Nationally there is an urgent need for new approaches to education for healthcare professionals caring for inpatients with diabetes. Locally, we identified that clinical commitments represent a major barrier to staff education. Training that does not draw staff away from their workplaces and routine duties is, therefore, desirable. One potential strategy for addressing this educational need could be delivering outreach training in clinical environments and specifically adapting content to meet the needs of each group.
Improving the quality of inpatient care
We performed a quality improvement project based on an educational tool developed by Ruth Miller (see Figure 1) to improve the care that people with diabetes were receiving (Curtis and Miller, 2017). The tool consists of 10 points based on the most common insulin- and diabetes-related errors, as identified by National Diabetes Inpatient Audit data (https://bit.ly/2xwFd0S), the 2010 National Patient Safety Agency rapid-response reports and local experience. We aimed to deliver highly flexible content in bite-size chunks to all healthcare professionals outside of our specialist ward and department who care for inpatients who may have diabetes. Our training was designed to maximise convenience by fitting in around clinical duties, and to be pertinent to the specific needs of each group.
Training was advertised with the support of the Medical Director and Director of Nursing. Two diabetes specialist nurses carried out ward drop-ins 7 days per week and approached all healthcare professionals present (doctors, nurses, nursing assistants, pharmacists, midwives, therapists, operating department practitioners and theatre technicians), inviting them to take part in a short training session in diabetes. Group sizes were typically between one and five participants. Some areas (endoscopy, emergency department and intensive care unit) required sessions to be booked in advance due to their working patterns and job requirements.
Adapting content
Content was based on the 10-point training tool; however, this was customised to the specialty of the participants present. For example, on surgical wards there were many questions about the use of intravenous insulin and glycaemic control during nasogastric feeding. The oncology wards commonly focused on high-dose steroid use and how to best manage symptoms of hyperglycaemia in the patient who is already unwell. On elderly care; ear, nose and throat; and stroke wards, the conversations and questions were often around hyperglycaemia due to enteral feeding. Our gastroenterology colleagues regularly sought training on the specific requirements of secondary diabetes.
Results
A total of 640 healthcare professionals were trained in a 6-month period. Training efficacy was assessed by participant self-reported confidence in 11 different domains on a three-point Likert scale immediately prior to education and 3 months after training. Significant improvement in staff confidence was seen across all areas post-training (P<0.001). The results of the National Inpatient Diabetes Audit before and after this quality improvement strategy were compared. Our Trust moved from the highest quartile for insulin errors to the lowest quartile in this short time-frame. We have found that working collaboratively with colleagues in the clinical setting has engendered a mutual ownership of maintaining high standards of diabetes care, as opposed to the expectation of deferring to the specialist team.
Rolling out training
This educational tool has been presented to the All-Party Parliamentary Group for Diabetes as an example of how to improve inpatient outcomes and has been up taken by other Trusts, such as the Royal Free NHS Trust. Details of diabetes 10-point training can be found on the Diabetes UK website: https://bit.ly/2NkmCcg). The training is a generalisable and easily reproducible strategy that can deliver rapid results, benefiting both staff and inpatients with diabetes.
Expansion of the training programme
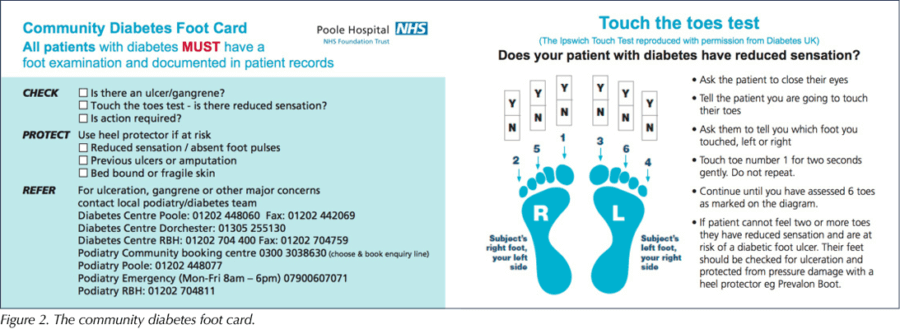
The tool has also been used in other healthcare arenas. An adapted version has been trialled in community settings. A community diabetes foot card (Figure 2) was also produced, including the Ipswich Touch Test, to prompt nurses to check, protect and – where necessary – refer patients and to document foot examination.
Ruth now works as Diabetes Nurse Consultant in the North West London Diabetes Transformation Programme. In the last year, she has developed a further five diabetes 10-point training programmes for staff working in settings where there is a high prevalence of diabetes and a lack of access to specialist advice or training. These programmes are in the process of being implemented across eight Clinical Commissioning Groups in north west London in the following settings: haemodialysis centres, community nursing teams, homeless hostels, care homes and mental health workers. The ambition is to improve basic diabetes care at scale.
The diabetes 10-point training for hospitals is in the process of being implemented in acute Trusts across north west London.
For more information or if you want to implement the 10-point training tools in your setting, contact Ruth Miller at: [email protected]





In her final editorial, Su Down reflects on her career and the remarkable progress in diabetes care she has seen.
11 Dec 2025