Questions by:
Pam Brown, GP, Swansea
Jane Diggle, Specialist Diabetes Nurse Practitioner, West Yorkshire
Q: When do raised triglycerides need specific management and how can they be reduced?
Triglyceride (TG) levels above 4.5 mmol/L require management. The management and actions needed depend on the level, as summarised in Table 1.
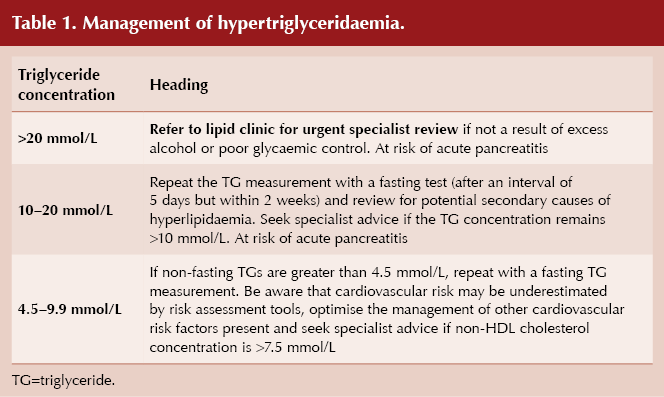
There are several potential secondary causes for hypertriglyceridaemia, and these should be explored and, where modifiable, acted upon when a high TG level is discovered. Secondary causes of hypertriglyceridaemia are listed in Box 1.
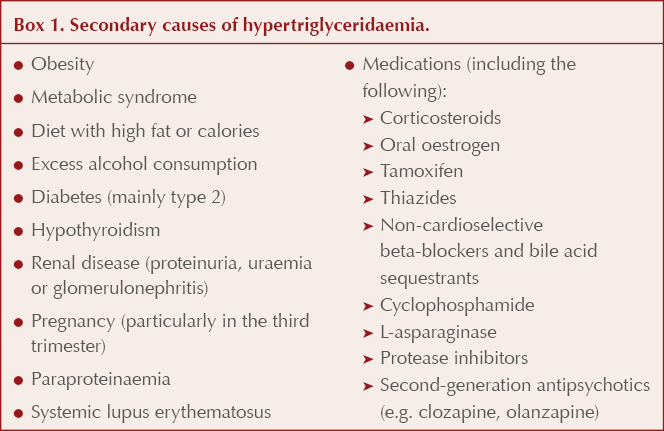
Where possible, people should be supported to correct possible secondary causes by, for example, reducing weight, improving diet, reducing alcohol intake and increasing exercise. Dietary changes should focus on reducing intake of sugar, total carbohydrates and fat.
Once secondary causes have been addressed and repeat TG levels have been taken, pharmacological treatment may be required to reduce levels.
For those with a repeat fasting triglyceride level of 4.5–9.9 mmol/L, atorvastatin 20 mg daily should be commenced if QRISK® score is greater than 10%. It should be noted that cardiovascular risk may be underestimated by risk assessment tools, as these do not factor TG levels into their algorithms.
For those with repeat fasting TG levels greater than 10 mmol/L, input from specialist services is required. Fenofibrate can be commenced at 200 mg daily, or at a reduced dose of 67 mg daily if eGFR is between 30 and 59 mL/min/1.73 m2, whilst further advice is awaited.
Anyone with elevated TG levels and current abdominal pain should be assessed for pancreatitis.
Q: If treatment targets are not achieved on maximum tolerated doses of a statin, what additional options are available and can these be initiated in primary care?
There are many options now available beyond statin therapy for lipid management, including ezetimibe, bempedoic acid, icosapent ethyl, PCSK9 inhibitors and inclisiran. Several of these can be initiated in primary care. These newer therapies are explored in this At a glance factsheet.
Q: Should ezetimibe be used alone initially, before use of ezetimibe/bempedoic acid combination? Can the combination be initiated in primary care?
Ezetimibe monotherapy should be used initially before use of the ezetimibe/bempedoic acid combination. Per NICE guidelines, summarised in the NHS England (2024) Summary of national guidance for lipid management, the response to ezetimibe monotherapy should be assessed after 2–3 months, whereupon the combination therapy may be considered if ezetimibe alone does not achieve target lipid reductions.
Bempedoic acid is a relatively new lipid-lowering therapy which inhibits cholesterol synthesis in the liver, thus lowering LDL cholesterol levels. It is licensed as follows:
● In adults with primary hypercholesterolaemia (heterozygous familial and non-familial) or mixed dyslipidaemia, as an adjunct to diet:
- In combination with a statin +/– other lipid-lowering therapies in patients unable to reach LDL cholesterol goals with the maximum tolerated dose of a statin, or
- Alone or in combination with other lipid-lowering therapies in patients who are statin-intolerant, or for whom a statin is contraindicated.
● In adults with established or high risk of atherosclerotic cardiovascular disease to reduce cardiovascular risk by lowering LDL cholesterol levels, as an adjunct to correction of other risk factors:
- In patients on a maximum tolerated dose of a statin with or without ezetimibe, or
- Alone or in combination with ezetimibe in patients who are statin-intolerant, or for whom a statin is contraindicated.
However, NICE (2021) TA694 guidance recommends bempedoic acid with ezetimibe as an option only when statins are contraindicated or not tolerated and when ezetimibe alone does not control LDL cholesterol sufficiently. Therefore, in practice in the UK, bempedoic acid is not commonly used with statin therapy.
Bempedoic acid when combined with ezetimibe produces an additional LDL cholesterol reduction of approximately 28% (range 22–33%), but no clinical outcome evidence for this specific combination is currently available. Treatment can be with separate tablets (Nilemdo®) or a fixed-dose combination (Nustendi®), which reduces tablet burden for patients. Nustendi® contains 180 mg bempedoic acid and 10 mg ezetimibe, enabling once-daily dosing. This can be initiated in primary care.
Q: When is it appropriate to refer for consideration of newer specialist lipid treatments, such as PCSK9 inhibitors?
Depending on a patient’s lipid dysfunction diagnosis, treatment targets and current medication regimen, referral to specialist services may be warranted. It is worth noting that, depending on local arrangements, in some areas PCSK9 inhibitors are not restricted to secondary care only, although generally these agents are initiated and monitored by specialists.
NICE lipid management guidance recommends considering referral in the following circumstances (NHS England, 2024):
● For management of primary prevention:
- If non-HDL cholesterol reduction remains <40% of baseline despite maximal tolerated lipid-lowering therapy (including people with intolerances and contraindications).
● For management of secondary prevention:
- If the lipid target is not met despite the maximum tolerated dose of lipid-lowering treatment, consider referral to a specialist lipid management clinic according to local arrangements.
● For management of severe hyperlipidaemia:
- Refer to lipid clinic for further assessment if any of the following:
⦿ Clinical diagnosis of familial hypercholesterolaemia.
⦿ Total cholesterol >9.0 mmol/L, LDL cholesterol >6.5 mmol/L, and/or non-HDL cholesterol >7.5 mmol/L.
⦿ Fasting triglycerides >10 mmol/L (regardless of family history). - Consider specialist referral for further treatment and/or consideration of PCSK9 inhibitor therapy if any of the following, despite maximal tolerated statin and ezetimibe therapy:
⦿ Very high risk of a coronary event (i.e. established coronary heart disease or ≥2 other cardiovascular risk factors).
⦿ Therapy is not tolerated.
⦿ LDL is >5 mmol/L (primary prevention).
⦿ LDL is >3.5 mmol/L (secondary prevention).
Q: How do PCSK9 inhibitors and inclisiran work, and how do these modes of action differ from statins?
The PCKS9 inhibitors, alirocumab (Praluent®) and evolocumab (Repatha®), are monoclonal antibodies. They bind to the PCSK9 pro-protein, inhibiting the breakdown of LDL receptors in the liver cells and thus increasing receptor numbers, raising capacity for cholesterol uptake and recycling.
Inclisiran (Leqvio®) also acts via the PCSK9 protein, in this case by inhibiting its production, increasing uptake of LDL cholesterol and thereby lowering levels in the blood.
By comparison, statins act primarily by inhibition of HMG-CoA reductase, the rate-limiting enzyme in the cholesterol biosynthesis pathway. Therefore, they work higher up the cholesterol pathway, while PCKS9 inhibitors and inclisiran work further downstream.
Q: Is there any role for omega-3 fatty acids, nicotinic acid or bile salt binders?
NHS England (2024) clearly stipulates: “Do not offer nicotinic acid, bile acid binder or omega-3 fatty acids alone or in combination with statin, for the prevention of CVD (check NICE NG238 and TA805 for exceptions).”
Icosapent ethyl, an omega-3 fatty acid, is the exception to this, and can be used with statin therapy to reduce the risk of cardiovascular events in certain high-risk people with raised triglycerides (see next section).
It should be noted that these recommendations apply to primary and secondary prevention of cardiovascular disease, including in people with diabetes and chronic kidney disease, only. They do not apply to people with familial hypercholesterolaemia. For further advice on use of these agents in people with this condition, NICE (2019) CG71 guidance should be followed. Generally, specialist advice is required.
Q: When should icosapent ethyl be considered?
Granted NICE approval in July 2022, icosapent ethyl (Vazkepa®) is the newest lipid-lowering therapy available in the UK market. NICE (2022) TA805 recommends icosapent ethyl as an option for secondary prevention of cardiovascular events in adults.
It is recommended if the person has a high risk of cardiovascular events and raised fasting triglycerides (≥1.7 mmol/L) and is taking statins, but only if they have:
● Established cardiovascular disease (defined as a history of acute coronary syndrome, coronary or other arterial revascularisation procedures, coronary heart disease, ischaemic stroke or peripheral arterial disease), and
● LDL cholesterol levels above 1.04 mmol/L and ≤2.60 mmol/L.
These recommendations were made as there are currently no treatment options to reduce the risk of cardiovascular events in people taking statins who have controlled levels of LDL cholesterol but raised triglyceride levels. Thus, this agent is suitable for a very specific cohort of patients.





Increased risk of new-onset heart failure in over-65s suggests caution is required before prescribing pregabalin for painful diabetic neuropathy.
14 Aug 2025