Blood glucose monitoring is a common procedure in type 1 diabetes care. Evidence has shown that frequent capillary blood glucose monitoring is directly related to better glycaemic control, prevention of long-term complications and better health outcomes (JDRF Continuous Glucose Monitoring Study Group, 2011; Miller and Dimatteo, 2013). Thus, blood glucose monitoring should be encouraged in type 1 diabetes self-management.
Nurses are members of the multidisciplinary healthcare team and are protagonists in teaching and guiding the technique of self-monitoring of blood glucose (SMBG) for children with type 1 diabetes and/or their families. Generally, nurses teach the technique to family members first and family members teach their child later. Teaching of SMBG involves several steps (Diabetes UK; Sherr et al, 2018), among which is teaching the sequence of procedures.
Some studies have highlighted certain characteristics of child development, correlating them with a child’s readiness to perform SMBG (Borzekowski, 2009; Chiang et al, 2018; Children’s of Alabama). According to child cognitive development stages, in children aged 2–7 years, symbolic thinking emerges, mental reasoning grows and the use of concepts increases. Between 7 and 11 years, children develop skills in physical, social and academic fields, gaining more autonomy, although they still require adult supervision in diabetes care (Borzekowski, 2009; Chiang et al, 2018).
At the time of conducting this study, we have not identified any published protocol that standardises SMBG technique, especially with respect to the paediatric population. Likewise, there is no evidence to prove that the SMBG technique used by adults can be reproduced by children. Therefore, there is a need to identify the steps of SMBG in the paediatric population, to offer healthcare teams, children and their families an evidence-based technique that respects the uniqueness of the child development process.
This review aimed to identify and synthesise studies that gathered evidence on SMBG technique in children with type 1 diabetes. We sought to provide recommendations to support future research, education and clinical practice focusing on paediatric SMBG. The following research question guided this review: What is the evidence in the scientific literature about the steps of SMBG technique for children with type 1 diabetes?
Method
Study design
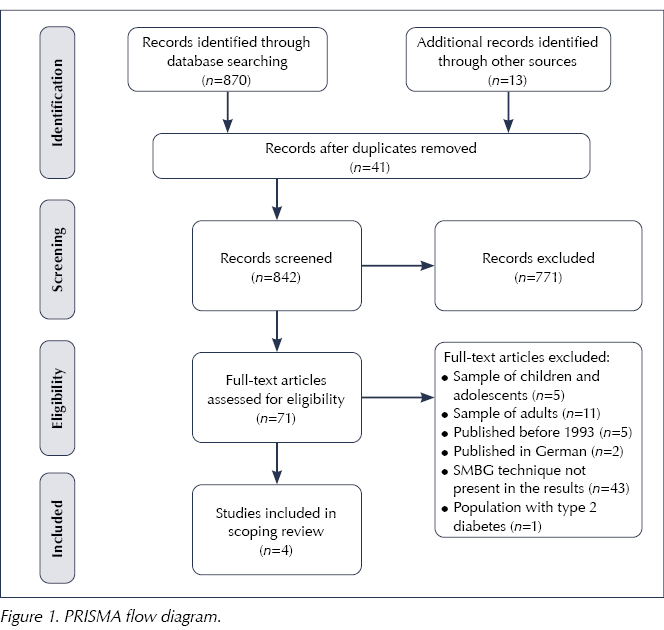
This scoping review was conducted following these steps: identification of relevant studies, selection of studies, data mapping, extraction, summary and report of results (Arksey and O’Malley, 2005). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) was used to guide this review and its report (Moher et al, 2009; Tricco et al, 2018).
Information sources
Searches were performed in seven databases: PubMed, CINAHL, EMBASE, LILACS, SCOPUS, Web of Science and The Cochrane Library. The searches were limited to studies published between January 1993 and December 2019, in English, Spanish, French or Portuguese. The year of publication of the Diabetes Control and Complications Trial (DCCT) was the parameter used to define the initial publication date (DCCT Research Group, 1993).
The search strategy was developed using the PCC (Population, Concept and Context) tool (Peters et al, 2020), and search terms were adapted to the specificity of each database. A combination of descriptors and keywords were used with Boolean operators (Appendix 1).
To identify the grey literature, manual searches were conducted on the websites of paediatric and endocrinology associations, such as Diabetes UK, the International Diabetes Federation, the American Association of Diabetes Educators, the International Society for Pediatric and Adolescent Diabetes, Diabetes Australia and the Brazilian Diabetes Society. In addition, the reference lists of the included studies were manually reviewed.
Eligibility criteria
Qualitative studies, quantitative studies, reviews and grey literature about SMBG technique for children up to 12 years old diagnosed with type 1 diabetes were included. Studies on SMBG technique with glucose sensors (linked to insulin pumps or not) and studies with adolescents included in the same sample were excluded.
Selection of sources of evidence
Two reviewers (MdL and ACABL) used the Rayyan platform (Ouzzani et al, 2016) and independently screened all studies considering the eligibility criteria. Three diabetes experts were consulted to validate the decisions.
Synthesis of results
Data extraction was conducted according to the recommendations of Arksey and O’Malley (2005). Extracted data were: authors, year of publication, study origin, objective, method, participants, steps and materials used in SMBG technique, study limitations and main conclusions. Data were descriptively analysed by two authors and validated by the entire research team.
Results
Systematic searches in the databases identified 870 potential articles. Unsystematic searches identified a further 13 potential records. After excluding 41 repeated articles, 842 records were screened by their titles and abstracts. Seventy-one records were fully read, resulting in four studies that met the inclusion criteria and composed the final sample of this review (Figure 1).
The reviewed articles included a quasi-experimental study (Kaneto et al, 2018), a cross-sectional study (Perwien et al, 2000) and two patient guides (Dumas et al, 2004; Advance for Nurse Practitioners, 2005). The studies were published between 2000 and 2018, and were developed in the US (Perwien et al, 2000; Advance for Nurse Practitioners, 2005), Brazil (Kaneto et al, 2018) and France (Dumas et al, 2004). Studies included a total of 299 children, aged 6–12 years, of whom 145 were male and 154 female. Two studies reported participants’ mean HbA1c: 71 and 76 mmol/mol (8.6% and 9.1%), respectively (Perwien et al, 2000; Kaneto et al, 2018).
In one of the studies, an educational workshop was held based on recreational activities on the same day as the outpatient appointment (Kaneto et al, 2018). Four stations were organised, including activities with questions related to SMBG: storytelling and puzzles, a bingo game, a memory game and a board game. Activities were carried out in private rooms and the researcher asked the children to perform the SMBG technique in the same way they did at home, without offering any instructions at that time. Data were collected immediately before the workshop and 4–6 weeks after the workshop. At the end of the study, frequency of SMBG, changing of lancets, alternation of the puncture and calibration sites, and periodic checking of the meter and date settings improved, demonstrating the effectiveness of the workshop.
The cross-sectional study presented data from a summer camp for children with type 1 diabetes (Perwien et al, 2000). One researcher observed children performing SMBG. Errors and successes, including 15 behaviours, were assessed in a skill test previously prepared by professionals specialised in diabetes. After being observed, children were corrected and instructed to perform the test again if they had made a critical mistake.
SMBG technique and supervision
Figure 2 summarises the steps of the SMBG technique in children, according to the evidence presented in the four studies included in this review.

The child’s developmental stage must be taken into account when teaching and supervising the SMBG technique. Younger children need to be monitored more carefully because the younger they are, the fewer skills they will have in performing the SMBG technique. Moreover, boys need to be monitored until a later age compared with girls, because girls showed better performance than boys (Perwien et al, 2000).
Adult supervision should also be closer when the child starts the SMBG routine with a new glucometer. Perwien et al (2000) showed higher performance in SMBG technique by children who used the same type of glucometer at home and in data collection. Similarly, supervision of SMBG should be even more attentive when children show signs of hypoglycaemia, as hypoglycaemic children tended to perform worse than those who did not experience this complication (Perwien et al, 2000).
Discussion
This review describes the steps for SMBG performed by children aged 6–12 years. The selected studies had different designs and were published over an 18-year period. The studies showed the evolution of research on SMBG in children with type 1 diabetes, from “patient guides” in 2004 (Dumas et al, 2004) to quasi-experimental studies in 2018 (Kaneto et al, 2018).
Children can perform SMBG without the direct help of an adult but they must be adequately supervised. Failure to perform each step of SMBG correctly can bring consequences. Children can intentionally or accidentally modify the glucometer data, resulting in errors that can be harmful to the child (Marks and Wolfsdorf, 2020).
Handling of peeled fruits, such as bananas, apples and oranges, can leave traces of fructose and glucose on children’s fingertips, resulting in incorrect readings by the glucometer, overestimating the capillary glucose level (Arakawa and Ebato, 2012; Olamoyegun et al, 2016). In addition, newspaper print, perfumes, hand creams and hair gels can also be sources of errors in blood glucose readings (Gordon, 2019). In these situations, washing hands with soap and water provides security for safe reading (Arakawa and Ebato, 2012; Olamoyegun et al, 2016). In our review there was no consensus on the best method for hand hygiene before SMBG. However, guidelines in infection control recommend hand sanitiser in cases when soap and water are not available (Centers for Disease Control and Prevention, 2020). Nurses must teach children with type 1 diabetes the importance of hand hygiene regardless of the method used.
Other factors that can affect the results of SMBG are failure to handle the system according to the manufacturer’s instructions, incorrect maintenance of the glucometer, the use of expired test strips or incorrect storage of strips, and an inadequate amount of blood on the test strip, which can lead to false low readings (Nerhus et al, 2011; Gordon, 2019). Extreme temperatures and rapid changes in temperature, such as moving from the outside to the inside of a house during winter, can also affect the accuracy of results obtained with SMBG (Nerhus et al, 2011).
The steps of the SMBG techniques are synthesised in this review; however, due to current advances in technology, some of these steps may already be outdated. These include checking the code of the glucometer and bottle of reagent strips shown in step 3 of the results. Currently, modern devices do not use this code system. With each tube of new strips or with the suspicion that the meter or strips are not working properly, the user performs a test with a control solution to confirm that the strips are reading correctly (Accumed-Glicomed, 2018). The control solution contains a known amount of glucose that reacts with the test strip.
Factors should be considered when choosing and purchasing the ideal glucometer, such as ensuring that the meter is suitable for the particular environment, for personal rather than laboratory use, the ease of use, quality seal, the size of the device and the blood sample required (the smaller the better), the price of the test strips, the accuracy of the test and the ease of cleaning (Advance for Nurse Practitioners, 2005; Gordon, 2019).
In addition, step five presented in this review shows how to place the blood on the test strip and then fit the strip in the meter. For the more modern glucometers, the recommendation is to insert the reagent strip in the meter and then turn on the device. Thus, a blinking blood-drop icon will appear on the screen, indicating that the meter is ready for blood collection (Johnson & Johnson, 2017). There are controversial data from studies included in this review about the amount of blood that should be used to measure blood glucose. Perwien et al (2000) indicated a “large” blood drop, while Kaneto et al (2018) described a “sufficient” amount. At present, an amount of blood with a volume equivalent to 0.5 µL is indicated. Excessive amounts of blood can cause the meter to malfunction by polluting it (Accumed-Glicomed, 2018).
Our results indicate that families should contact a hospital waste company to send a sharps container for lancet disposal. However, this is not financially feasible for many people with diabetes in many countries. Patients can dispose of needles and lancets in any hard plastic capped bottle and bring this to the nearest health service.
It is evident from this review that there is a scarcity of studies about the education of children aged up to 12 years on SMBG technique. Children must learn the technique at a certain age, but the literature is deficient in showing how best to introduce children to SMBG care, a procedure that will have been present in their lives since diagnosis. Studies indicate that school-age children are already performing the technique on their own, yet there are no direct guidelines for them (Kelo et al, 2011; Koller et al, 2015).
Conclusions
This scoping review identified four studies that describe the steps of SMBG technique in the paediatric population with type 1 diabetes. The limited number of studies highlights the knowledge gap in this area and alerts us to the need to base nurses’ educational practice on children’s needs.
Education about SMBG must be continuous and high-quality. The low number of studies identified indicates the need for research in the paediatric area, the development of paediatric materials, and explanations about SMBG that are suitable for each age group. In addition, research should support the production of educational resources for healthcare professionals and diabetes educators, with a view to promoting children’s autonomy in carrying out the procedure safely.





Charity publishes its 10-year vision to transform diabetes prevention, care and treatment.
22 May 2025