Hypertension can be present in up to two thirds of patients living with diabetes (Pavlou et al, 2018). It is an important risk factor for atherosclerotic cardiovascular disease (ASCVD), heart failure and microvascular complications. In primary care settings, almost 40% of individuals with type 2 diabetes mellitus are already hypertensive at diagnosis (The Hypertension in Diabetes Study Group, 1993). Individuals with type 2 diabetes, compared with those without the condition, have increased cardiovascular morbidity and mortality (Martín-Timón et al, 2014). Diabetic vascular disease is associated with a 2–4-fold increase in the incidence of coronary heart disease and stroke, and 2–8 times the risk of heart failure (Boccara and Cohen, 2004).
Important meta-analyses have shown that antihypertensive therapy reduces ASCVD events, heart failure and microvascular complications in people with diabetes (Emdin et al, 2015; Ettehad et al, 2016). The Steno-2 study has shown that large benefits are seen when multiple risk factors, including hypertension, are addressed simultaneously (Gæde et al, 2016). Fortunately, there is evidence that ASCVD morbidity and mortality have decreased for people living with diabetes since 1990 (Rawshani et al, 2017; Gregg et al, 2018) and this may be due to improvements in part in blood pressure (BP) control (Ali et al, 2013).
Trial evidence for the management of hypertension
Epidemiologic analyses show that BP greater than 115/75 mmHg is associated with increased rates of ASCVD (Forouzanfar et al, 2017). Trial evidence highlighting the importance of BP management in people living with diabetes comes from two types of clinical trial: those in which glycaemic control and BP is concurrently monitored, and those that analyse ASCVD outcomes in subsets of subjects with diabetes in hypertension studies. Meta-analyses have added additional value.
The first trial to really highlight the importance of BP management in type 2 diabetes, the UKPDS (UK Prospective Diabetes Study), showed that targeting BP reduced composite microvascular and macrovascular diabetes complications by 24% (UKPDS Group, 1998). Each 10-mmHg reduction in systolic pressure was associated with a 15% reduction in the risk of cardiovascular disease (CVD) death over 10 years (Adler et al, 2000).
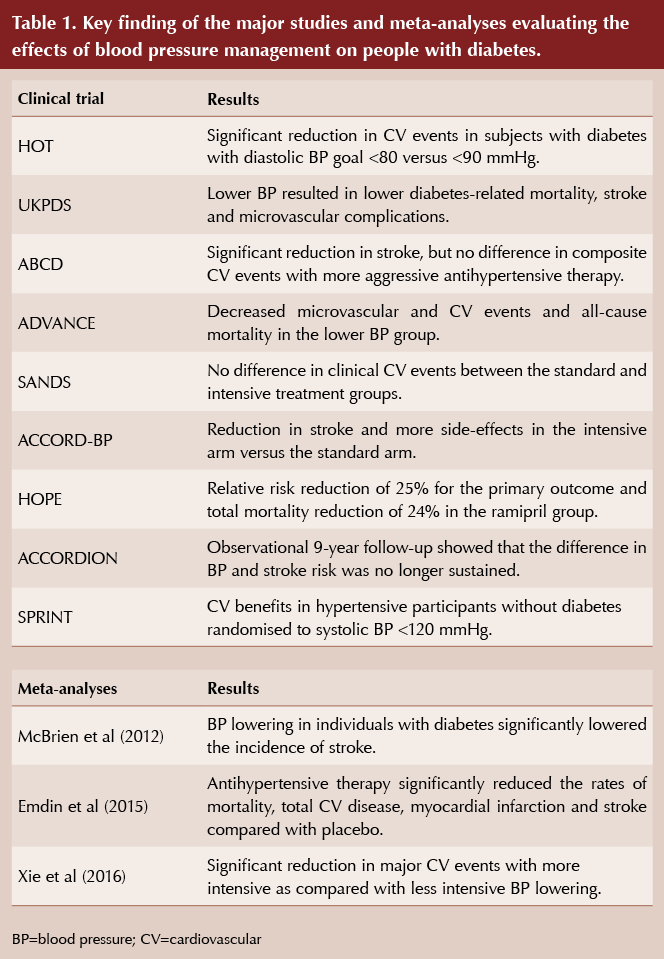
Table 1 summarises subsequent trials and meta-analyses in people with diabetes living with hypertension. In the HOT (Hypertension Optimal Treatment) trial, almost 19000 participants were randomly assigned to achieve average diastolic values of ≤90, ≤85 or ≤80 mmHg (Hansson et al, 1998). In a subset of 1501 participants with diabetes, the relative risk of a CVD event was significantly reduced in the ≤80 mmHg group compared to the ≤90 mmHg group.
The normotensive ABCD (Appropriate Blood pressure Control in Diabetes) trial enrolled 500 participants with type 2 diabetes into a moderate control (placebo) arm or an intensive control arm. The latter was set a target diastolic BP 10 mmHg below the initial baseline level, using either enalapril or nisoldipine (Schrier et al, 2002). At 5 years, mean attained BP for the moderate and intensive control groups were 137/81 and 128/75 mmHg, respectively. Intensive BP control slowed progression of retinopathy and albuminuria. Apart from a significant reduction in stroke, there was no difference in composite cardiovascular events with more aggressive antihypertensive therapy.
The ADVANCE trial assessed the use of a perindopril/indapamide fixed combination as the antihypertensive treatment in individuals with type 2 diabetes of long duration who were at high risk of vascular complications (Patel et al, 2007). The baseline BP was 145/81 mmHg and no BP goal was aimed for. Over 11000 people were studied and a placebo arm was included. The mean BP values were 134.5/74 (active therapy) versus 140/76 mmHg (control) after 4 years. The intensively treated group had fewer macro- and microvascular events, and decreased CVD mortality (3.8% vs 4.6%) as well as all-cause mortality (7.3% vs 8.5%). Taking into account a post-trial observational phase of 6 years, all-cause mortality was significantly lower among those in the lower BP group.
The SANDS (Stop Atherosclerosis in Native Diabetics Study) trial showed that reducing LDL-C and systolic BP to lower targets resulted in regression of carotid intimal medial thickness and greater decrease in left ventricular mass in individuals with type 2 diabetes. Clinical events were lower than expected and did not differ significantly between groups (Howard et al, 2008).
The MICRO-HOPE (Microalbuminuria, Cardiovascular and Renal Outcomes–Heart Outcomes Prevention Evaluation) trial was a sub-study of the HOPE trial. 3577 subjects with diabetes (the majority type 2), aged 55 years and older, were randomised to receive ramipril or placebo for 5 years. This intervention led to a 25% relative risk reduction for the primary outcome (cardiovascular death, non-fatal stroke, non-fatal myocardial infarction [MI]), and total mortality reduction of 24% in the ramipril group (HOPE Study Investigators, 2000).
The DASH (Dietary Approaches to Stop Hypertension) eating pattern is rich in fruits, vegetables and low-fat dairy foods. Investigators have demonstrated that it has beneficial effects on the cardiometabolic parameters of people with type 2 diabetes (Azadbakht et al, 2011).
In people with primary hypertension, weight-loss diets have been found to reduce body weight and blood pressure. However, the magnitude of these effects is uncertain owing to the small number of participants and studies included in the analyses (Semlitsch et al, 2016).
Randomised clinical trials of intensive blood pressure control
The ACCORD-BP trial examined the effects of intensive BP control (systolic BP target <120 mmHg) versus standard BP control (systolic BP target <140 mmHg) among people with type 2 diabetes. In this trial, intensive BP control did not reduce total major atherosclerotic cardiovascular events, but did reduce the risk of stroke, at the expense of increased adverse events (The ACCORD Study Group, 2010). Specifically, compared with a target systolic BP <140 mmHg, a target systolic BP of <120 mmHg resulted in no significant difference in the primary composite outcome of MI, stroke or cardiovascular death (3-point major adverse cardiovascular event [MACE]).
A subsequent 9-year follow-up of the ACCORD-BP subjects, termed ACCORDION, demonstrated a significant interaction between glucose and BP control. The intensive treatment group had a significant 21% reduction in the primary endpoints (3-point MACE) compared to the standard group (The ACCORD Study Group, 2016).
The recently published SPRINT (Systolic Blood Pressure Intervention Trial) study (Wright et al, 2015) sparked controversy as among individuals at high risk for cardiovascular events but without diabetes, targeting a systolic BP of <120 mmHg, as compared with <140 mmHg, resulted in lower rates of fatal and non-fatal major cardiovascular events and death from any cause. Significantly higher rates of some adverse events were observed in the intensive-treatment group and observers have been critical of some of the methodologies.
Meta-analyses
A combined analysis of three of the previously mentioned trials (ACCORD-BP, ABCD and HOT) suggested that intensive BP lowering in people with diabetes significantly lowered the incidence of stroke, but not mortality or myocardial infarction (McBrien et al, 2012). A recent meta-analysis of 40 trials examined the effects of antihypertensive therapy in studies that ranged in duration from 6 months to 8 years. In >100000 subjects with diabetes, antihypertensive therapy significantly reduced the rates of mortality, total CVD, MI and stroke compared with placebo (Emdin et al, 2015).
Finally, a meta-analysis of 19 BP trials (including five that included individuals with diabetes), with a combined 44989 participants, found a significant reduction in major CV events with more intensive, as compared to less intensive, BP lowering treatments (with different BP targets). The effect of intensive BP lowering in the five trials that included people with diabetes was similar to other trials. All-cause mortality was also lower with intensive treatment, although it was not statistically significant (Xie et al, 2016).
Guidance
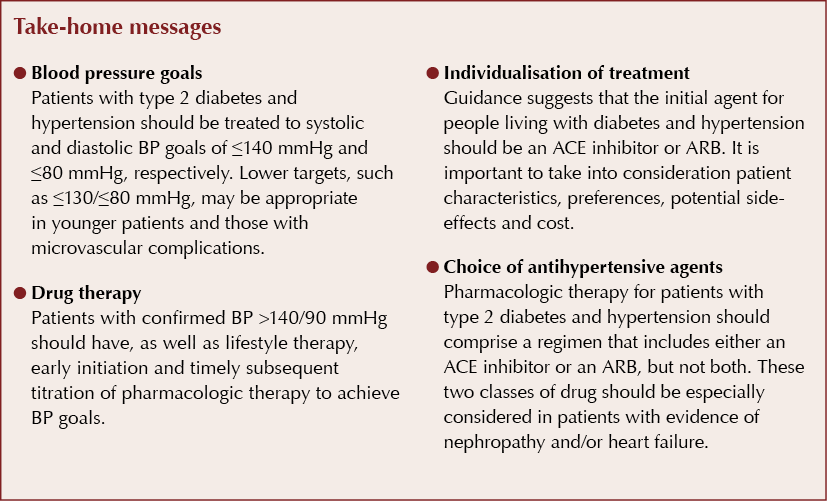
The healthcare professional working in primary care will be aware that all these trials are done in specific, often younger, populations and they do not always have generalisability in typical primary care settings. Both NICE (2015) and SIGN (2010) guidance broadly concur that the management of hypertension in people living with diabetes should be part of a shared decision-making process between the clinician and the individual patient. SIGN implies a slightly lower systolic BP reduction to a target of 130 mmHg.
These guidelines translated into achievement targets where over 50% of QOF (Quality and Outcome Framework) targets in diabetes care were related to hypertension management (http://bit.ly/2JjwiAP). Both sets of guidance suggest that appropriate medication needs to be offered if lifestyle advice does not reduce BP to <140/80 mmHg (<130/80 mmHg if there is kidney, eye or cerebrovascular damage). Blood pressure should be monitored every 1–2 months and intensified until it is consistently <140/80 mmHg.
First-line therapy in hypertension in a patient living with diabetes should be a once-daily, generic angiotensin-converting enzyme (ACE) inhibitor. If the person’s BP is not reduced to the individually agreed target with first-line therapy, then a calcium channel blocker or a thiazide or thiazide-related diuretic should be added. Additional therapy, such as an alpha-blocker or a beta-blocker, may be added if targets are not achieved.
Although the aetiology is unknown, as a group, people of African ancestry respond better to calcium blockers and diuretics, while the response to beta-adrenergic blockage and inhibition of the angiotensin converting enzyme is attenuated (Brewster and Seedat, 2013). In keeping with the need to individualise antihypertensive therapy, this is an important consideration in people living with diabetes who self-define as being of African ancestry.
We know that treatment medications, such as calcium channel blockers, have shown no teratogenic effects when used in the first trimester and have not demonstrated alterations in uterine flow compared to ACE inhibitors, angiotensin receptor blockers (ARBs), beta-blockers and diuretics. The calcium antagonists appear to be a favourable option in a population of women with hypertension who have child-bearing potential (Tellez-Mendez et al, 2015).
Summary
Hypertension is a strong, modifiable risk factor for the macrovascular and microvascular complications of diabetes. A number of trials over the years have highlighted the importance of lowering BP in people with diabetes, with benefits shown across a range of antihypertensive medications. Evidence from clinical trials and meta-analyses supports targeting BP reduction to at least 140/80 mmHg in most adults living with diabetes. In selected patients with high cardiovascular risk or microvascular complications, lower BP targets can be appropriate.
Contemporary guidance emphasises that any prescription should be part of a shared decision-making process between the healthcare professional and the individual patient. When patients have any degree of albuminuria, an ACE inhibitor or ARB should be part of the antihypertensive regimen. Treatment should be individualised to the specific patient and based on their comorbidities and their anticipated benefit from reduction in ASCVD, heart failure, progressive diabetic kidney disease and retinopathy events – all set against the risk of adverse events.





Jane Diggle examines the draft update to the NICE NG28 clinical guideline, plus new advice regarding the discontinuation of Levemir.
10 Sep 2025