Chronic, non-healing lower extremity wounds have been estimated to affect up to 4.5 million people total in the United States (Frykberg and Banks, 2015). These wounds can last for over a year and recur in 60%-70% of patients (Frykberg and Banks, 2015). These wounds are often associated with diabetes, arterial disease, or neuropathy (Frykberg and Banks, 2015). For patients with diabetes, the presence of these non-healing wounds carries a risk for amputation (Lin et al, 2020; Crocker et al, 2021). The risk for amputation is further increased in patients that are of the male sex, and with a history of tobacco use, foot ulcers, osteomyelitis, gangrene, lower body mass index, and higher white blood cell count (Lin et al, 2020).
With the large number of available wound care modalities (such as surgical debridement, advanced wound dressings, and negative pressure wound therapy [NPWT]), clinicians have a wide range of options for managing chronic, lower extremity ulcers which may potentially help avoid limb amputation. One advanced wound care option for the management of lower extremity ulcers is NPWT with instillation and dwell time (NPWTi-d, 3M™ Veraflo™ Therapy, 3M Health Care, St. Paul, MN) using reticulated open cell foam dressings with through holes (ROCF-CC, 3M™ Veraflo Cleanse Choice™ Dressing, 3M Health Care). NPWTi-d with ROCF-CC dressings provide hydromechanical removal of infectious materials, non-viable tissue, and wound debris which reduces the number of surgical debridements required, while promoting granulation tissue formation and creating an environment that promotes wound healing. The use of NPWTi-d with ROCF-CC dressings was assessed in three patients, two with diabetic foot wounds, and one with a non-healing, lower extremity wound.
Methods
Patients presented for care after failing previous treatment plans with other health care providers. Their wounds were assessed for osteomyelitis and malignancy, using both wound biopsy and magnetic resonance imaging (MRI). Antibiotic therapy was initiated for all patients. Surgical debridement was performed followed by application of NPWTi-d with ROCF-CC dressings. Normal saline was instilled into the wound bed with a 1-minute dwell time, followed by continuous negative pressure at -125 mmHg for 2.5 hours. Dressings were changed every 2-3 days. Once the wound bed was covered with healthy granulation tissue, NPWTi-d was discontinued. Patients then either received split-thickness skin grafts (STSG) or continued wound care using advanced wound dressings alone or with hyperbaric oxygen therapy (HBOT).
Case study 1
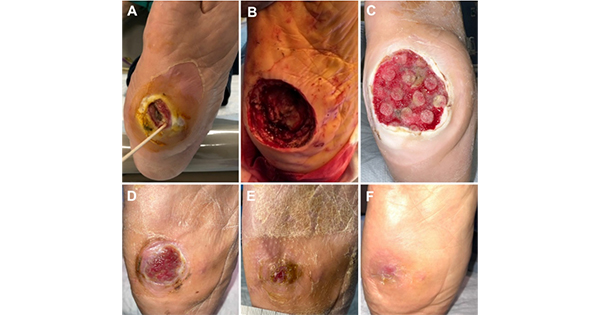
A 66-year-old female presented with a Wagner Stage 3 diabetic foot ulcer (3.9 x 4.0 x 3.1 cm3) of the right midfoot present for over 1 year [Figure 1A]. Previous medical history included diabetes, coronary heart disease, cancer, chemotherapy, obesity, hypertension, chronic kidney disease, Charcot foot, and peripheral neuropathy. Previous treatment included sharp debridement, advanced wound dressings, and offloading. MRI identified an adventitial bursa, thick-walled fluid collection, measuring 5.3 x 1.0 x 5.8 cm3 communicating with plantar midfoot ulcer, along with soft tissue edema consistent with cellulitis. The resulting diagnosis was infected adventitial bursa with potential early acute osteomyelitis. Wound biopsy was negative for malignancy. Surgical debridement for osteomyelitis and excision of the infected bursa were performed [Figure 1B]. The patient was discharged to a long-term acute care facility where she received NPWTi-d with ROCF-CC dressings [Figure 1C]. After 48 days, NPWTi-d was discontinued, and HBOT, antimicrobial wound matrix, and placental allograft applications were initiated. The patient underwent 40 treatments of HBOT, 5 placements of native Type 1 collagen matrix with polyhexamethylene biguanide (PHMB) dressing, and 3 placements of placental allograft [Figures 1D and 1E]. The patient was fitted for a Charcot restraint orthotic walker to support offloading. The wound was fully healed 140 days after presentation [Figure 1F].
Case study 2
A 73-year-old female presented with a Stage 4 pressure injury (7.0 x 5.2 x 6.3 cm3) of the left heel present for 7 days. Previous medical history included diabetes, obesity, hypertension, congestive heart failure, Charcot foot, gout, hyperlipidemia, hypertrophia, cardiomyopathy, neuropathy, and incontinence. Previous treatment included sharp debridement, alginate dressings with active leptospermum honey, and povidone-iodine solution. The initial wound was 88% closed when her caregiver went away for 7 days [Figure 2A]. During this time, the wound deteriorated [Figure 2B]. MRI findings were negative for osteomyelitis and wound biopsy was negative for malignancy. Sharp debridement was performed followed by application of wound dressings and offloading at home [Figure 2C]. Due to limited wound improvement, the patient was admitted to a long-term acute care facility and NPWTi-d was initiated to promote granulation tissue development, remove debris, infectious material, and non-viable tissue, as well as prepare the wound bed for an STSG [Figure 2D]. After 26 days of NPWTi-d, healthy granulation tissue covered the wound bed [Figure 2E]. NPWTi-d was discontinued, and use of advanced wound dressings initiated.
Case study 3
A 72-year-old female presented with a neuropathic ulcer on the planter surface of the right heel (5.6 x 4.5 x 2.3 cm3 with probing to bone, Figure 3A) present for over 8 years. Patient medical history included obesity, hypertension, hyperlipidemia, autoimmune hepatitis, degenerative disk disease, and neuropathy. Previous wound management included sharp debridement, antimicrobial dressings, collagen dressings with silver, and hydrofiber dressings. However, these treatments failed, and wound closure was not achieved. The patient was admitted to a long-term acute care facility. Wound biopsy was negative for malignancy and MRI was negative for osteomyelitis. Surgical debridement was performed. Following debridement, NPWTi-d with ROCF-CC dressing was initiated with the goals of wound bed preparation, removal of infectious material, and promoting granulation tissue development [Figure 3B]. After 14 days, healthy granulation tissue covered the wound bed and an STSG procedure was performed. Traditional NPWT (3M™ V.A.C.® Therapy, 3M Health Care) was utilized as a bolster for the STSG with dressing changes every 3-5 days. Eight days post-grafting, NPWT was discontinued, and the patient was discharged home [Figure 3C]. The wound was fully closed 51 days after presentation. Upon wound closure, the patient was fitted with a custom ankle foot orthosis brace and extra depth shoes. The wound remained closed 38 days after grafting [Figure 3D].
Discussion
Chronic, non-healing lower extremity ulcers are difficult to manage and often carry a risk of amputation, particularly in patients with diabetes (Frykberg and Banks, 2015; Lin et al, 2020; Crocker et al, 2021). Often, advanced wound care modalities are utilized to manage these ulcers. One modality, NPWTi-d with ROCF-CC dressings can provide hydromechanical removal of infectious materials, non-viable tissue, and wound debris, while promoting granulation tissue formation. The use of NPWTi-d with ROCF-CC dressings in two patients with diabetic foot wounds, and one patient with a non-healing, lower extremity wound resulted in the removal of debris, infectious material, and non-viable tissue along with development of granulation tissue in the wound bed. Additionally, these patients were able to avoid amputation when the combined care plan that included NPWTi-d with ROCF-CC dressings, HBOT, and advanced wound dressings were employed.
Patients living with chronic lower extremity wounds have oftentimes exhausted previous wound care treatments without achieving wound bed optimization and have failed to go on to closure. The author routinely uses NPWTi-d in patients with hard-to-heal wounds of the lower extremity and has observed that NPWTi-d with ROCF-CC dressings provide hydromechanical removal of wound debris, non-viable tissue, and promotes robust granulation tissue formation. When using NPWTi-d with ROCF-CC dressings for wound bed preparation, the author has been able to successfully close many hard-to-heal wounds of the lower extremity. He has found that NPWTi-d sets the stage for advanced wound care modalities such as STSG and/or the use of cellular tissue products. NPWTi-d with ROCF-CC dressings should be considered as one of many tools in the wound care providers’ toolkit when faced with challenging and hard-to-heal wounds of the lower extremity.
Conclusion
NPWTi-d with ROCF-CC dressing use helped remove debris, infectious material, and non-viable tissue and promoted granulation tissue development in these 3 patients. The comprehensive wound care plan that included NPWTi-d with ROCF-CC dressing, HBOT, and advanced wound dressings helped with limb preservation.