The diabesity epidemic
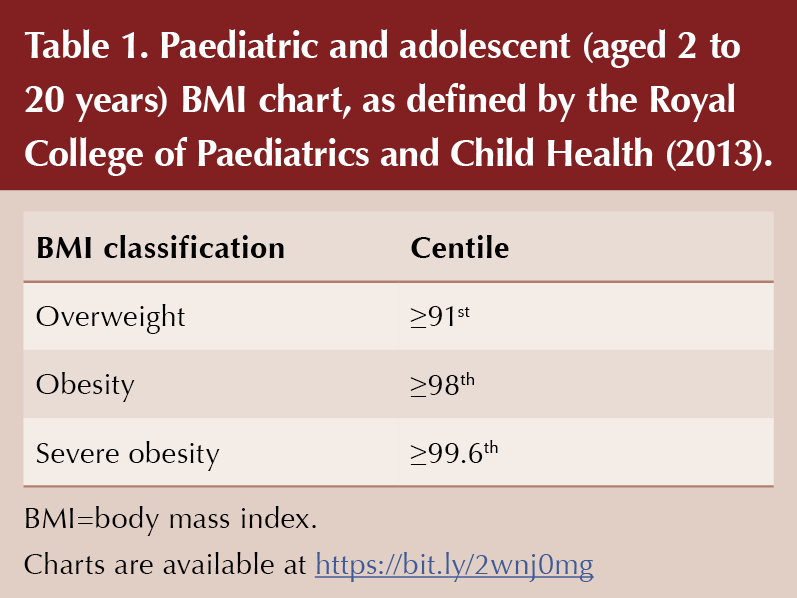
Obesity has rapidly become one of the greatest health threats in the UK and is projected to overtake smoking as the biggest human-generated burden on the economy (Dobbs et al, 2014). The exponential rise in childhood obesity (defined in Table 1) over the last three decades is particularly alarming, with almost half of UK children soon to be classed as overweight or obese (Royal College of Paediatrics and Child Health, 2018). Obese children are likely to become obese adults, and with that comes the development of obesity-related complications. The “diabesity” epidemic (coexistence of type 2 diabetes and obesity) also invalidates the belief that type 2 diabetes represents a disease burden purely on the older population.
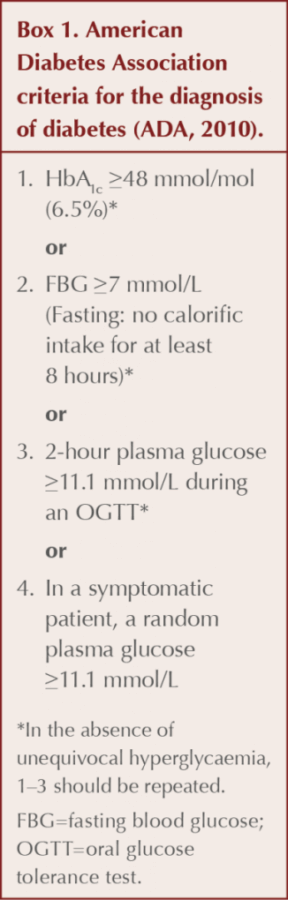
Over the last decade, HbA1c testing has become the principal diagnostic tool for the diagnosis of type 2 diabetes in asymptomatic adults (International Expert Committee, 2009), with a threshold of 48 mmol/mol (6.5%) being adopted. The main advantage is that HbA1c testing does not need to be conducted at a time of fasting, has less intra-individual variability and has been shown to be more reproducible than plasma glucose levels (Kapadia, 2013).
Extrapolating HbA1c to the paediatric population
The International Expert Committee (2009) made similar recommendations for HbA1c testing in asymptomatic children, which was also adopted by the American Diabetes Association (2010; Box 1). This has proved more controversial, not least because an HbA1c threshold of 48 mmol/mol (6.5%) in a paediatric cohort had not been properly validated as a diagnostic tool (Kapadia, 2013). Furthermore, HbA1c correlation studies in children and adolescents have been somewhat conflicting when applying sensitivity and specificity values for diabetes diagnosis at this HbA1c threshold (Lee et al, 2011; Nowicka et al, 2011; Kim et al, 2019).
Other reported disadvantages of utilising HbA1c include variability between different age and ethnicity groups, as well as haemoglobinopathy and iron deficiency states (Kapadia, 2013). Furthermore, the presentation of type 1 diabetes in children and adolescents often has a rapid course and, in such patients with significant hyperglycaemia, an elevated HbA1c will not be immediately reflected.
Considering the above, many authorities would not routinely recommend using HbA1c as a diagnostic tool for type 2 diabetes and prediabetes in children and adolescents (Diabetes UK, 2019), and instead advocate the use of an oral glucose tolerance test (OGTT) as the gold standard.
An OGTT, however, is not without limitations. It is costly, inconvenient, not particularly expeditious and, in many cases, not directly available to primary care physicians. Combining HbA1c and fasting blood glucose (FBG) tests as a screening tool for high-risk asymptomatic children may, therefore, provide a pragmatic solution for clinicians.
The two cases in this article illustrate the alarming trend in childhood obesity and are likely to represent the tip of an iceberg of a large subgroup that has fallen under the radar. This is especially true for the South Asian population, who are at increased risk of developing the condition.
Case histories
Patient A
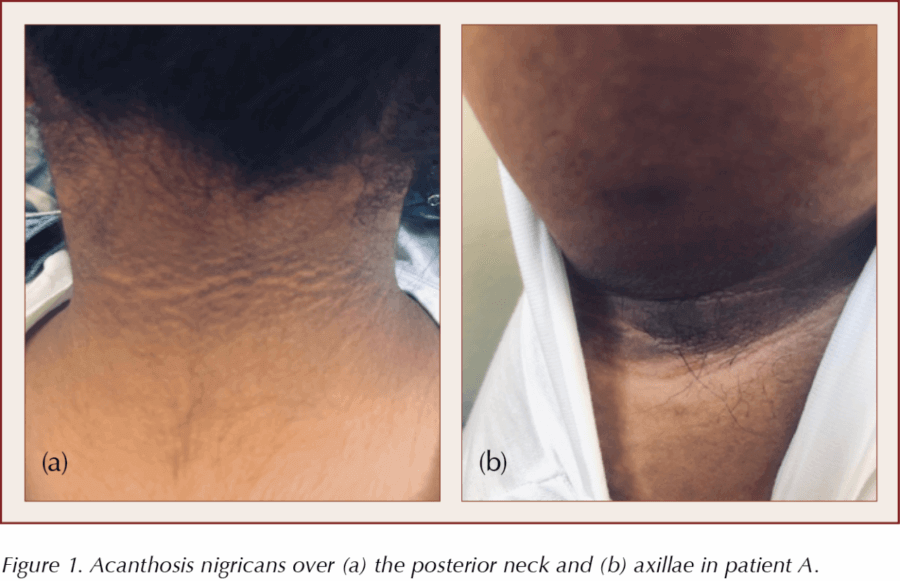
An 8-year-old girl of South Asian ethnicity presented because of concerns of “dirty marks” over her neck, axillae and groin regions. The areas of discolouration were not itchy or causing any particular symptom, other than being unsightly. The child was otherwise asymptomatic and denied any fatigue or osmotic symptoms. Her mother was concerned that her weight had increased significantly over the preceding years, but freely admitted that physical inactivity and a regular high calorific intake had contributed to this.
On examination, the child’s weight was recorded as 62 kg, with a calculated BMI of 27.6 kg/m2. Her BMI-for-age was plotted above the 99.6th centile, placing her in the severely obese category.
There were no dysmorphic features or evidence of underlying Cushing’s syndrome. Examination of the nape of the neck, axillae and groin revealed prominent ill-defined, darkened and velvety patches that were consistent with acanthosis nigricans (Figure 1).
Laboratory evaluation revealed normal FBG (4.8 mmol/L). HbA1c was elevated at 44 mmol/mol (6.2%). This was repeated after several weeks and had risen to 45 mmol/mol (6.3%).
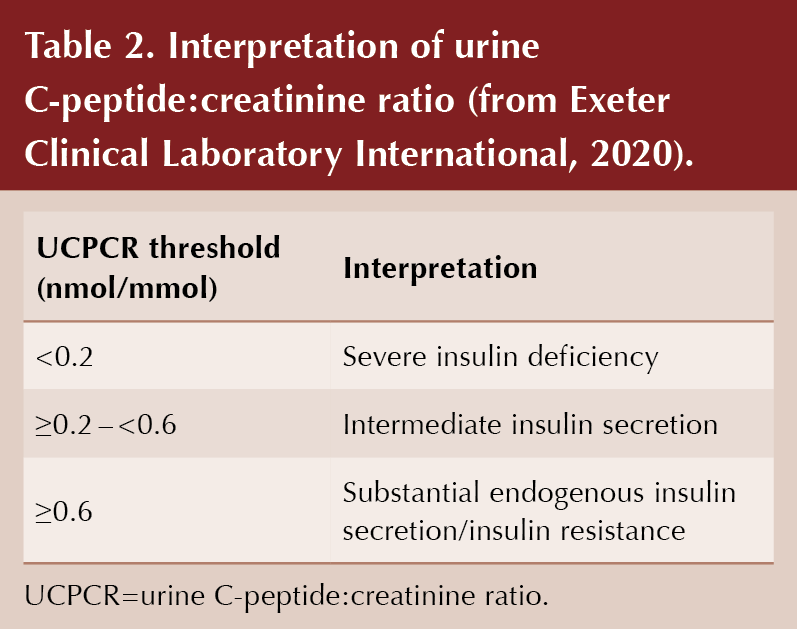
Tests for glutamic acid decarboxylase (GAD) antibodies and pancreatic islet cell antibodies (PICA) were negative. Two-hour post-prandial urine C-peptide:creatinine ratio (UCPCR) was additionally requested and reported at 8.3 nmol/mmol, indicating very substantial endogenous insulin secretion.
A discussion with the child’s mother about the importance of immediate lifestyle intervention was held – and the advice subsequently applied – whilst awaiting routine paediatric input.
The girl was reviewed after several months by a paediatric endocrinologist. A formal OGTT revealed a normal result (baseline glucose of 4.5 mmol/L, rising to 7.2 mmol/L at 2 hours). Importantly, her clinic HbA1c had fallen to 40 mmol/mol (5.8%), which reflected her recent dietary modification. No medication was initiated and she was subsequently discharged back to primary care, with a request for onward referral to a weight management service.
Patient B
A 12-year-old girl of South Asian ethnicity presented because her mother was concerned about unhealthy snacking that included a preference of sugary foods and drinks. There was also a strong family history of type 2 diabetes. The girl was otherwise well, although relayed a history of mild, albeit intermittent, polyuria. There were no other osmotic symptoms of note.
A clinic weight of 59 kg was recorded, with a calculated BMI of 25.2 kg/m2. Her BMI-for-age was plotted above the 91st centile, which put her in the overweight category.
Examination of the skin folds revealed an ill-defined darkened patch over the nape of the neck consistent with acanthosis nigricans.
Random capillary glucose taken in clinic was normal. Laboratory evaluation revealed an FBG of 3.9 mmol/L. HbA1c was elevated at 49 mmol/mol (6.6%). This was repeated after 3 weeks and was still demonstrably elevated at 50 mmol/mol (6.7%). Tests for pancreatic antibodies were negative and 2-hour post-prandial UCPCR was reported at 0.76 nmol/mmol, indicating elevated endogenous insulin secretion.
The girl was urgently reviewed by a paediatric endocrinologist and given a blood glucose meter to record a combination of fasting and post-prandial readings, whilst awaiting a confirmatory OGTT. She was subsequently commenced on metformin.
Discussion
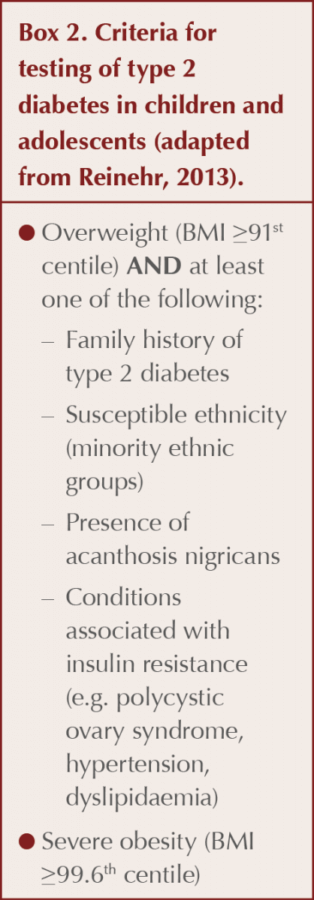
Testing for type 2 diabetes should be considered in all overweight children and adolescents who also have at least one of the following risk factors: a family history of type 2 diabetes; a susceptible ethnicity; presence of acanthosis nigricans; or a condition associated with insulin resistance, such as polycystic ovarian syndrome, hypertension or dyslipidaemia. Severe obesity alone may also necessitate testing (Box 2; Reinehr, 2013).
Negative pancreatic antibody screening (and elevated UCPCR) is expected in overweight or obese children (especially if other clinical features of insulin resistance are present) and is usually only warranted when there is a doubt about the aetiology of prodromal hyperglycaemia. It must be noted that these specialised tests are not widely available to primary care and cost may additionally limit their routine use. A UCPCR test, however, offers a practical and non-invasive means of measuring endogenous insulin production. A single urine sample taken 2 hours after a meal will remain stable for several days when preserved in a boric acid container, allowing transport to specialist laboratories for analysis (Bowman et al, 2012). A UCPCR threshold of >0.6 nmol/mmol is associated with substantial endogenous insulin secretion (Table 2). The UCPCR value mirrors the clinical features of insulin resistance, underlining the importance of urgent lifestyle modification.
Should HbA1c be used at all for diabetes screening in children?
The routine use of HbA1c as a diagnostic tool for diabetes in children remains controversial. The major concern is that an HbA1c threshold of 48 mmol/mol may not be sensitive enough, leading to a proportion of children who have type 2 diabetes being missed. In the cases above though, the FBG level was initially normal, highlighting the real concerns regarding day-to-day variability with FBG measurements. In contrast, HbA1c was raised, putting these individuals into the prediabetes and diabetes ranges, respectively. Furthermore, this was corroborated by clear clinical and biochemical evidence of insulin resistance in both cases.
The raised HbA1c findings also provided opportune moments for candid discussions with the respective families about instituting immediate lifestyle interventions whilst awaiting specialist review. This may not have been forthcoming had an FBG been relied upon solely. In addition, a direct OGTT request was not within the remit of primary care.
Whilst glycated haemoglobin may not be entirely relied upon as a diagnostic test for type 2 diabetes in children, there is a strong argument for its utility as a screening marker for diabetes when taken in combination with an FBG measurement. A single blood sample used for both tests may obviate the need for an OGTT in many cases. This is particularly important given the inconvenience of an OGTT.
With respect to screening for diabetes, a lower HbA1c cut-off in the paediatric population would seem intuitive, in light of concerns regarding the applicability of the current adult HbA1c threshold of 48 mmol/mol. The determination of a specific HbA1c cut-off that is highly sensitive (at the expense of a higher false positive rate) would be welcomed to ensure that patients do not fall through the net. The use of receiver-operating characteristic (ROC) curves from regression methods within larger series/observational studies may help identify the ideal HbA1c threshold at which an individual is deemed unlikely to have diabetes. OGTT provision could, therefore, be reserved for those high-risk asymptomatic children who are found to have an HbA1c above this agreed threshold.
The above should be incorporated within a comprehensive primary care pathway and include the provision of a multidisciplinary weight management service for children found to be at high risk. This is urgently required to properly tackle the growing challenges of the childhood obesity time bomb.





It is crucial that we review retinal screening reports prior to prescribing GLP-1 or GIP/GLP-1 receptor agonists.
6 Aug 2025