needs. By focusing all their energy into managing their child’s T1D, they reported that they often neglected their own diabetes needs. Examples were given of forgetting to administer long-acting insulin or to take their diabetes supplies out with them. One parent also noted missing their own diabetes clinic appointments, as they could not get time off work to attend both their child’s and their own appointments.
How can the diabetes team provide support?
Following a diagnosis of T1D, the diabetes team should provide support and education that is tailored to the individual family’s needs (NICE, 2023), as personalised care leads to better health outcomes (Williams, 2022). The point of diagnosis is a key time in the family’s diabetes journey and can impact on future health outcomes (Dunning, 2012). Therefore, it is imperative that the diabetes team is empathetic, non-judgemental and supportive, using the principles of Language Matters (NHS England, 2018), whilst also providing diabetes education that is pitched at the correct level and pace for the family (Phelan et al, 2018).
Parent reflections highlighted that it is paramount that healthcare professionals do not make assumptions about the knowledge or confidence of the parents at diagnosis, especially with the parent who has T1D. One parent felt that presumptions were made by ward staff, who knew they had T1D, leading to feelings of unnecessary pressure and expectation that resulted in the parent feeling embarrassed to ask for advice or assistance from ward staff.
The diabetes team should acknowledge that the parent with T1D will bring their own personal experiences, which will influence their ability to manage their child’s T1D and engage with staff. All the parents in the study recalled psychological trauma related to their diabetes. Exploration of the parent’s relationship with their own diabetes may be beneficial for the team in order to gain insight into the wider dynamics within the family.
Parents felt that a holistic approach from the team was essential, and helped to build a positive therapeutic relationship between the family and the diabetes team (Mills, 2017). Comparing their child’s clinic appointments to their own, one parent noted that the consultation styles were very different. Reflecting the opinion of others, one parent felt that their own diabetes appointments lacked active listening from the doctor and, overall, was not a positive experience due to feelings of judgement (Phillips et al, 2020). Praise was given to the consultation style at their child’s clinic appointments, which emphasises the importance of keeping them positive and non-judgemental, and allowing the family to discuss the issues that are most pertinent to them (Odiase et al, 2020).
Owing to the nature of the condition, it is unsurprising that there is a high prevalence of diabetes distress in the T1D adult community (Kiriella et al, 2021). Distress amongst parents caring for children with T1D is also common (Noser et al, 2019). It is key that the diabetes team considers that a parent may be facing a combination of diabetes distress from not only their own condition, but also their child’s. All parents reported they had experienced diabetes psychological distress. Consideration of the added pressure on parents is imperative, as failure to acknowledge parental distress and burnout can impair their ability to manage their child’s diabetes and engage with the diabetes team (Helgeson et al, 2012).
Diabetes teams can support families by discussing their emotional health routinely at their appointments, and assessing for diabetes distress (Fisher, 2019). It has been suggested that by using a family-centred care model, diabetes teams can address diabetes burden and burnout, and support families to manage the psychological challenges of T1D (Abdoli et al, 2020).
The team can also utilise the 7 As model (Diabetes UK, 2019), which can easilty be applied to practice, to aid in the assessment of psychological needs and implementation of help and support within a person-centred approach.
Conclusion
This exploration of parental experiences and opinions following their child’s diagnosis of T1D sought to highlight the needs of parents who also live with T1D. Discussions with four parents highlighted that they experience additional pressures and challenges compared to parents who do not have the condition. However, the parent’s and child’s diagnoses of T1D bring many positives to the family situation, and all of the parents demonstrated fortitude and resilience in their own and their child’s diabetes journeys. Diabetes teams need to acknowledge the strengths of a family and the challenges they may face in their diabetes journey, and seek to support their needs by utilising all members of the diabetes team, especially the team psychologist.
There is minimal research into this subset of families. It would be helpful to conduct a multi-centre, qualitative research study on families in which both a parent and child have T1D. A larger study could explore and build on previous themes, dissecting the specific needs of the families and evaluating how diabetes teams can provide support and potentially improve their practice.
Acknowledgement
The author would like to thank the Children and Young People’s Diabetes Care Module, Birmingham City University, for its support in the writing of this article.





Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025