Questions by:
Pam Brown, GP, Swansea
Jane Diggle, Specialist Diabetes Nurse Practitioner, West Yorkshire
Q: In primary prevention, when is a statin recommended in people with diabetes (both type 1 and type 2)?
Statins are recommended in the following scenarios for people living with diabetes.
- For those with type 2 diabetes, atorvastatin 20 mg should be offered to people with a 10-year QRISK3 score of 10% or above.
– Note that NICE NG238 guidance advises not to rule out treatment just because a person’s QRISK3 score is less than 10% if they have a preference for commencing statin therapy or if there is concern that cardiovascular risk may be underestimated (NICE, 2023a).
- For those living with type 1 diabetes, statins (for choice, atorvastatin 20 mg) should be offered if one or more of the following circumstances apply:
– Older than 40 years.
– Diabetes duration of more than 10 years.
– Established nephropathy.
– Other cardiovascular risk factors.
Statin therapy should be considered for all people aged 18–40 years with type 1 diabetes, including those who have had diabetes for 10 years or less. It is worth considering therapy in this patient cohort as at some point they will meet the criteria above, and earlier conversations about lipid management ensure that people living with diabetes are informed about this element of their care and management.
Q: When are statins contraindicated?
Statins are contraindicated, and thus should not be prescribed, in the following situations (NICE, 2023b):
- Active liver disease.
- Unexplained persistent elevations of transaminases that are three-times the upper limit of normal or greater.
- Pregnancy or breastfeeding:
– Statins should be stopped if pregnancy is a possibility.
– Statins should not be restarted until breastfeeding has ended. - Women of childbearing potential not using contraception. Statins should be stopped 3 months before attempting to conceive.
Q: What follow-up is recommended after initiating a statin?
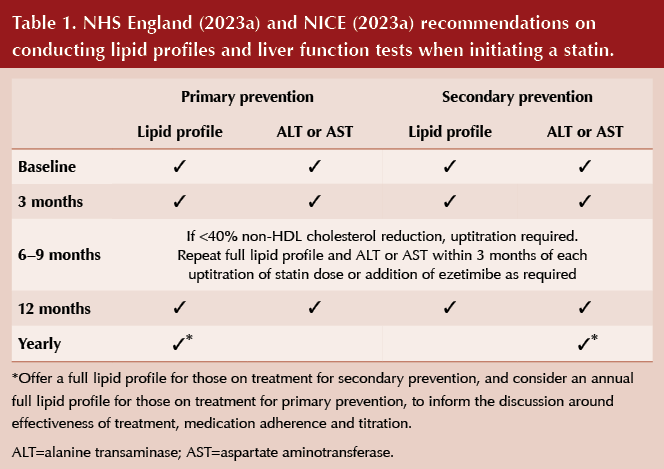
Following commencement of a statin, a full lipid profile and liver function tests (LFTs) should be repeated within 3 months, and then again at 12 months (see Table 1). LFTs do not then need to be checked again unless clinically indicated (e.g. at the time of signs or symptoms of hepatotoxicity).
Thereafter, NHS England (2024) and NICE (2023a) suggest to offer a full lipid profile for those on treatment for secondary prevention, and to consider an annual full lipid profile for those on treatment for primary prevention, to inform the discussion around effectiveness of treatment, medication adherence and titration.
If unexplained muscle symptoms (e.g. pain, tenderness or weakness) develop, creatinine kinase levels should be checked.
Medication reviews
An annual medication review should be conducted for all people on statins. During this review, the following should be discussed:
- Medicines adherence.
- Dietary and lifestyle changes, if appropriate.
- Address cardiovascular risk factors.
If the person is on low- or medium-intensity statin therapy, the likely benefits and potential risks of changing to a high-intensity statin should also be discussed.
Q: What rise in liver transaminases is acceptable after starting a statin?
As stated in Table 1, after commencement of statin therapy, liver transaminases should be measured within 3 months and then within 3 months of every additional uptitration, and then again at 12 months. This is to monitor for rises in liver transaminases.
If ALTs or ASTs are three-times the upper limit of normal (ULN) or greater, statin therapy should be discontinued and liver transaminases repeated in a month.
If ALTs or ASTs are elevated by less than three-times the ULN, statin therapy can be continued, with tests repeated in a month. If they remain elevated on repeat testing but are less than three-times the ULN, statin therapy can be continued and the tests repeated in 6 months.
Q: For primary prevention, what is the recommended first-line statin? And for secondary prevention?
- For primary prevention, the recommended first-line statin therapy is atorvastatin 20 mg daily.
- For secondary prevention, the recommended first-line statin therapy is atorvastatin 80 mg daily.
Q: How do the different statins compare in terms of efficacy and tolerability? If intolerant to atorvastatin, which statin should be tried next?
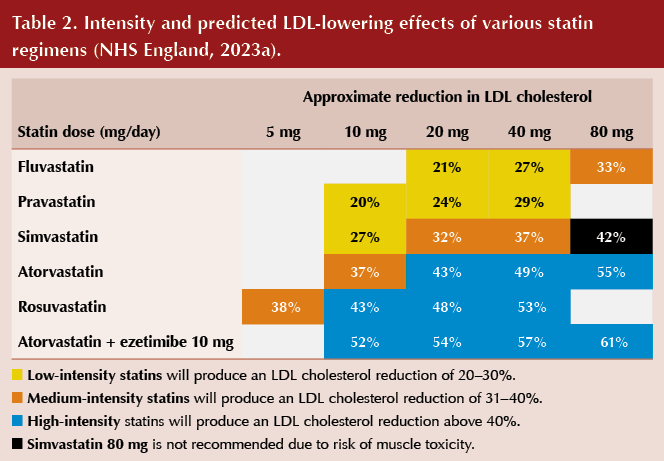
It is important to note that not all statins have equal efficacy. Table 2 summarises statin intensity in relation to LDL cholesterol reduction.
A person-centred approach should be adopted in cases of potential statin intolerance, including listening to the concerns of the patient, reinforcing lifestyle advice, discussing the aims of treatment, explaining the benefits of statin therapy, and evaluating and identifying any risk factors.
NHS England (2023) advocates that therapy with a lower-dose statin is preferred to no statin therapy at all, noting that any statin at any dose will reduce cardiovascular risk. A repetitive approach of rechallenging is recommended to establish whether the symptoms described are being caused by statin therapy. NHS England (2023) advises:
- Switching to a different statin or rechallenging with the same statin at a lower dose or frequency.
- If daily statin dosing is not tolerated, alternate-day or twice-weekly dosing is an option.
- Rosuvastatin and atorvastatin have longer half-lives, which facilitate their use in a non-daily regimen.
- Addition of ezetimibe to a lower-dose statin may be better tolerated.
It should be noted that the cardiovascular benefits have not been proven for the above suggestions; however, a good reduction in LDL/non-HDL cholesterol has been observed, and any reduction is deemed beneficial (NHS England, 2023). It is important to reiterate this to the person being treated. When a new regimen is tolerated, dose and/or frequency can be gradually increased to achieve targets.
If atorvastatin is not tolerated, then rosuvastatin is recommended as the next line by NICE (2023a), as this is in the same intensity group. If a person is not able to tolerate high-intensity statin therapy, then therapy should be with the maximal tolerated intensity and dose of statin.
Pharmacologically, it is also worth noting that statins are either water- or fat-soluble. Water-soluble statins are rosuvastatin and pravastatin; all others are fat-soluble. Some studies suggest that water-soluble statins may be better tolerated by those who develop muscle pain/symptoms, as these agents are less able to enter muscle cells.
Q: How can we support individuals who are reluctant to take a statin?
Statins have had a large amount of press coverage in recent years, which has led to many people having fervent opinions and potential misconceptions about this treatment choice. NICE (2023a) advocates that decisions regarding commencement of statin therapy should only be made after an informed discussion between the clinician and the person about risks and benefits of statin therapy.
NICE recommends taking into account:
- Potential benefits from lifestyle changes.
- The person’s preferences.
- Presence of comorbidities.
- Medication history, polypharmacy and tablet burden.
- Frailty.
- Life expectancy.
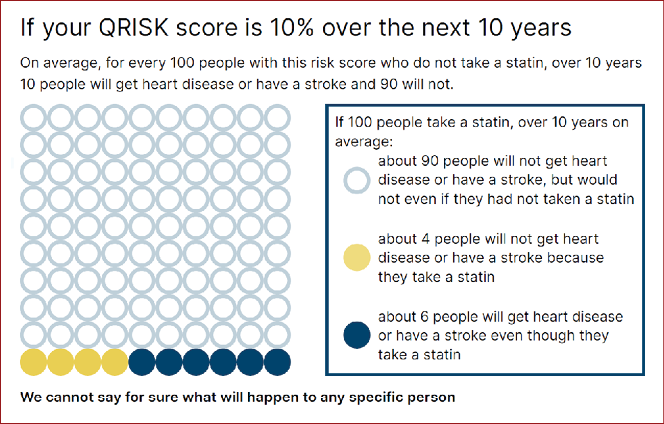
As part of this discussion, NICE specifies that all people being offered statin therapy should be informed that the risk of muscle pain, tenderness or weakness is small, and the rate of severe muscle adverse effects is extremely low. Within the NG238 guidance, NICE has produced a very useful patient decision aid, covering the need and rationale for statin therapy as well as side effects, which clinicians can use in consultations. The decision aid also includes infographics to help explain risk reduction, likelihood of side effects and QRISK scores, which some people may find helpful to visualise the information they are being told (see Figure 1 for an example).
NICE also states that, where a person’s cardiovascular risk warrants treatment but they decline this, the person should be advised that their cardiovascular risk should be reassessed in the future, and this should be documented in their medical records.
Q: What action should be taken in an individual who complains of muscular aches and pains after starting a statin? When should creatine kinase levels be checked?
In individuals who experience muscle aches and pains following starting statin therapy, the NHS England (2023) Statin Intolerance Pathway should be followed. This pathway will help consider whether the symptoms described are typical of statin-related muscle toxicity (SRM) and the relevant actions to take.
Options recommended by NICE (2023a) include:
- Stopping the statin and trying again when symptoms have resolved, to check whether the symptoms are related to the statin.
- Changing to a different statin in the same intensity group.
- Reducing the statin dose.
- Changing to a lower-intensity statin.
Creatinine kinase (CK) is recommended to be checked in individuals with:
- New onset or worsening of muscle symptoms which are typical of SRM (pain, tenderness or weakness) since starting statins.
- NHS England (2023) defines symptoms which are typical for SRM as “symmetrical pain and/or weakness in large proximal muscle groups, worsened by exercise”.
CK should not routinely be measured in asymptomatic people on statin therapy.
Q: Should statins be offered to people with diabetes over the age of 85 years?
In recent years, studies have been undertaken regarding the value of statin therapy depending on a person’s age. Ramos et al (2018) suggested that the effect of statin therapy in reducing incidence of cardiovascular disease (CVD) and all-cause mortality was lower after the age of 85 years and disappeared in nonagenarians. It was, therefore, felt that the widespread use of statins in old and very old populations was not supported, but use was recommended in people under 85 years living with diabetes.
NICE (2023a) does not specify an age cut-off to stop offering statin therapy, but it does suggest to take into account factors which may make treatment inappropriate, such as comorbidities, polypharmacy, general frailty and life expectancy.
Q: Where a baseline non-HDL cholesterol level is not known, what is the recommended target in people with diabetes when using a statin?
NICE advice was updated in December 2023, and now states that, for secondary prevention of CVD, aim for LDL cholesterol levels of ≤2.0 mmol/L or non-HDL cholesterol levels of ≤2.6 mmol/L irrespective of baseline (NICE, 2023a). This is broadly aligned with the Joint British Societies Consensus recommendation (JBS3 Board, 2014), which advocates, “Statins should be prescribed with a ‘lower is better’ approach to achieve values of at least <2.5 mmol/L for non-HDL-c (equivalent to <1.8 mmol/L for LDL-c)”, and noting that, “The concept of ‘lower is better’ is supported by evidence for LDL-c reduction”.
NICE does not currently offer any guidance on targets for primary prevention where the baseline non-HDL cholesterol level is unknown. Best practice and NICE advice would promote the use of baseline blood tests to guide treatment and titration, aiming for a reduction in non-HDL of >40% from baseline.
Q: What constitutes a cardiovascular risk factor when considering need for a statin?
The following cardiovascular risk factors are factored into the QRISK3 algorithm (available at: https://qrisk.org/index.php) for assessing need for statin therapy:
- Age.
- Sex.
- Ethnicity.
- Postcode.
- Smoking status.
- Diabetes status.
- Angina or heart attack in a first-degree relative aged <60 years.
- Chronic kidney disease (stage 3, 4 or 5).
- Atrial fibrillation.
- Blood pressure treatment.
- Migraine history.
- Rheumatoid arthritis.
- Systemic lupus erythematosus (SLE).
- Severe mental illness (including schizophrenia, bipolar disorder and moderate/severe depression).
- On atypical antipsychotic medication.
- On regular steroid tablets.
- Diagnosis or treatment for erectile dysfunction.
- Total cholesterol:HDL ratio.
- Systolic blood pressure.
- BMI.
Some of these factors are modifiable and others are not; therefore, it is important to tell people who may be being considered for statin therapy the nature of the factors and how they can help manage their own risk factors, whilst also acknowledging that this is a dynamic score.
Note that the recent NICE guideline updates advocate for a more person-centred approach, suggesting that atorvastatin 20 mg should be used as an option for people who want to take statins irrespective of their QRISK3 score, or where clinical judgement suggests the person may be at high risk of CVD; for example, if the person has cardiovascular risk factors not covered by QRISK3. NICE is clear in emphasising that “any statin at any dose reduces CVD risk”.
Q: When is it NOT appropriate to use a cardiovascular risk score?
QRISK3 is the tool of choice for CVD risk assessment in the UK. However, it is important to note that this should not be used in the following groups:
- People aged <25 years or ≥85 years.
- People with type 1 diabetes.
- eGFR <60 mL/min/1.73 m2.
- ACR ≥3 mg/mmol.
- Familial hypercholesterolaemia or other inherited disorders of lipid metabolism.
QRISK3 is only valid for patients who do not already have a diagnosis of coronary heart disease (including angina or heart attack) or stroke/transient ischaemic attack. Cardiovascular risk tools may also underestimate risk in certain groups of people (e.g. HIV; taking medications to treat CVD risk factors; recently stopped smoking; taking medicines that can cause dyslipidaemia, such as immunosuppressant drugs; severe mental illness; autoimmune disorders; other systemic inflammatory disorders).
People aged 85 years or older should be considered at an increased risk of CVD because of age alone, particularly those who smoke or have raised blood pressure; however, note the questionable benefits of offering statins in this group discussed previously (Ramos et al, 2018).






It is crucial that we review retinal screening reports prior to prescribing GLP-1 or GIP/GLP-1 receptor agonists.
6 Aug 2025