In spite of significant medical advancement in care, diabetes remains a growing global concern. The estimated global cost of diabetes in 2015 was US$1.31 trillion (Bommer et al, 2017), and the American Diabetes Association (2013) states that the increase in the cost of treating type 2 diabetes could outgrow the national gross domestic product of some countries unless this is addressed. Similarly, the cost of prescribed antidiabetes drugs in the UK rose from £572.4 million to £983.7 million between 2006/07 and 2016/17 (NHS Digital, 2017). Apart from the organisational healthcare costs, diabetes is a lifelong condition that affects people from all socioeconomic backgrounds, and it has a significant impact on the physical, social, economic and psychological wellbeing of the affected people (Lawal, 2016; Public Health England, 2018).
Several studies have identified the benefits of diabetes education in promoting self-care abilities and reducing preventable complications. Diabetes education programmes improve individuals’ knowledge of diabetes, reduce complications and hospital admissions, and promote healthy lifestyles (Davies et al, 2008; Rygg et al, 2012). Therefore, a key global healthcare policy response has been to emphasise empowerment through education. Structured patient education forms part of the World Health Organization (2016), National Service Framework for Diabetes (Department of Health, 2001) and NICE (2017) recommendations for managing diabetes.
Although it is acknowledged that diabetes services in the UK and other parts of the world are improving, there is a need for further improvement, particularly in promoting structured patient education. The statistics show that people with diabetes often fail to attend the structured education sessions for a range of reasons (Schäfer et al, 2013; Winkley et al, 2015; Lawal, 2016). Two recent systematic reviews conducted on this phenomenon identified limited studies and established the need for further research on this topic (Lawal, 2014; Horigan et al, 2017). Therefore, the current study was conducted to contribute insights into barriers that may hinder the uptake of structured diabetes education.
Methods
Research design
In bridging the identified gap in research on this problem, this second-phase study was designed as a follow-up to explore the findings from a series of focus group interviews with healthcare professionals (Lawal et al, 2017). To address the research question, the authors used one-to-one telephone interviews with people with newly diagnosed diabetes who did not attend a diabetes education programme after referral.
Sample and setting
In accordance with the UK national diabetes management policy, all newly diagnosed people with diabetes are referred to attend diabetes education sessions. The participants were recruited through the hospital database of these newly diagnosed people. They were drawn from four diabetes education centres with different demographic characteristics and high attrition rates in south east England. The study employed a convenience sample of participants who were willing to volunteer information. In total, 102 people were approached to take part in the study but only 24 consented, for various reasons listed in Box 1. Each telephone number was called three to five times.
Data collection procedures
Semi-structured interviews were conducted by an experienced researcher with a written guide to facilitate discussion on the topic of barriers and enablers to attendance at diabetes structured education. The question guide was developed based on the literature review and data generated from phase 1 of the study (Lawal, 2014; Lawal et al, 2017). The investigator conducted the one-to-one interviews by telephone in an office within the hospital Trust, and each interview lasted between 5 and 10 minutes. The researcher used a conversational style and recorded answers to questions regarding participants’ personal characteristics.
Ethical implications
The research followed the principles outlined in the Declaration of Helsinki and was conducted according to the ethical codes guiding research in Great Britain. Ethics approval was granted by Berkshire Research Ethics Committee and permission was received from the Clinical Research Development Unit of Berkshire East Primary Care Trust. Similarly, each participant’s consent was sought at the beginning of each telephone interview.
Data analysis
The researchers performed thematic analysis to identify barriers to attendance using an inductive approach to build a descriptive narrative of the phenomenon (Polit and Beck, 2012). Coded data were analysed to identify themes and subthemes to illustrate the issues affecting attendance.
Results
Twenty-four people contributed their views during a one-to-one telephone interview. All participants were 40 years of age and older, with a mean age of 52.9 years (range, 44–68 years), and included men and women. All participants were newly diagnosed with diabetes; the duration of diabetes was 1–2 years and the mean time since diagnosis was 1.2 years. There were slightly more male participants than female (13 male, 11 female). The study population comprised people from different ethnic backgrounds: 12 Caucasian (50%), eight Asian (33%) and four African/Caribbean (17%).
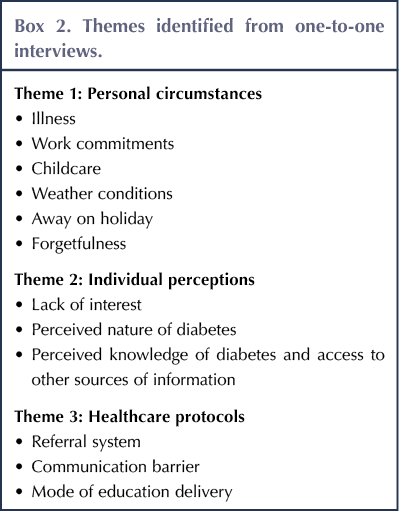
Quotes are provided as examples of each participant’s responses. Based on thematic analysis, the main areas of findings are discussed under three broad themes, as shown in Box 2.
Theme 1: Personal circumstances
An individual is unique and our circumstances differ at different times. In this study, participants divulged various personal difficulties and barriers to attendance, which will be discussed under the following subthemes.
Illness
Being ill during the allocated time was mentioned by the participants: “I was very poorly and cannot attend” (Interviewee 11); “I was sick and couldn’t come because I had bronchitis” (Interviewee 19); and “I am not well enough to attend the session” (Interviewee 6).
Work commitments
Some of the interviewees attributed their reason for non-attendance to work-related problems: “It was in the afternoon and I went to work and got caught in the traffic” (Interviewee 5); and “I was working on that day” (Interviewee 4).
Childcare
Some participants cited childcare issues as the reason that prevented them from attending the session: “Sometimes I have to attend to my grandchildren because my daughter is working” (Interviewee 10).
Weather conditions
A few respondents stated that they could not attend due to unforeseen circumstances, such as bad weather: “You will find that day was a bad day and most people couldn’t go out because it was snowing heavily” (Interviewee 17).
Holiday
Some respondents were out of the country during the planned sessions; therefore, it was impossible to attend the sessions: “Gone to Australia for 1 month” (Interviewee 7).
Forgetfulness
Some participants identified forgetfulness as the reason for their non-attendance: “Sorry, I forgot about it completely” (Interviewee 16); “I did not remember at all” (Interviewee 22); and “I messed up really because I’ve got problem at work then” (Interviewee 14).
Theme 2: Individual perceptions
Lack of interest
Absence of the desire to attend the education sessions for certain personal beliefs or behaviours was revealed by the data: “I don’t really want to come because I am fine” (Interviewee 3); “I am not interested” (Interviewee 20). Some participants showed complete lack of interest in the session: “No, I am quite happy even if I don’t know everything. No thank you. It was unnecessary and I don’t know why they are bothering me” (Interviewee 13); and “Nothing in particular” (Interviewee 2).
Perceived nature of diabetes
Considering the time since diagnosis, some respondents did not attend because of their personal perception about the seriousness of diabetes: “I am really pre-diabetic and I have taken some test and I am no longer pre-diabetic” (Interviewee 24). In a similar way, some respondents did not attend because they had the opinion that they were all right: “I am quite comfortable” and “My diabetes is well controlled” (Interviewee 3); and “I am doing everything right and my blood sugar level is okay” (Interviewee 23).
Perceived level of knowledge and access to other sources of information
Some respondents demonstrated lack of interest by saying: “Also, my son-in-law knows a lot about it because he is a health professional” (Interviewee 15). Another respondent stated that he could find out more information from other sources: “I can find out more information on the internet” (Interviewee 15).
Theme 3: Healthcare protocols
Some of the respondents identified certain administrative constraints that hindered their attendance, as follows.
Referral system
Some respondents stated that: “I didn’t because I couldn’t find my way, ehm, I mean I got lost because I trekked” (Interviewee 1); and “I was due to go to one earlier and I cancelled it and nobody contacted me” (Interviewee 9). The interviewees shed more light on this issue by stating that the invitation was by telephone in some cases and adequate information to guide their attendance was not given: “No, I didn’t have a letter to specify the place; it was a telephone message from a lady” (Interviewee 1); “I did not attend because I didn’t get a letter” (Interviewee 2); and “No, unfortunately, I didn’t get a letter” (Interviewee 8).
Communication barriers
When asked whether they were willing to attend the session next time, most of the interviewees stated they were willing to attend based on the current information. This suggests that adequate information may aid attendance. Some of the illustrative quotes are thus: “Yes, if I can get a letter, then I would attend” (Interviewee 1); “I have been expecting someone to call me to book me for another session but that has not happened” (Interviewee 9); “Please can you give me the appointment line” (Interviewee 8); “Yes, I would be happy to attend another session if I know about it” (Interviewee 17); and “Yes. If I am not working. That means if I can be given some dates in advance” (Interviewee 18).
Mode of education delivery
Most participants had no issue with attending group, as opposed to one-to-one, education and this was verbalised thus: “No, that would not be a problem” (Interviewee 2); “Yes, it is fine by me” (Interviewee 4); “No, I don’t have any problem with that” (Interviewee 12) and “It would be interesting to have people with the same problem sharing their experience” (Interviewee 21). Two participants expressed their flair for group education by saying: “I was not aware before but that’s fine. Even if I am late, I would join – just be part of the group. You get to learn from other people as well and I have attended similar sessions in the past” (Interviewee 5); and “It will be good to hear information from other people to help each other” (Interviewee 14). One participant stated that he would need to attend the session before offering an appropriate comment on this question: “Ehm – I don’t really know because I have not been yet. So I need to attend to find out more” (Interviewee 19).
Discussion
Compliance, adherence and concordance are popular terms in care management, and these concepts are applicable to health education. Concordance with self-care education is important in preventing complications and promoting health.
Participants in our study were aged 44–68 years, with a mean age of 53 years. Epidemiological evidence has shown that type 2 diabetes is common among this age group (Brashers et al, 2016). Our study showed that the attrition rate was influenced by various personal-life problems, ranging from work-related issues to childcare problems and ill health. Gucciardi (2012), Winkley et al (2015) and Lawal et al (2017) have all identified conflicting personal circumstances to be a barrier to attendance, and this is congruent with the findings of this study. These findings confirm the importance of considering these personal problems and demographic characteristics when providing necessary interventions.
Our findings revealed that some respondents did not attend because of their perception about the level of diabetes knowledge they possessed, or because they believed they could gain sufficient information by searching the internet or through family discussions. This result corroborates the findings of Winkley et al (2015), who found lack of perceived benefits of diabetes education to be a barrier to attendance. Diabetes has a genetic predisposition (Brashers et al, 2016), so individuals with diabetes are likely to have a relative with the condition. Additionally, the duration of diabetes could be a contributory factor due to lack of understanding about the progressive impact of beta-cell dysfunction (Brashers et al, 2016). Although informal education is increasingly becoming a key source of health education, it has its flaws (Lawal, 2016). Consequently, it is important to reinforce the superiority of structured education and the short- and long-term complications of diabetes.
Our data suggested that some participants were not at all interested in structured education, while others claimed to have forgotten about it. It could be argued that the latter group used forgetfulness as an excuse to cover their lack of interest, but this forgetfulness could equally have been due to old age, the added stress of recognising the severity of the condition, or other personal or family issues in their life at that time (Lawal, 2016). It could also be due to stigma, as stigma and shame contribute to lack of uptake of diabetes education in some people (Winkley et al, 2015). Whilst it can be assumed that people need to rearrange their appointments if they cannot make them due to circumstances such as a bad weather or a holiday, an individual who is ashamed is unlikely to make such effort.
Interestingly, this study showed that the group nature of structured education was not a barrier to attendance for people with diabetes. This is in contrast with the perceptions of structured education providers, who believed that group education could be off-putting for some (Lawal et al, 2017). Some studies have compared the benefits of individual versus group diabetes education, with conflicting results (Gucciardi et al, 2007; Duke et al, 2009); however, NICE (2017) recommends that individual preferences for either group or individual education should be considered.
This research showed that a poor appointment system with ineffective practitioner–patient communication has a role to play in non-attendance. The impact of poor communication on healthcare practice is well documented in the literature and this finding is consistent with other studies (Gucciardi et al, 2012; Winkley et al, 2015; Lawal et al, 2017). These results suggest the need to improve appointment and referral systems. In relation to communication with people with diabetes, NHS England (2018) has recently set out principles of good practice, which emphasise a collaborative and engaging communication style.
Other authors have identified several measures that can improve attendance rates. These include improving referral and appointment systems, offering flexible options for time and location, and reducing waiting times between referral and attendance (Winkley et al, 2015; Lawal et al, 2017). Pender (2016) states that offering a taster session, informing employers about the impact of diabetes, raising awareness and providing a straightforward invitation can help to improve attendance. In addition, it is important for practitioners to be aware that diabetes-related stigma exists among some individuals (Winkley et al, 2015).
Study strengths and limitations
Strategies were employed to enhance rigour and to minimise researcher bias through verbatim representation of views. Saturation was achieved at a point that no new barriers were forthcoming (Polit and Beck, 2012). In conducting research of this nature, access to participants can pose serious difficulties; therefore, a key limitation of the study was the use of the convenience sampling technique. To mitigate this, the study’s population was drawn from four diverse geographical areas with different demographic characteristics.
Conclusion
The national and international response to diabetes prevention includes empowerment, and structured patient education has a proven part in this. Nevertheless, it is important not to assume that people will automatically attend a referral from a medical professional just because it is beneficial for them. Instead, healthcare providers and educators need to identify additional support that people with diabetes may need to ensure attendance after invitation.
The findings of this study elucidate the barriers to successful education for people with diabetes, which include the individual’s circumstances, motivation, perceptions and beliefs, as well as the method of invitation and referral. The findings also suggest that the way practitioners provide information, follow up with patients and support them could aid attendance.
A better understanding of the barriers could facilitate the design of appropriate interventions to mitigate them. Therefore, we recommend further study to investigate the motivating factors of people who have attended structured education, because data triangulation may contribute to better understanding of this phenomenon.






Developments that will impact your practice.
29 Aug 2025