Foot and ankle complications in diabetes, including ulceration, amputation and Charcot neuro-osteoarthropathy (CNO), present a significant socioeconomic burden that negatively affects an individual’s physical and psychological wellbeing, and the lives of their friends and families (Coffey et al, 2019, Gooday et al, 2022).
CNO is a destructive, inflammatory condition of the bones, joints and soft tissues of individuals with peripheral polyneuropathy. Although CNO can occur in anyone with peripheral neuropathy, it most commonly affects the foot and ankle of individuals with diabetes mellitus (International Working Group on the Diabetic Foot [IWGDF], 2023). In these cases, progressive and uncontrolled inflammation causes osteolysis, leading to the weakening of the foot’s structure, which can result in fractures, joint dislocations, severe lower limb deformities, ulceration and even amputation (Gooday et al, 2021).
For individuals with diabetes mellitus, the true incidence of CNO remains unknown, but reported prevalence ranges from as low as 0.04% in specialist foot care centres in England to 0.79% in Swedish national diabetes registries (Metcalf et al, 2018, Tsatsaris et al, 2023). With an estimated average prevalence of 0.3%, approximately 1.9 million people with diabetes worldwide are expected to develop CNO by 2030, increasing to 2.3 million by 2045 (International Diabetes Federation [IDF], 2021).
CNO is commonly associated with midfoot collapse and the distinctive ‘rocker-bottom’ deformity, but it can also affect other joints with varying life-limiting presentations. Despite being associated with sensory neuropathy, pain or discomfort may still be present during the early acute stage, however, is usually significantly reduced compared to individuals with intact sensation experiencing a similar injury (Rogers et al, 2011).
While it often presents with intact skin, the structural and functional changes in the limb can lead to the coexistence of active, infected foot ulcers. Studies have shown that individuals with foot ulcers resulting from CNO-related deformities have a 6 to 12 times higher risk of major amputation compared to those with ulcers unrelated to CNO (Sohn et al, 2010; Wukich et al, 2017).
The treatment goal is therefore to resolve the inflammatory process as soon as possible, alleviate pain and preserve foot architecture without advancement to ulceration. This is achieved by promptly initiating a knee-high offloading device, preferably a non-removable below-knee cast or walker boot (IWGDF 2023). The duration of offloading can vary significantly, with national and international studies reporting a median time to remission of between 3–12 months (Game et al, 2012; Chantelau et al, 2007), although frequent cases extending beyond 1–2 years have also been documented. Individuals who adhere to self-care practices such as consistent use of offloading devices have been reported to have significantly better outcomes (Binning et al, 2019).
According to Sabate (2013), adherence is the extent to which a person’s behaviour corresponds with agreed recommendations from a healthcare provider. In their systematic scoping review, Racaru et al (2022) identified various complex and multifactorial factors that can negatively affect adherence to foot offloading, and therefore poorer outcomes. These included biological factors, such as disrupted gait and postural instability, as well as psychosocial factors like stigma and lack of motivation.
Additionally, a qualitative study by Gooday et al (2022) exploring individuals’ experiences of living with Charcot neuroarthropathy (CNO) highlighted impactful themes which extend beyond the burden of wearing an offloading device. These themes included feelings of frustration and social isolation, disruption or loss of roles and responsibilities, strain on relationships, additional pain caused by the offloading devices, and self-directed or externally perceived blame for developing CNO. The study emphasised that mitigating the negative consequences of CNO requires a deeper understanding of the physical and psychosocial experiences of individuals with diabetes and CNO.
Increasing knowledge through patient education remains a cornerstone of practice despite strong evidence showing it has a minimal effect on diabetes foot ulcer rates (Dorrestejin et al, 2014; Bus et al, 2016). This insight could assist healthcare professionals in developing interventions that extend beyond traditional patient education. Incorporating approaches such as motivational interviewing to enhance knowledge and foster motivation for behaviour change (Keukenkamp, 2018), alongside extrinsic prompts, such as digital watches, phone apps, activity diaries and infrared thermography, to support daily monitoring and understanding of the extent of a condition where lack of sensation limits understanding (Binning et al, 2019).
Infrared thermography
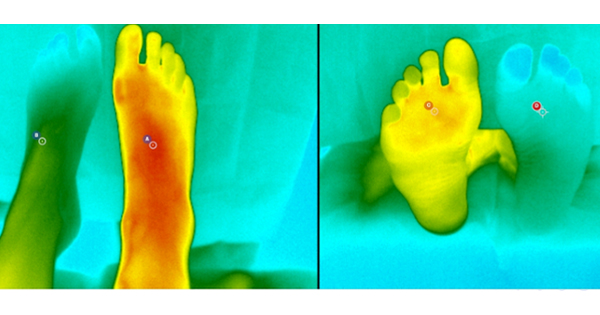
Infrared thermography is a safe, non-invasive imaging technique used to measure skin temperature and plays a valuable role in the prevention, early detection, and monitoring of inflammatory complications in diabetic foot disease — including pressure related injury, infection, vascular compromise and Charcot neuroarthropathy (IWGDF, 2023). The technique works by detecting infrared radiation naturally emitted by the body and is commonly applied in clinical practice using two main methods. The first involves handheld digital thermometers, which provide quantifiable readings on a digital display [Figure 1]. The second method uses infrared-enabled tablets that capture thermal images — visual maps of temperature distribution across the skin using a graded colour scale (Harkin, 2023) [Figure 2]. This latter method, known as thermal imaging, offers a more detailed overview of the surface temperature variation and supports targeted assessment of the areas of concern.
Accurate site selection with handheld thermometers can be challenging, especially during the consolidating phase of CNO, when ‘hot spots’ are not always visibly apparent. To address this, the IWGDF recommends a standardised approach to temperature measurement to ensure consistent and reliable comparisons over time (IWGDF, 2023). In contrast, thermal imaging, offers a visual map of temperature distribution, allowing both clinicians and patients to easily identify areas of concern. Specific regions can then be precisely selected for targeted measurement and longitudinal comparison.
The following case studies demonstrate how the use of thermal imaging can serve as an effective clinical tool to educate and motivate patients towards positive behaviours — such as consistent use of offloading devices and activity modification. By visually revealing underlying inflammation or trauma, this approach enhances patient understanding and supports adherence to preventative strategies, ultimately contributing to improved clinical outcomes.
Case study 1
A 70-year-old female with a 6-year history of type 2 diabetes, hypertension, hypercholesterolaemia, background retinopathy and peripheral neuropathy was referred to the acute multi-disciplinary diabetes foot clinic (MDFC) for assessment of an acute CNO. Prior to her first visit, plain X-Rays and magnetic resonance imaging (MRI) had already been performed. The X-Ray was unremarkable; however, the MRI revealed patchy marrow oedema involving the second to fourth tarsometatarsal joints, with minor involvement of the sustentaculum tali. The appearances were suggestive of early midfoot CNO with minor changes to the sustentaculum tali — consistent Stage 0 active CNO as defined by the IWGDF in 2023 (IWGDF, 2013).
At presentation, the patient reported an 8-week history of right foot swelling with a pain during mobilisation, which began after helping a neighbour paint their house. She expressed frustration at the injury, as it significantly limited her ability to walk or exercise — an activity she relied on to support weight management and improve glycaemic control. Her HbA1c had recently improved, 99 mmol/mol to 66 mmol/mol over a 4-month period. She had no previous history of lower-limb ulceration or neuro-osteoarthropathy.
Clinical examination revealed palpable, bi-phasic pedal pulses and evidence of peripheral neuropathy. The right foot appeared more oedematous and erythematous, extending from the forefoot to the ankle, although the overall structure and arch profile remained intact. Using a standard hand-held digital thermometer [Figure 1], the temperature of the right midfoot was 10c higher dorsally and 11c plantarly compared to the same location on the contralateral foot.
Treatment and intervention
A diagnosis of CNO was confirmed, and the patient was provided with a removable offloading walker boot, with plans to fit a custom insole the following week. Although she had been informed prior to the appointment that the diagnosis of CNO was likely, she appeared emotionally unprepared to accept it. She expressed disbelief — not only about the diagnosis but also about her diabetes itself — insisting her foot discomfort was merely a sprain and that her foot sensation was normal, despite clear clinical evidence of peripheral neuropathy. However she acknowledged the presence of inflammation and pain and agreed to wear the boot consistently when mobilising. A follow-up review was scheduled 7 days later.
At the follow-up appointment in MDFC, the patient reported adherence to wearing the boot but remained sceptical about its necessity. To support consultation infrared thermal imaging was introduced [Figure 2], enabling both visual and quantitative comparison of foot temperatures [Figure 3]. The thermal image clearly illustrated the extent and distribution of inflammation, offering a compelling visual representation pf the pathology. The asymmetry in temperature — both in numeric values and striking colour contrasts — had a significant impact on the patient. This visual evidence shifted the focus of the conversation from questioning the need for offloading to seeking clarity on treatment duration. This change in perspective opened space for a more meaningful patient-led discussion about her diagnosis and the implications of her diabetes management.
As part of her ongoing management, a custom total contact insole was fitted to the walker boot, with an ‘even-up’ shoe balancer to the contralateral limb to address leg length discrepancy and improve gait stability during offloading.
The patient was reviewed fortnightly in the joint podiatry-orthotics clinic over a 16-week period [Figure 4]. At each visit a progressive reduction in temperature differences and inflammatory signs was observed. By the end of this period, inter-limb temperature differences had fallen below 2c on two consecutive visits, using the thermal camera and all clinical signs of inflammation had resolved. The Charcot episode was deemed consolidated with no residual structural deformity or requirement for further imaging. She was subsequently discharged from specialist care with custom total contact insoles for use in her own trainers and referred to community podiatry foot protection services for continued preventative care and monitoring.
Case study 2
A 56-year-old male with a 14-year history of type 2 diabetes (HbA1c of 82mmol/mol, up from 65mmol/mol), hypercholesterolaemia, background retinopathy, a BMI of 34.8Kg/m2, established peripheral neuropathy, and a prior history of neuropathic foot ulceration was referred to the acute multidisciplinary diabetes foot clinic (MDFC) by the community podiatry foot protection team. The referral was prompted by multiple episodes of ankle inversion, which the patient associated with recently issued orthopaedic footwear and insoles. These episodes resulted in the development of a hot swollen left foot with a noticeable altered arch profile [Figure 5].
The patient reported a deep, throbbing pain in his left foot, accompanied by redness and swelling. He was concerned about the visible change in foot shape and expressed frustration, attributing the issue to the recently issued hospital footwear. On examination, peripheral neuropathy was confirmed, and pedal pulses were palpable and bi-phasic bilaterally. The left foot and lower leg showed increased oedema, and medial convexity deformity was noted, consistent with arch collapse. Using a standard handheld digital thermometer [Figure 1], his left midfoot was 9.5c warmer dorsally and 11c warmer plantarly than the corresponding sites on the right foot — findings indicative of active CNO.
Differential considerations included ankle fracture, posterior tibial rupture, deep venous thrombosis. A plain X-Ray was performed and appeared normal despite clinical deformity [Figure 6]. However, weightbearing views were not obtained which may have demonstrated alignment abnormalities. Ideally, bilateral plain X-rays with anteroposterior (AP), medial oblique, and lateral projections should be taken for accurate comparison (IWGDF, 2023). Due to strong clinical suspicion of CNO, an MRI was arranged.
Treatment and intervention
At initial presentation, immediate offloading of the affected limb was advised pending diagnostic confirmation. Removable and non-removable options were discussed, and the patient opted for a removable boot. He was fitted with the boot at the first visit, and a custom total contact insole was supplied and fitted the following week.
MRI findings confirmed active Charcot neuro-osteoarthropathy involving the ankle, hindfoot and midfoot, with a pes plano-valgus deformity, subluxation at the medial navicular, cuneiform joint, plantarflexion of the navicular, and a concurrent insufficiency fracture at the base of the second metatarsal [Figure 7]. According to the IWGDF (2023), the findings were consistent to Stage 1 active CNO.
During each clinical visit, the patient expressed frustration regarding the change in shape of his foot and the requirement to wear an offloading device, which he found cumbersome and awkward to walk with. He remained sceptical about the benefit of the custom insole, particularly as he believed his previously issued footwear and insoles had contributed to the development of his condition.
In the early phase of management, foot temperatures were monitored using handheld digital thermometer [Figure 1]. This provided objective measure of inflammation and served as a useful tool to communicate the ongoing activity of CNO to the patient. At that stage, the information supported clinical rationale for continued offloading and improve adherence to the prescribed boot.
However, a notable shift in patient engagement occurred at week 8, following the introduction of thermal imaging to monitor inflammation. Upon viewing the thermal images for the first time [Figure 8], the patient expressed surprise at being able to see the inflammation — particularly as he had no sensory perception of it. He remarked that, although he understood the importance of the boot, visualising the inflammation brought a new level of awareness and reinforced his motivation to adhere to treatment. Reviewing the thermal images and temperature readings each week also facilitated open discussions about the patients understanding of his condition and empowered him to explore lifestyle changes that could help reduce his risk of future diabetes-related and limb complications. This was further reinforced through fortnightly reviews, during which serial images showed a gradual reduction in temperature and visible improvement in the pathology [Figure 9] — providing the patient with clear visual evidence of progress and strengthening his commitment to the treatment plan.
By 6 months, temperature differences between both limbs were within 2c across 3 consecutive visits, with all other clinical signs of active disease resolved. His foot was deemed consolidated [Figure 10] and no further radiological investigations were required. Despite earlier concerns that similar footwear had contributed to his condition, he now understood their critical role in maintaining foot structure and function.
A brief questionnaire [Table 1] revealed highly positive patient-reported experiences, with both participants expressing confidence with the tool and recommending its broader use. Free text comments reflected perceived clarity and empowerment in understanding their condition.
Discussion
The Thermidas IRT-384 thermal tablet [Figure 2] is a portable thermal imaging tablet designed for routine clinical use. It holds Class IIa CE certification as a medical device and is approved by the MHRA for use in the UK. This certification is more desirable to other models without approval as shows the device is validated, regulated and specifically designed for medical diagnostics. While lower-cost or industrial thermal cameras may look similar, they lack the clinical validation, legal assurance and safety standards required for use with patients, especially in high-risk scenarios like diabetes-related foot care.
The case series demonstrates the value of thermal imaging as a tool not only for clinical assessment but also for enhancing patient engagement in the management of CNO. In both cases presented, thermal imaging provided immediate, visual evidence of inflammation across both feet simultaneously that was not subjectively perceived by the patients due to peripheral neuropathy. The visibility of the thermal images facilitated more meaningful conversations around severity of the condition, underscoring the rationale for strict adherence to offloading regimens and the importance of glycaemic control. The thermal tablet was easy for the clinicians to use, employing a simple point and shoot method that could be seen on the tablet screen during use for the best shot and required only basic operational instructions and guidance for initial image interpretation.
Patients responded positively to visual feedback, both reporting increased understanding of their condition and greater motivation to comply with treatment recommendations. This behavioural shift was associated with accelerated clinical improvements, including earlier than expected signs of resolution, reduced need for additional radiological imaging to confirm consolidation and avoidance of more severe structural foot changes. These outcomes suggest that thermal imaging may serve as a valuable adjunct in managing CNO, paricularly when used to support patient support and engagement.
Conclusion
Charcot neuro-osteoarthropathy is a serious, life-altering condition that can significantly compromise an individual’s quality of life and independence. This case series presents multiple examples where the use of digital thermal proved beneficial in clinical practice — not only as a diagnostic adjunct but also as a powerful connection tool. By visually illustrating areas of inflammation, thermal imaging helped bridge the gap in patient understanding caused by peripheral neuropathy, which often masks symptoms. Furthermore, sharing these visual findings with patients created a valuable opportunity for open person-centred dialogue. This facilitated meaningful discussions about their condition and individual circumstances ultimately supporting the development of tailored management plans and motivating adherence to pressure-relieving strategies and improved glycaemic control.