Abbreviations
ABPM=ambulatory blood pressure monitoring; ACEi=angiotensin-converting enzyme inhibitor; ACR=albumin-to-creatinine ratio; ARB=angiotensin receptor blocker; BP=blood pressure; CCB=calcium channel blocker; CKD=chronic kidney disease; CVD=cardiovascular disease; ECG=electrocardiogram; eGFR=estimated glomerular filtration rate; HBPM=home blood pressure monitoring; LFT=liver function tests; LVF=left ventricular hypertrophy; QOF=Quality and Outcomes Framework; RAS=renin–angiotensin system; TSH=thyroid-stimulating hormone; U&E=urea and electrolytes.
Need to know guide
For a brief summary of NICE blood pressure classification and targets in diabetes, click here.
What and why
● Hypertension is twice as common in people with diabetes, and coexistence of these conditions significantly increases the risk for coronary heart disease, left ventricular hypertrophy, congestive heart failure and stroke.1
● Nationally, a third of people with diabetes who have had a blood pressure (BP) measurement recorded in the previous 12 months are deemed to have uncontrolled BP.2
● NICE updated its Hypertension in adults: diagnosis and management (NG136) guideline in November 2023.3 This guidance overrides the BP recommendations that appeared in Type 2 diabetes in adults (NG28), last updated in June 2022.
● For those with diabetes and chronic kidney disease (CKD), refer to NICE Chronic kidney disease: assessment and management (NG203).4
● This document does not cover hypertension management in children or in women during pregnancy.
Measuring blood pressure
● Measure BP at least annually in a person without previously diagnosed hypertension or renal disease.
● Use validated equipment.
Select the correct cuff size:

● Promote a relaxed and temperate environment.
● Measure BP in both arms.
● Check pulse rate and rhythm. Do not use an electronic BP monitor in the presence of an irregular pulse.
● Measure BP in both arms. Repeat if difference between arms is >15 mmHg and, if difference remains >15 mmHg, use the arm with the higher reading for subsequent BP measurements.
Postural hypertension:
● In people with hypertension and diabetes, measure standing as well as seated BP. If systolic BP falls by ≥20 mmHg, or diastolic BP falls by ≥10 mmHg:
- Consider likely causes, including current medication.
- Manage appropriately (for example, for advice on preventing falls in older people, see NICE CG161).5
- Measure subsequent BP with the person standing.
- Consider referral to specialist care if symptoms of postural hypotension persist despite addressing likely causes.
● If the BP drop is <20 mmHg (systolic) or <10 mmHg (diastolic) but symptoms suggest postural hypotension, repeat the measurements with the person lying on their back.
● In people with a significant postural drop or symptoms of postural hypotension, treat to a target based on standing BP.
● Postural hypotension can occur secondary to autonomic neuropathy.6
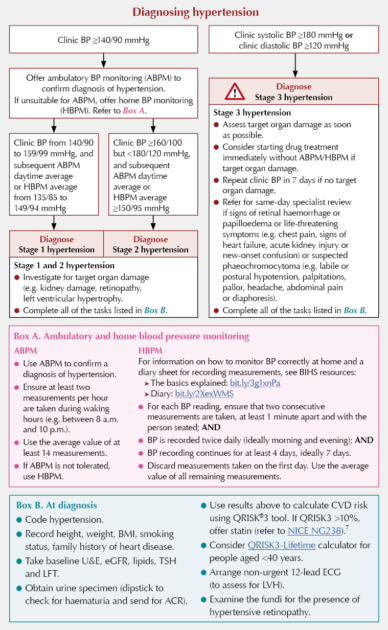
Diagnosing hypertension
Blood pressure targets
According to NICE,3,4 there is insufficient evidence to support the previously recommended lower BP targets for people with type 2 diabetes, other than for people with coexisting CKD and an ACR ≥70 mg/mmol.
The recommendation is to reduce and maintain BP to the targets in the Table below depending on the person’s age. BP targets are the same for people with and without cardiovascular disease.
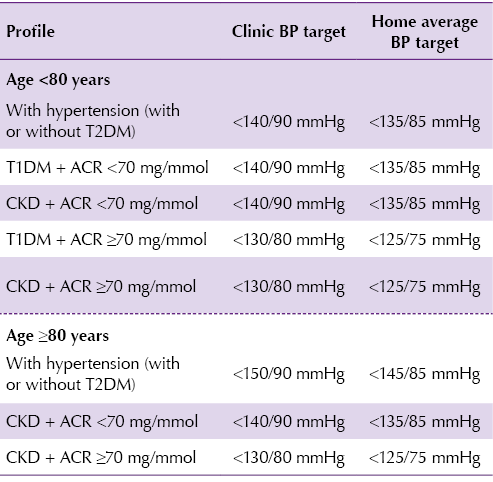
!!! Consider appropriate BP target level in special circumstances (e.g. those at risk of falls or postural hypotension, or with frailty, reduced life expectancy or polypharmacy).
Be mindful of low BP and consider reduction of treatment if a person’s systolic BP is <110 mmHg.
For adults <40 years, consider seeking specialist evaluation of secondary causes of hypertension, as appropriate.
KDIGO recommendations for people with CKD8
● Adults with high BP and CKD should be treated to a target SBP of <120 mmHg (also applies to the subgroups of older adults and those with increased albuminuria).
● The balance of benefits and harms is less certain in people with CKD G5 and in those with severely increased albuminuria (A3).
● The benefits of intensive BP lowering are less certain among patients with concomitant CKD and diabetes, compared to patients with CKD without diabetes.
2023/2024 QOF BP indicators
● Diabetes (excluding moderate or severe frailty: ≤140/90 mmHg
● Coronary heart disease/hypertension/stroke/TIA:
- Age <80 years: ≤140/90 mmHg
- Age ≥80 years: ≤150/90 mmHg
● There is no QOF BP target for those with CKD.
Treatment of hypertension
Lifestyle advice
● Ask about lifestyle. Where appropriate, offer lifestyle advice that includes healthy eating:
- A diet rich in a variety of vegetables, fruits and whole grains.
- Healthy natural fats (olive oil, nuts and fish) and dairy (milk, yoghurt and cheese).
- A variety of proteins, including seafood, lean meat, poultry, eggs, legumes, soy, seeds and nuts.
- Limit sugar-sweetened foods and drinks, refined carbohydrates and processed foods.
● The DASH (Dietary Approaches to Stop Hypertension) eating plan recommends reducing salt intake.
- Standard DASH = 2300 mg/day sodium (6 g salt); lower-sodium DASH = 1500 mg/day sodium (3–4 g salt).
● Support individuals who are overweight to lose weight.
● Offer smoking cessation advice to smokers (see Useful resources section).
● Provide information about local initiatives that support and promote a healthy lifestyle.
When to start/consider antihypertensive drug treatment
● Discuss individual CVD risk and preferences for treatment, including no treatment, and explain the risks and benefits before starting antihypertensive drug treatment.
● Continue to offer lifestyle advice and support them to make lifestyle changes.
● Offer antihypertensive drug treatment in addition to lifestyle advice to adults of any age with persistent stage 2 hypertension. Use clinical judgement for people of any age with frailty or multimorbidity.
● Discuss starting antihypertensive drug treatment, in addition to lifestyle advice, with adults aged <80 years with persistent stage 1 hypertension who have diabetes.
● Consider antihypertensive drug treatment in addition to lifestyle advice for people aged >80 years with stage 1 hypertension, if their clinic blood pressure is over 150/90 mmHg. Use clinical judgement for people with frailty or multimorbidity.
Special groups
● For choice of hypertensive agent in people with CKD, see NICE NG203 guideline on chronic kidney disease.4
● For women considering pregnancy or who are pregnant or breastfeeding, manage hypertension in line with NICE NG133 recommendations9 on management of pregnancy with chronic hypertension, and on antihypertensive treatment postnatally and while breastfeeding.
● For adults aged <40 years with hypertension, consider seeking specialist evaluation of secondary causes of hypertension and a more detailed assessment of the long-term balance of treatment benefit and risks.
Stepwise approach to the pharmacological management of hypertension in adults with type 2 diabetes
● Offer people with isolated systolic hypertension (systolic BP ≥160 mmHg) the same treatment as people with both raised systolic and diastolic BP.

Hypertension prescribing tips
● Do not offer a combination of ACEi and ARB.
● Indapamide should be used in preference to a conventional thiazide diuretic, such as bendroflumethiazide or hydrochlorothiazide.
● During intercurrent illness, especially where there is risk of dehydration, consider pausing ACEi/ARBs and diuretics until recovered.
● Measure serum potassium concentrations and estimate the GFR before starting RAS antagonists.
● Repeat these measurements between 1 and 2 weeks after starting RAS antagonists, and after each dose increase.
● Do not routinely offer an ACEi or ARB if pre-treatment serum potassium concentration is >5.0 mmol/L and STOP if it rises to ≥6.0 mmol/L.
● Following the introduction or dose increase of RAS antagonists, do not modify the dose unless either the GFR decrease from pre-treatment baseline is >25% or serum creatinine increase from baseline is >30%.
Useful resources
● British and Irish Hypertension Society (BIHS) educational resources and list of approved home BP monitors: https://bihsoc.org
● BIHS healthy eating diet sheet: bit.ly/2ZoZWyX
● DASH (Dietary Approaches to Stop Hypertension): https://dashdiet.org
● Diabetes UK Information Prescription on diabetes and blood pressure: bit.ly/2JtPH23
● QRISK3 cardiovascular risk calculator: https://qrisk.org
● How to help people with diabetes stop smoking: bit.ly/3j2hSsk





Benefits of SGLT2 inhibitors on CKD progression and hospitalisation for heart failure are similar regardless of diabetes status, uACR or eGFR levels.
24 Nov 2025