Business planning allows NHS organisations to make sure that the services they are commissioning or providing are well planned, meet the needs of the population and are financially viable. “Business cases” are pivotal to allow good business planning. Previously, the skill of writing a compelling business case was considered a task for NHS managers. With the changing landscape of the NHS, clinicians working in clinical commissioning groups (CCGs) and provider organisations, are now increasingly required to write business cases. This ensures that the services are clinically led and provides opportunities for effective communication with senior decision-makers.
A good business case provides justification for the proposed business change or plan, and includes an outline of what resources need to be allocated to implement it. It acts as a lever to move forward the proposed plan. It also allows the decision-makers to evaluate the proposal objectively in the context of local and national policies.
The following example is of a business case that we, the Diabetes Transformation Project Team, wrote to justify the proposed implementation of enhanced diabetes service provision in the community setting. This was the preferred option locally to improve care processes and outcomes for our population with type 2 diabetes.
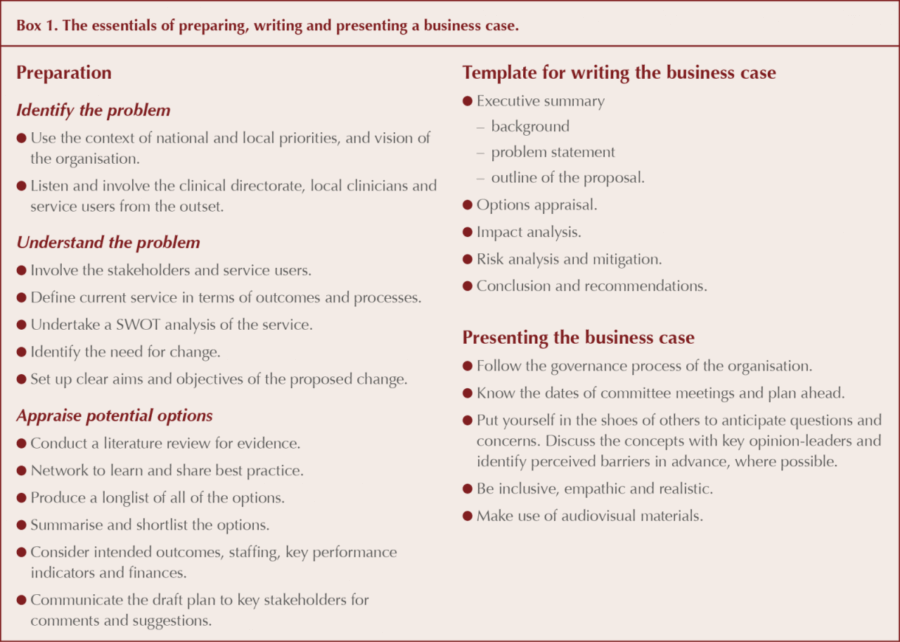
Preparation
1. Identify the problem
It was important to determine if the business case would fit into the overall context, strategy and vision of the organisations involved, to ensure the participation and support of the proposed change. Improving care and outcomes in diabetes was a priority for our CCG, as ours is one of the areas in the country with the highest prevalence of type 2 diabetes. The local clinical directorate and clinicians had brought the scope for improvement in this area to the attention of the CCG.
We referred to national policies, such as the NHS Outcomes Framework, which prioritises prevention and treatment of diabetes nationally, and the priorities set out by the Leicester City CCG, which included improving the quality of diabetes services in the city. We also consulted national policies, such as Moving Care Closer to Home and the Our Health, Our Care, Our Say White Paper, which would support our proposed business case.
2. Understand the problem
The next step was to understand the problem and the gap in the service provision using SWOT analysis (strengths, weaknesses, opportunities and threats). We reviewed the National Diabetes Audit data for our local area to identify areas where we were underachieving. To get a better picture of current performance, the data was supplemented with information from local intelligence, such as: outpatient department (OPD) utilisation at local hospitals; admissions with hypoglycaemia and other complications related to diabetes; and, most importantly, feedback from service users. This information was analysed against national benchmarks to demonstrate that there was scope for improvement in the service provision for diabetes in the city. We also included the current cost of service provision locally and compared it to other areas with similar demographics to make a case for cost–benefit improvements as well.
The following problems were identified in terms of process and outcomes:
Processes
- Fragmented service provision, with no defined pathway for primary and secondary care responsibilities, causing variation in referrals to OPD and poor service-user feedback.
- Low confidence among primary care healthcare professionals in the management of diabetes, owing to a lack of support and resources for upskilling.
Outcomes
- Low achievement of care processes and three treatment targets locally.
- High hospital admission with hypoglycaemia and diabetes-related complications.
Understanding the problems enabled us to set the following clear aims and objectives, and paved the way for us to consider options to achieve these.
- To improve the provision of eight care processes and to achieve three treatment targets (with a 3% improvement in each in the first year).
- To reduce by 5% inappropriate referral to secondary care (through enhanced service provision in primary care and by using locally agreed referral criteria, when appropriate).
- To define a unified pathway for the service across organisational boundaries to set up clear accountability for providers.
3. Appraise potential options
The purpose of this step was to identify a wide range of possible options to achieve the set objectives and to answer “how do we get there?”
Brainstorming sessions were held with clinicians and a designated managerial lead for diabetes. A public representative from Diabetes UK was included to obtain service-user feedback. The clinical lead in diabetes, a general practitioner and a consultant were tasked to review the literature, while the managerial lead agreed to gather information on diabetes service provision in other areas with similar demographics.
This step required an options appraisal, where options of “doing nothing” and “doing minimal” were also considered. For example, an option of just expanding the OPD to cope with the demand was appraised against the option of reducing the demand for OPD by improving the service provision in the community. A good option appraisal of proposed change would be more credible with the stakeholders and decision makers, as it would show that a careful thinking process had been conducted before conclusions were reached.
Based on the available evidence, the option of commissioning enhanced diabetes service provision in the community while integrating with the secondary care setting was considered as a feasible solution to the problem. In liaison with the CCG’s finance department, a draft cost–benefit analysis was conducted at this stage to determine the financial viability of the proposed model.
Before going on to write the business case, we took the draft plan outlined above to our GP reference group and finance department to get further comments and suggestions. We discussed the proposed change with key stakeholders to obtain their views and prior approval in principle.
Writing the business case
Executive summary
This section is very important as it gives a snapshot and overview of your business case, rather like an abstract in a research paper. We included the following in our executive summary.
Background
Current service provision in diabetes in the city was described briefly to inform the audience, including the decision makers.
Problem statement
We defined the problem and justification for the need for a change. We included the summary of analysis of current data, such as low achievement in eight care processes and the three treatment targets, OPD waiting times and acute admissions related to complications of diabetes, to define the problem. We included the results of a service-user feedback survey and the views of the public representative to reinforce our problem statement.
Outline of proposed solution
We described the proposed solution of commissioning an enhanced diabetes service provision in the community, which would be integrated with the secondary care settings. Key evidence was cited to justify the choice and a brief cost–benefit analysis included to provide reassurance that the proposed model would be financially viable. To support the solution, we also indicated how this proposed model complied with the current objectives and priorities, of the organisation and national policies.
Options appraisal and details of the proposal
Here, we elaborated further on options that we had considered and the reason for the preferred option. To reinforce our choice, we cited further evidence, and shared our knowledge of similar service provisions in other areas and their outcomes.
Then, we described the details of the proposed model by breaking it down into strategy and implementation/delivery. Under strategy, we defined the setting up of a steering group, identified stakeholders to form it, and provided a brief outline of this group.
The implementation plan was broken down into components, such as:
- Seeking expression of interest from GP practices to provide enhanced service.
- Training to upskill healthcare professionals.
- Monitoring and support of the programme.
In addition, a brief outline of project timelines was included in this section. Further details of financial modelling, including the cost–benefit analysis, were described here in detail.
Impact analysis
This section explores any potential impact on existing services and service users brought about by implementing the proposed change. This step is important, as it considers the different perspectives of existing and future stakeholders. This, in turn, can improve the chance of stakeholders accepting the proposed change by reassuring them that the potential impact on them has been acknowledged and discussed in the context of the greater good.
In our plan, we included consideration of the impact on staffing and recruitment; the capacity of GP practices; the potential impact on the financial viability of outpatient settings in secondary care; and changes in referral pathways, waiting times, and so on. For example, the impact on the workload of practices was discussed in both circumstances, along with the potential solution of employing staff with a skill mix to reduce the effect. Similarly, the impact on service users’ choice of care setting was considered, along with the option of allowing such a choice, when justifiable.
We also included the impact of not implementing the proposed change, which would result in further widening of the gaps in inequality of access to service, along with the potential for being unable to meet the cost of treating complications of diabetes in future.
Risk analysis and mitigation
This section describes what could go wrong with the proposed change, how likely these risks are and what could be done to mitigate them.
This step provides the proposed change with credibility by making it more realistic and applicable. We described the risks of not persuading enough GP practices to provide the service, not having enough staff to train and upskill, the potential of creating a two-tier service if only very few GP practices were willing to provide the enhanced service for their patients, and financial risks. Risk-scoring criteria were defined and applied to each risk, along with mitigation plans.
Conclusion and recommendations
This includes a summary of the business case and indicates the recommendations to be made to the executive team.
Presenting the business case
This is, perhaps, the most important and daunting task that needs to be done after writing the business case. We took our business case to our integrated governance committee (IGC), which governs the commissioning and oversight of clinical services in our CCG. We approached the key decision makers prior to the meeting to get their comments and queries on the business case, so that this could be reflected on when formally presenting the case.
We also conducted another brainstorming session to explore potential concerns that management and clinicians could have regarding the case. This enabled us to address these concerns in our presentation before they were raised at the meeting. For example, we were alerted to a concern regarding the selection procedure for practices being able to provide the enhanced services for their practice population. We addressed it by providing transparent criteria for the accreditation process as an appendix to the business case.
Reflection
Our business case was well received and implementation of the proposed change was accepted by the CCG board.
The strength of our approach was that we were able to define clear aims and objectives, which were achievable and relevant to the local needs and priorities. The proposed change was based on available evidence and included a careful thought process around its application in real-world setting. We learned that understanding the users is paramount to make sure the proposed services will meet their needs, rather than just clinical goals.
In conclusion, preparing and writing a business case is a challenging, yet rewarding, task. To be successful, it needs time to prepare well, to collect accurate information and to gain support from colleagues.




Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025