Statistics show 15% of high-risk patients with diabetes will experience a diabetic foot ulcer (DFU), of which 1.8% will have an amputation, with a 68–79% mortality rate within 5 years. The NHS expenditure for ulcer management in 2014-15 was £837–£962 million (Ahmed et al, 2010; Kerr et al, 2019; Altoijry et al, 2021). National Institute for Health and Care Excellence (NICE) guidelines NG19 suggest addressing this issue from the earliest point in treatment, where multidisciplinary teams should use specialised healthcare techniques to manage such wounds (NICE, 2015).
The first metatarsophalangeal joint (MTPJ) is one of the most common sites for DFUs (Ahmed et al, 2010). A cascade of issues leads to inflammation that is only visible after 3–10 days, when initial tissue damage has already occurred; but Collet et al (2019) report that measuring oxygen saturation levels (SpO2) during this period can help prevent tissue breakdown. Using the moorVMS-OXY™ tissue oxygenation system (Moor Instruments, Delaware, USA) allows detection of optimal levels of SpO2, so that effective treatment and wound healing can be managed (Ito et al, 2016; Malone-Povolny et al, 2019).
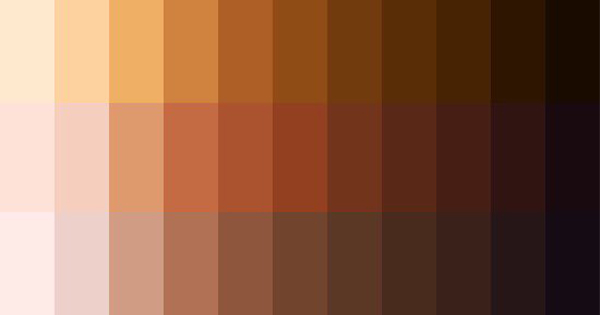
Based on white light reflectance spectroscopy, the moorVMS-OXY is non-invasive, pain-free and easy to use. Probe-to-skin contact scatters white light into tissue at 500–600nm, being absorbed by two major chromospheres: oxygen and melanin. Residing in superficial layers of the skin, melanin acts as a confounding variable and there is a significant difference of melanin concentrations between dorsum and plantar (Zonios et al, 2001). Technologies such as pulse oximetry usually overestimate SpO2 values for dark skin (Shih et al, 2015; Bothma et al, 1996). This study aims to investigate the effect of anatomical sites and melanin, using the Fitzpatrick skin phototypes (1975) scale classification system on SpO2 readings in healthy individuals.
Method
This research is ethically approved by University of Brighton, The School of Health Sciences Research Ethics Panel. Volunteer participants from Fitzpatrick skin types 1–6 were recruited through the university. Written and verbal informed consent were taken. Screening for inclusion and exclusion criteria, a Dopplex MD2 Bi-Directional Doppler was used to test the vascular status of participants. The moorVMS-OXY was used for measuring SpO2; to obtain data, an OP1T probe was used along with a flexible PVC probe holder PH1-V2.
Participants were divided into three groups by Fitzpatrick skin type (FST): group 1, FST 1–2; group 2, FST 3–4; and group 3, FST 5–6. The other independent variable was site, which was also broken into two: site 1 (dorsal) and site 2 (plantar).
Results
Values for SpO2 obtained from all 19 participants were in the normal range for the foot, suggesting that appropriate inclusion/exclusion criteria were followed, reducing bias and the chance of error (Qi et al, 2022) The mean difference for SpO2 values between each site was significantly different 0.000001 (p value<0.05), excluding the effect of skin type. In Table 2, the confidence interval lacked difference, showing less probability of error as outlier values would be reduced, indicating values obtained were reliable and valid for site.
This study identified that there was no statistically significant difference for the FST of 19 participants (Table 4), resulting in acceptance of the null hypothesis of no difference in variables. This study showed that the amount of pigmentation nor FST created an impact on the SpO2, and increased concentration of melanin did not act as a confounding variable. Although the p value was not significant, the level of error in each skin type group could suggest that melanin did impact SpO2 values as there is a positive correlation seen in Table 4, as the skin pigmentation increases and the difference in confidence interval increases too; thus, suggesting melanin caused greater error in the results. Which are what previous studies showed, but this was not significant enough to accept the alternative hypothesis (Mujis, 2004; Qi et al, 2022).
The results of considering the impact of both independent variables on SpO2 values are in Table 5.
The combination in site 1 (dorsum) of groups 2 and 3 showed a significance of 0.047 (p value <0.05), suggesting that the SpO2 on the dorsum in FST 5–6 was statistically significant compared to FST 3–4.
Discussion
The findings of this study indicate that there was a significant difference in the mean obtained in the SpO2 values when comparing the dorsum and plantar surface of the foot p=0.000001 (p value <0.05) excluding the effect of FST (Table 3). When considering factors that may contribute to these results, anatomy and tissue pigmentation need to be considered (Boyle et al, 2019).
Anatomy is a major factor impacting SpO2, the dorsal skin of the foot varies in some significant respects when compared to the plantar skin. For example, strength of tissue, thickness, pigmentation and angiosomes differ in the two regions (Kumar and Schmitt, 1997). Youngs modulus can help in understanding the skins strength and its likelihood of ulceration (Sasaki and Odajima, 1996). When considering the mechanical stresses applied to the dorsum versus the plantar surface of the foot, it is easy to appreciate that the physical stresses and strains placed on the plantar structures of the foot are considerably different to those placed on the dorsum. The plantar surface can bear 100kPa pressure through the calcaneus, hence prevents skin tearing, blistering and ulcers. Thus, if the skin on the plantar foot develops an ulcer it would require more nutritional support hence the increased vascular network. It is reported that there is a 2.9-fold greater vessel density in the plantar surface of the foot as it is perfused by three different of angiosomes, whereas the dorsum is supplied by only one (Ricci, 2015; Lechner et al, 2019). This could be a factor in the significant difference of SpO2 value 0.000001(p value <0.05) in Table 3 for site variable. This increased perfusion is further supported by the mean SpO2 for the dorsum being 33% and the plantar surface 56% (Boyle et al, 2015; Altoijry et al, 2021; Shabhay et al, 2021).
As well as considering the anatomical construct of the tissues, melanin content needs to be explored. There is considerably less melanin present in the plantar compared to the dorsum of the same foot (Nagaoka et al, 2007). This pigmentation difference could be one of the factors which has contributed to the significant difference in SpO2 values obtained in this study. The moorVMS-OXY is recommended for use on FST 1–2, due to the potential interference of melanin (Qi et al, 2022). This is supported by Shaban (2013), who suggested that melanin made it difficult to distinguish between reflectance getting an equal number in the three skin type groups.
When exploring the lower and upper bound of the confidence interval of group 3, it shows that the greatest difference occurs when comparing to group 1 and 2. An explanation for that can be that although all groups had equal number of subjects there were two anomaly values that could affect the mean greatly. In Table 2, we can see there were no participants of FST 1 and one participant with FST 6. These values fall far from mean number of participants in each group and when added to the mean SPO2 values it could greatly affect data input. The results found are closely comparable to Mahmoud et al (2010) and Zonios, Bykowski and Kollias (2001), whose studies have similar participant quantities and found that skin pigmentation did not affect SpO2 values. These findings are contradictory to studies such as Finer et al (2007) and Yudovsky and Pilon (2010), who found that skin pigmentation did affect SpO2 values, and their sample size was over 100, suggesting that the chances of type 2 errors occurring in studies with fewer participants is greater.
Limitations
Previous studies suggest that age and gender both could affect SpO2 values in our study. Having a controlled age range and gender ratio may reduce bias by increasing the replicability of the study and result reliability. Sample size affects most studies. As a pilot study, this research was efficient at highlighting the study’s biggest limitation. Machine probes such as the adhesive probes that come with the moorVMS-OXY may cause greater bias in SpO2 readings due to factors such as sweat causing detachment of the probe from the skin. Finally, the Fitzpatrick scale may not be entirely suitable for clinical purposes due to its subjective nature.
Conclusion
There is a statistical significance in SpO2 when comparing the dorsum and plantar values of the first MTPJ across the population group studied; however, there was insufficient data to conclusively say that any FST affected the SpO2 values. If greater scale studies are conducted, results may become more consistent with previous findings. Assessing the SpO2 values in hypopigmented areas of differing skin types is worthy of further investigation.