More than 4.9 million people in the UK have diabetes (Diabetes UK, 2021). All adults with type 1 diabetes and some with type 2 diabetes are reliant on insulin treatment to manage their condition. The number of older, frail, and comorbid people with diabetes requiring insulin therapy is also increasing, and many are reliant on community services for the provision of this crucial intervention. This has resulted in additional pressure on already overstretched District Nursing workloads, especially on the background of the COVID-19 pandemic.
To manage this demand, appropriately trained and competency-assessed health and care workers (HCWs), including health support workers and healthcare assistants, have been identified as capable to perform the delegated task of insulin administration to those people with diabetes whose glycaemic control is stable. NHS England and NHS Improvement (NHSE and NHSI, 2020) published a voluntary framework for teaching and training HCWs to administer insulin to adults with type 2 diabetes who are unable to perform this task themselves and have no family or unpaid carer who can do it for them.
Prior to the launch of the NHSE and NHSI framework, joint working led by East Sussex Healthcare NHS Trust with Sussex Community NHS Foundation Trust resulted in the drafting of a guideline to build upon a successful pilot of insulin delegation in care homes and District Nursing, which had been carried out in October 2019 and covered the delegation to appropriately trained HCWs in residential/care homes of insulin administration using pens to adult persons with diabetes in the community who have either type 1 or type 2 diabetes.
The outcomes of the pilot and subsequent development of the guideline gave key stakeholders assurance that investing in the wider roll-out of insulin delegation was safe for patients, had the necessary clinical governance and was worthwhile in terms of net efficacy savings. Scope and accountabilities were clearly defined within the guideline, specifying the duties and responsibilities of the HCW’s employer, the Head of Community Nursing, the Registered Nurse responsible for delegating the task and the HCW, in line with recommendations from the NHSE/NHSI voluntary framework.
The Registered Nurse was defined as accountable for the delegation of any aspects of the task and ensuring the individual was competent to carry it out, in line with Item 11 of the Nursing and Midwifery Council (NMC, 2018) Code. This included ongoing assessment and supervision of practice. The HCW was defined as the person to whom the task of administering insulin was delegated, either a non-regulated role (e.g. a healthcare assistant or equivalent health support worker in social care settings), an Allied Healthcare Professional or a Healthcare Scientist. The HCW was defined as accountable for ensuring that they did not take on this extended role until they had been trained and assessed as competent by the named Registered Nurse, and for ensuring that the delegated task was undertaken as per the document, in addition to ensuring their knowledge and competence was reviewed every 6 months.
This article presents the outcomes of this pilot and the learnings and recommendations derived.
Rationale
It is well recognised that District Nursing teams are under increasing pressures. Through our pilot, we have demonstrated that the safe delegation of insulin to HCWs has released capacity of District Nurses, reduced unnecessary delays in delivering insulin to people living with diabetes, and improved cross-sector working across community nursing, diabetes specialist teams and Medicines Optimisation in Care Homes (MOCH), as well as empowering the role of care homes, improving the quality of care for patients and increasing the resilience of our shared community workforce. This is outlined through quantitative data and qualitative feedback from staff and service users.
Definitions
For the purpose of the pilot, the following terms are used:
Insulin delegation: The process by which a Registered Nurse allocates the task of insulin administration to a named, competent, non-registered HCW (Diabetes UK, 2016). Only trained and competent staff should be responsible for administering insulin or monitoring blood glucose levels. Where a person’s diabetes care is stable, a care worker could complete this activity as a delegated task (Care Quality Commission, 2021).
Insulin administration: A subcutaneous injection of insulin using a pen.
Registered Nurse: The person who delegates the task of administering insulin to another HCW, based on their professional judgement, and acts as their assessor. Their name should be listed on Part 1 of the register of the NMC. The Registered Nurse is professionally accountable for the delegation of the task (NMC, 2018).
Health and care worker (HCW): The person to whom the task of administering insulin is delegated, in a non-regulated role (e.g. a healthcare assistant or equivalent health support worker in a social care settings; NHS England, 2020).
Patient criteria for insulin delegation
Table 1 explains the inclusion and exclusion criteria for people with diabetes to be considered for delegated insulin administration.

Duties and responsibilities
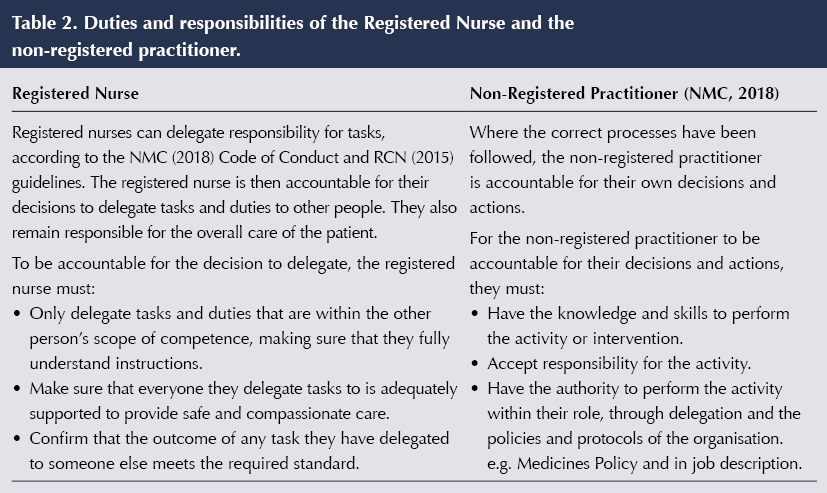
Table 2 lists the duties and responsibilities of the Registered Nurse and the non-registered HCW.
Essential training requirements
Delegated HCWs had to be compliant with the mandatory training required by their employer organisations. To accept the delegated task of insulin administration, the HCW must also have completed the Diabetes in Healthcare online education from Diabetes UK and the Six Steps to Insulin Safety module from the Primary Care Diabetes Society. Furthermore, the task could only be delegated once competency was signed off by an experienced Registered Nurse, who then acted as a mentor.
Following completion of the e-learning, the HCW was required to:
- Have knowledge of the diagnosis and treatment of both type 1 and type 2 diabetes.
- Be able to demonstrate the correct procedure for performing blood glucose monitoring.
- Be able to describe the effect of insulin on blood glucose levels.
- Administer insulin using the correct injection technique.
- Have knowledge of hypoglycaemia and hyperglycaemia, and appropriate treatment.
The pilot
Fourteen care homes and one respite care service in East Sussex were included in the pilot, which started in October 2019. Of the 17 homes that could potentially have participated in the pilot, one was unable to participate as the resident with diabetes had unstable diabetes control, and one did not have governance in place to facilitate delegation.
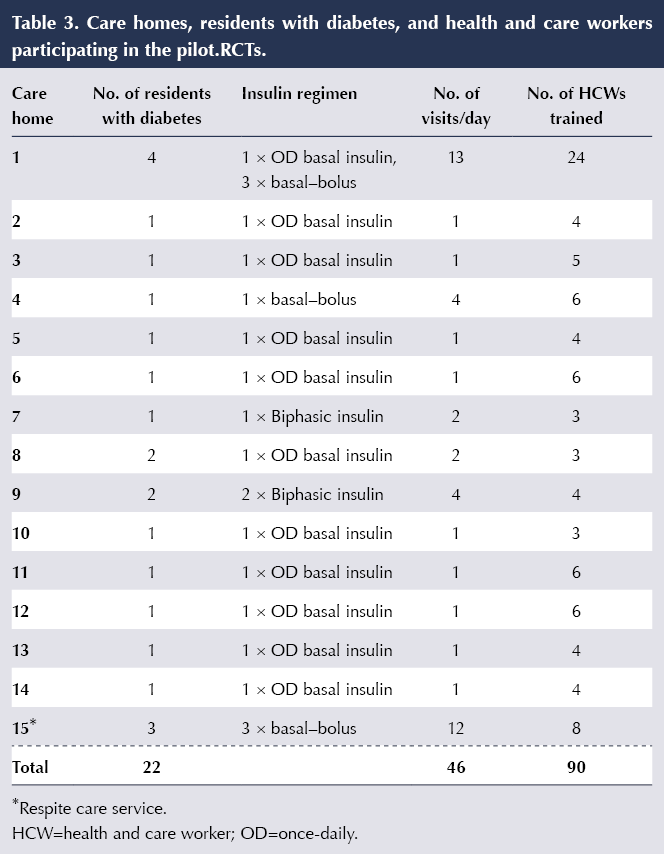
The participating homes had residents with diabetes under the caseload of the District Nursing team, and they were visited at least daily, and up to four times daily depending on their insulin regimen, for the administration of their insulin and blood glucose monitoring. A total of 22 residents with diabetes were identified following a review that satisfied the inclusion criteria for the pilot, requiring a total of 46 daily visits by the District Nursing team to administer insulin. Table 3 lists the care homes with the number of residents with diabetes, their insulin regimens, and the number of visits and number of HCWs trained.
For the people with diabetes who had the capacity to consent, this was sought verbally and documented on their notes. For those lacking capacity, this was discussed and agreed with their next of kin or through a best interest meeting, and documented accordingly by the care home.
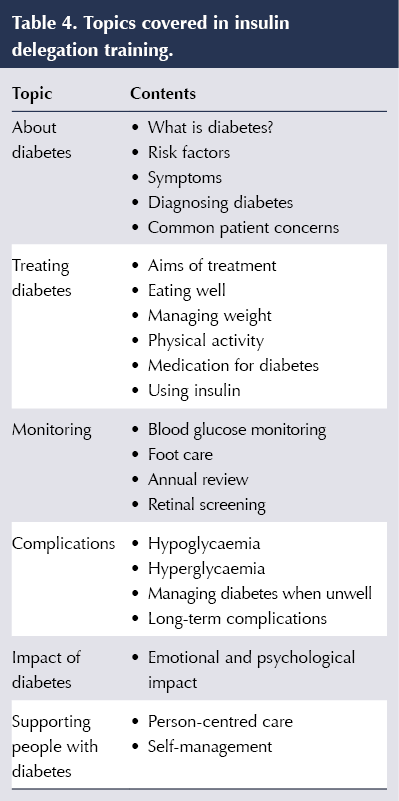
Ninety staff from the fourteen care homes and one respite facility completed the necessary online training prior to their face-to-face assessment of competency. Table 4 lists the topics that were covered by the training. A resource pack was also supplied to carers to use for future reference.
Competency had to be checked at least once per resident and typically three times for a new carer/ resident every 2 years. Assessment in practice had to be by a Registered Nurse who could demonstrate competence at level 4 or above, as per Fearon (1998).
These HCWs who have been trained and assessed are still using these skills.
Results
The pilot has been successful in achieving the following benefits.
1. Cost and time saving for District Nursing
In the monitoring of capillary blood glucose and insulin administration, the District Nursing team spends an average 30 minutes per visit. Twenty-two people with diabetes in the pilot started to receive this care from the HCWs in their respective homes. For 46 visits a day requiring 30 minutes each, this equates to 1380 minutes (23 hours) per day, 365 days per year: a total of 8395 hours a year. When accounting for the 30 minutes required for the Registered Nurses to assess the competencies of the HCWs three times per patient before being signed off (2970 hours a year), this pilot resulted in 5425 hours saved from the District Nursing caseload per year. These hours could be diverted to look after more vulnerable people in the community requiring healthcare support, especially on the background of the COVID-19 pandemic.
The Band 5 mid point is £27 239 per annum. Their gross hourly income before tax is £13.93. Calculating the cost of the visits (5425 hours) per year at this hourly rate, the pilot demonstrated a saving of £75 570. Furthermore, these savings do not include the mileage cost.
2. Cross-sector working
The pilot was designed in close collaboration with the District Nursing team, the Health and Social Care representative, the diabetes specialist team and MOCH. This has been incredibly positive in terms of ensuring that the care provision for these cohorts of patients has undergone multisectoral discussion and agreement. This process has helped in identifying how this intervention can be improved to reflect the learnings derived from the pilot.
3. Benefit to residents and patient-focused care
Delays in the delivery of insulin have been identified in numerous incident reports. Various factors have been identified, including task allocation, heavy caseloads, traffic, etc. HCWs who have received training and been assessed to be competent can provide this care without these extraneous delays. The HCWs also have a closer professional relationship with the residents, whom they have regular interactions with. Their presence within the care environment where the intervention takes place also reduces, if not avoids, issues relating to the incidence of acute diabetes complications (i.e. hypoglycaemia and hyperglycaemia).
Examples of staff and patient feedback
One District Nurse describes the benefits and challenges of the pilot:
“Insulin delegation has been an incredibly positive experience. Although it was quite stressful at the beginning as I was concerned that errors might happen, this has not been the case. I do still provide a resource pack. I feel that the care homes do need information that they can refer to when they are unsure or need reminding about procedures and hypos, etc. A difficulty that I had to overcome was calibrating the glucose monitors; this took some time for them to get on board with, but we managed to get there in the end with showing them how to order calibration solution”.
Feedback from four care home managers has also been positive:
“The whole process of moving the administration of insulin task from community nursing to the healthcare team has given us a much better awareness of diabetes and an opportunity to discuss our learning gaps with an expert. It took a couple of weeks to competency-check all the senior HCWs, which was plenty of time to gain confidence and provide mutual support to each other.”
“It was quite daunting to start with, but the bonus of administering insulin at a time the resident wants it is huge, and reducing the footfall into the home has been a necessity in the last 15 months.”
“Our head office governance can be a block to us doing this. We were really keen to support our residents and local health team and have now been able to positively shift the company. Having a guide that we can add as an addendum to the Medicines policy is useful.”
“If we have any queries the [Advanced Nurse Practitioner] who takes our weekly ward round can resolve them – it helps when everyone knows what the process is and how the network across services works.”
Care home residents appeared happy with the changes:
“I’m partially sighted and was unable to dial up the insulin accurately – having the carers that I am familiar with has been great, and my diabetes and sugar levels are now much better controlled. If they didn’t do it I may have had to move to a different care facility that provided nursing care.”
“I’m more comfortable with the care home regular carers giving me my insulin, they know me well and it’s part of the morning routine now.”
“I’m not bothered who gives me my insulin – as long as it gets done.”
One resident’s next of kin was also happy with the pilot:
“On admission to the care home we signed to agree that medicines administration is done by the care staff. It was a comfort to be told explicitly that the insulin administration required additional training and that the regular community nursing team would do that. Dad was familiar with them so it was a really good handover”.
Conclusions
This pilot has resulted in a significant reduction in the number of visits on the District Nursing caseload. It has also enhanced cross-sector working and reduced delays in the timing of insulin administration and improved access for patients in the delivery of this crucial intervention.
As a result of the pilot, we have been able to develop a full guideline which is fit for local use and adheres to the best practices described by NHSE. Owing to our experience in this area, we have been able to adjust the voluntary framework to ensure it is practically fit for purpose locally. The success of our pilot enabled buy-in for key stakeholders and much-needed reassurance in terms of risk management, enabling us to quickly take up the NHSE voluntary framework and obtain governance and accountability sign-off through our local Trust.
Through working closely with our key stakeholders from the outset of this pilot, we were able to overcome challenges that others have struggled with, mainly around governance processes, that have prevented several neighbouring areas from getting this work off the ground. We learned early on that it was vital to engage the Head of Community Nursing employed by East Sussex Healthcare, the organisation that supplies Community Nurses. Without this buy-in, the spread and subsequent roll-out of the pilot would not have been possible.
Owing to our successful pilot, our work is now being considered at a Sussex level.
Recommendations
The pilot has revealed elements within the process that needed improvement. Understanding these proved especially useful when the local guidance on insulin delegation was drafted.
• In compliance with the NHSE and NHSI framework, a review of each patient’s glycaemic management and control should be done every six months by a diabetes nurse specialist, GP or suitably competent healthcare professional, such as a nurse or pharmacist acting within scope of practice, and annually by the MOCH service as part of the structured medication review.
• Requirements for HCWs before they start the delegation process should include up to basic life support and anaphylaxis training. They would also be expected to co-operate with and participate in ongoing clinical and management supervision and assessment by a registered nurse/registered practitioner, including observed practice.
• The online training package has been changed to the e-LfH Delegated Administration of Insulin programme, to align with the national recommendation in the NHSE/NHSI framework. E-learning verification should be confirmed by the HCW’s line manager at annual appraisal.
• A fully completed risk assessment for each person with diabetes receiving care is essential to meet legal requirements. The registered nurse/practitioner who is delegating the duty must complete this risk assessment for each person with diabetes, and a copy kept in the patient’s care record.
- Insulin must not be administered without the completion of a risk assessment, an individualised care plan/support plan and evidence that the delegated HCW has been assessed as competent to undertake the delegated task.
- The registered nurse/practitioner must complete a comprehensive record of care and identify the condition of the person with diabetes as predictable.
• There must be clear arrangements for timely access to the registered nurse/practitioner for advice and guidance if/when the patient’s condition and blood glucose ranges deviate from what is normal for them. Access may be via phone or other telehealth methods.
• The registered nurse/practitioner must obtain informed consent to the delegation of the task from the person with diabetes. If that person does not have the capacity to give consent, the principles of the Mental Capacity Act (2005) should be followed as set out in the Consent to Treatment Policy (2015) and Mental Capacity Act (2005).
- The registered nurse/practitioner must ensure that the person’s mental capacity is kept under review. The HCW is responsible for the duty to obtain ongoing consent every time medicines (in this case insulin) are administered.
• NHS England has also produced a competency framework and workbook, Blood glucose monitoring and subcutaneous insulin administration, for use with HCWs.
• Competence should be reviewed on a six-monthly basis, or in response to any incidents occurring and/or being reported. If there has been break in practice, a refreshed certificate of e-Learning and updated competency assessment is required before the delegation of duties to the HCW can recommence.
- Where the HCW has already completed initial training and demonstrated competence in practice, assessment of competence does not need to be repeated for each new person receiving care. However, the delegating registered nurse/practitioner does need to complete a risk assessment for each new person receiving care and each HCW taking on new responsibilities.
- A signed confirmation of competence assessment by the registered nurse/practitioner must be obtained for each HCW as assurance that the training and assessment of competence was successfully completed.
- The competency assessment should be completed five times as part of the initial training and then once at six-monthly intervals by the registered nurse/practitioner.
• Registers must be maintained to record the following:
- A register of registered nurses and registered practitioners willing and able to delegate administration, held by Community Nursing.
- -A register of HCWs deemed competent, held by District Nursing.
- Records of e-Learning completion, competency assessment, completion of checklist and final sign-off, held in the care homes’ training records.
- -Annual review of registers undertaken by care homes through self-declaration and audited through random selection by the care home and Community Nursing.
• The HCW should have access to advice and guidance on a regular basis (e.g. monthly clinical supervision and regular huddles to discuss diabetes cases) as part of a mentoring relationship, and the ability to access ad hoc advice when needed.
Resources
- Diabetes UK: Diabetes in Healthcare introductory diabetes education tool
- Diabetes UK: Position Statement: Delegating responsibility for insulin administration to non-registered practitioners
- e-LfH: Delegated Administration of Insulin training module
- NHS England: Competency framework and workbook: Blood glucose monitoring and subcutaneous insulin administration
- NHS England: Checklist for health and care workers who are delegated responsibility to administer insulin to adults
- Primary Care Diabetes Society: Six Steps to Insulin Safety CPD module





Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024