What is HbA1c?
HbA1c is a measurement of glycated haemoglobin. Glucose present in the bloodstream spontaneously binds to the haemoglobin in red blood cells in a process called glycation, with the amount of glucose that binds to the haemoglobin directly proportional to the level of glucose at that time.
After binding to the red blood cell, the glucose remains attached for the lifespan of the cell: usually around 12 weeks. Thus, HbA1c provides an indicator of average blood glucose levels over that period.
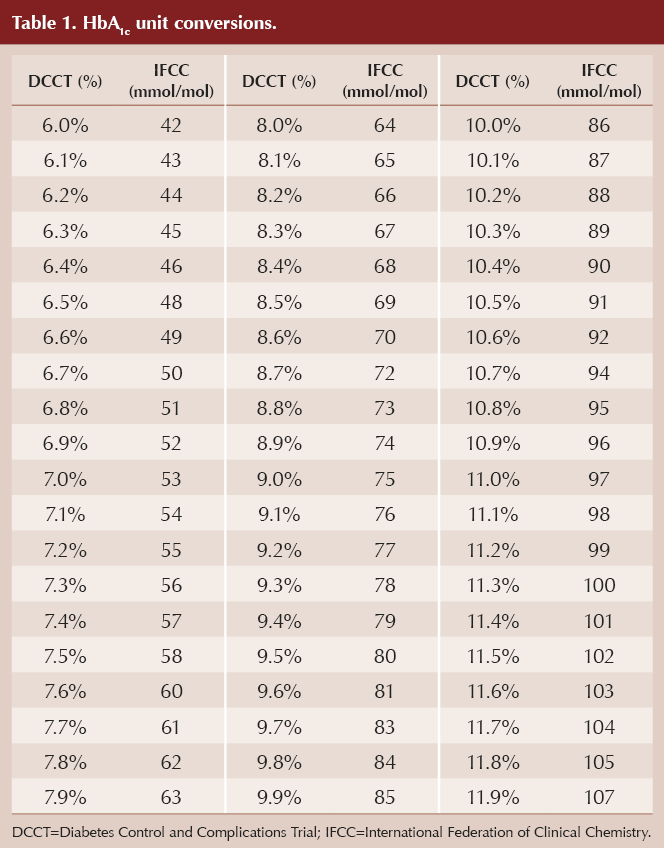
HbA1c levels may be reported either as a percentage or in mmol/mol. Since 2009, in the UK the standard unit of measurement has been mmol/mol, to align with the International Federation of Clinical Chemistry (see Table 1 for conversions).
HbA1c is useful in the diagnosis, prevention and monitoring of diabetes, as it reflects the impact of diet, lifestyle and medication on glycaemic control over the preceding 3 months.
When is HbA1c used in practice?
Monitoring glycaemic control
For decades, HbA1c has been used as the standard measure for monitoring glycaemic control in people living with diabetes. It was demonstrated to be an important predictor of diabetes-related complications in 1993, which led to the recommendation of specific HbA1c targets (DCCT Research Group, 1993).
Other landmark studies, including the UKPDS (Adler et al, 2024), have demonstrated the link between HbA1c and diabetes complications, reinforcing the use of these targets in people living with type 2 diabetes.
A note about glucose variability and hypoglycaemia
HbA1c is a biomarker of glucose control over the preceding 2–3 month period. It does not provide any insight into day-to-day glucose variability or provide evidence of hypoglycaemia. There are circumstances when such information is essential, in particular where a person is treated with blood glucose-lowering therapies associated with hypoglycaemia (e.g. sulfonylureas and insulin). To guide these treatment decisions, self-monitoring of capillary glucose should be utilised or, for individuals on insulin who meet the eligibility criteria, continuous glucose monitoring should be considered.
Diagnosing type 2 diabetes
The use of HbA1c was broadened in 2010, when the American Diabetes Association added it as a diagnostic criterion for type 2 diabetes. It has been standard practice in the UK to use HbA1c for diagnosing type 2 diabetes since 2011, when the World Health Organization (WHO, 2011a) published guidance on its use.
Use of point-of-care devices to assess HbA1c
Point-of-care (POC) testing devices for HbA1c measurement are available and may be used in some community settings. Such devices offer an immediate test result and operate via a finger-prick blood sample; thus, they do not require a trained healthcare professional to draw a venous blood sample. This clearly offers benefits, particularly in a community setting; however, concerns have been raised around the accuracy of this method. Recently, Sacks et al (2024) explored the advantages and disadvantages of POC HbA1c testing and concluded that, although it is convenient and useful for assessing glycaemic control in individuals with diabetes, it should not be used for diabetes diagnosis, due to lack of accuracy.
Diagnosing diabetes using HbA1c
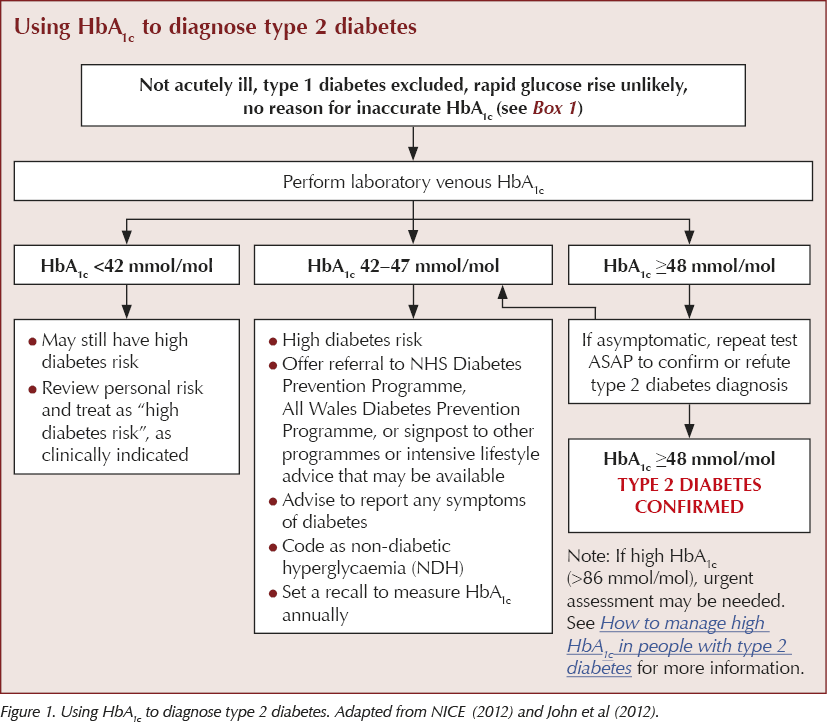
An HbA1c of 48 mmol/mol (6.5%) is used as the cut-off point for diagnosis although, as per the WHO (2011a) consensus, a value of less than this does not exclude diabetes diagnosed using other glucose tests (such as fasting glucose or an oral glucose tolerance test). This diagnostic threshold was chosen because it is the point at which the incidence of retinopathy, a common complication that may be present even before the actual diagnosis of diabetes is made, is increased (International Expert Committee, 2009).
WHO (2011a) recommends the following diagnostic criteria for diabetes:
- HbA1c below 42 mmol/mol (6.0%): Not diabetes.
- HbA1c 42–47 mmol/mol (6.0–6.4%): Impaired glucose regulation or prediabetes.
- HbA1c ≥48 mmol/mol (6.5%): Type 2 diabetes.
Importantly, individuals with a single elevated HbA1c between 42 and 47 mmol/mol are classified by NICE as having non-diabetic hyperglycaemia (NDH) and being at increased risk of developing type 2 diabetes. NDH is a clinical domain within the current NHS Quality and Outcomes Framework (QOF; NHS England, 2024). Practices are required to report on “the percentage of patients with non-diabetic hyperglycaemia who have had an HbA1c or fasting glucose performed in the preceding 12 months”, and this is currently worth 18 points with a threshold of 50–90%.
Progression to type 2 diabetes may be prevented or delayed in people with NDH through lifestyle changes with a focus on diet, weight loss and exercise. Referral to the National Diabetes Prevention Programme (or a local equivalent) is strongly advocated.
The process of using HbA1c to diagnose type 2 diabetes is summarised in Figure 1.
Situations where HbA1c is not appropriate for diagnosing diabetes
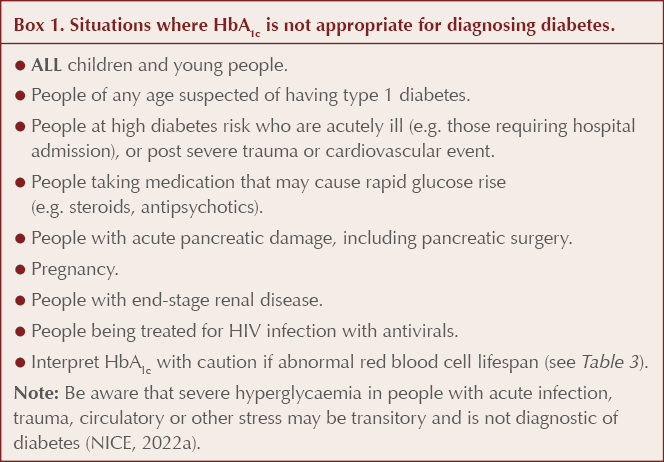
Because an HbA1c test may be performed at any time of day and does not require any preparation such as fasting, it has become the preferred method for diagnosing type 2 diabetes and assessing glycaemic control in those with diabetes. However, test results may be affected by a number of factors that impact the amount of glucose penetrating the red cell membrane, the rate of glycation or the lifespan of red blood cells (Radin, 2014; Kaiafa et al, 2021).
These factors must be considered when reviewing HbA1c results both for the purposes of making a diagnosis and in the ongoing management of diabetes. In particular, there are situations where it is not appropriate to use HbA1c to diagnose diabetes (Box 1).
Using HbA1c to monitor glycaemic control
In relation to HbA1c monitoring and agreeing targets, NICE (2022b) NG28 recommends the following:
Measure HbA1c levels in adults with type 2 diabetes every:
- 3 to 6 months (tailored to individual needs) until HbA1c is stable on unchanging therapy.
- 6 months once the HbA1c level and blood glucose-lowering therapy are stable.
Target setting
Clinicians are advised to discuss and agree an individual HbA1c target and encourage the person to reach their target and maintain it, unless there are resulting adverse effects (including hypoglycaemia) or their efforts to achieve their target impair their quality of life.
● For those managed either by lifestyle and diet, or lifestyle and diet combined with a single drug not associated with hypoglycaemia, aim for an HbA1c of 48 mmol/mol (6.5%).
● For those on a drug associated with hypoglycaemia, aim for an HbA1c level of 53 mmol/mol (7.0%).
● If HbA1c levels are not adequately controlled by a single drug and rise to ≥58 mmol/mol (7.5%):
- Reinforce advice about diet, lifestyle and adherence to drug treatment, and
- Aim for HbA1c 53 mmol/mol (7.0%), and
- Intensify drug treatment.
● Consider relaxing the target HbA1c on a case-by-case basis and in discussion with the individual, with particular consideration for people who are older or frailer, if:
- They are unlikely to achieve longer-term risk-reduction benefits (e.g. people with reduced life expectancy).
- Tight blood glucose control would put them at high risk if they developed hypoglycaemia (e.g. those at risk of falling, those with impaired awareness of hypoglycaemia, or those who drive or operate machinery as part of their job).
- Intensive management would not be appropriate (e.g. those with significant comorbidities).
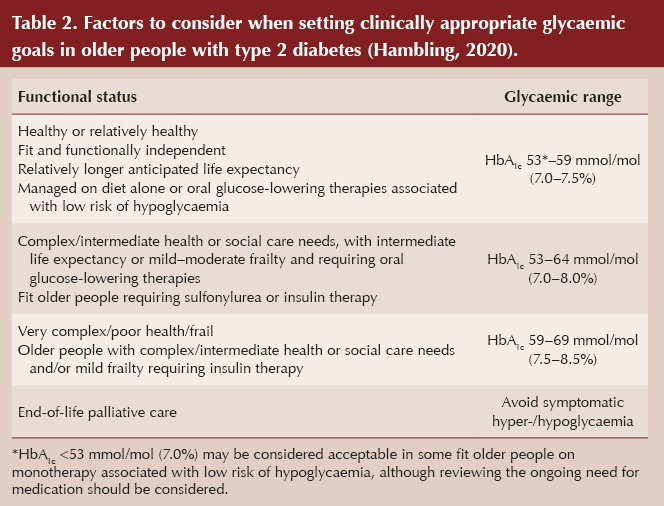
Notably, QOF allows for looser glycaemic control in people with frailty, with indicator IND180 being: “The percentage of patients with diabetes with moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months.”
Illustrative HbA1c targets for older people depending on their functional status are listed in Table 2 (Hambling, 2020).
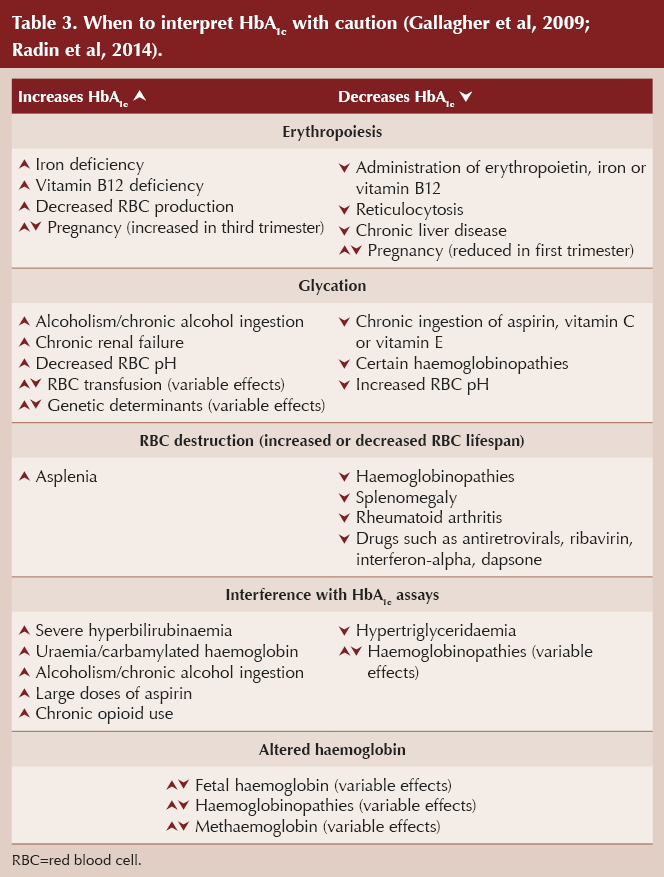
Monitoring glycaemic control in people with type 1 diabetes
An assessment of HbA1c levels is still included as part of the diabetes review for individuals with type 1 diabetes within the NICE (2022c) NG17 guideline. The guidance recommends that HbA1c be measured every 3–6 months in adults with type 1 diabetes (providing there are no circumstances that would render the test invalid – see Table 3). Adults with type 1 diabetes should be supported to aim for a target HbA1c level of ≤48 mmol/mol (6.5%), to minimise the risk of long-term vascular complications, although an individualised target should always be considered, with avoidance of problematic hypoglycaemia a priority.
However, an increasing number of people with type 1 diabetes are choosing to use continuous glucose monitoring devices and will use these (alongside capillary blood glucose measurements when needed) to monitor and self-manage their glucose levels. The three key glucose metrics used to do this are time in range (TIR), time below range and time above range (see Milne, 2023 for more information). There is a good correlation between HbA1c and percentage TIR, and on average a TIR of 70% corresponds to an HbA1c level of approximately 53 mmol/mol (7.0%) (Beck et al, 2019).
In the future, there may be a transition to using percentage TIR as the preferred metric for assessing glycaemic control and risk of diabetes complications (Vigersky and McMahon, 2019).
What can interfere with HbA1c and when to interpret tests with caution
Any condition that prolongs or shortens the lifespan of red blood cells, or reduces or increases their rate of regeneration, can affect how long the cells are exposed to glucose, resulting in increased or decreased HbA1c values. See Table 3 for a list of situations where HbA1c tests may be inaccurate.
HbA1c should be interpreted with caution in people with abnormal haemoglobin type, such as haemoglobinopathy, including sickle cell trait. Black people (including those with potentially undiagnosed sickle cell trait) may need further evaluation when considering an HbA1c test result, as the result may underestimate past glycaemia.
In pregnancy, red blood cell lifespan is reduced from around 120 to 90 days. HbA1c values reduce in the second trimester, plateau at 20–24 weeks and increase in the third trimester.
Interpretation of HbA1c should be approached with caution in older adults because the concentration of HbA1c increases as people age (Masuch et al, 2019). A few studies have explored the underlying mechanisms and suggested that a decreased red blood cell count caused by a reduction in cell turnover could lead to an increased red blood cell lifespan, thus increasing the levels of HbA1c (Wu et al, 2017). It has also been proposed that the cellular damage that occurs with aging, including altered enzyme activity, decreased membrane lipids and increased cell fragility, might accelerate glycation of haemoglobin and result in higher HbA1c levels (Rooney et al, 2021).
Official guidelines do not suggest using different reference values based on age for making the diagnosis of type 2 diabetes; however, it has been argued that definitions of prediabetes in older adults do not have the same prognostic meaning as they have in younger individuals (JN Learning, 2021). A more relaxed approach to target setting is advocated in most guidelines, including NICE, for older frailer individuals living with diabetes, as highlighted earlier.
Is there a correlation between average glucose and HbA1c?
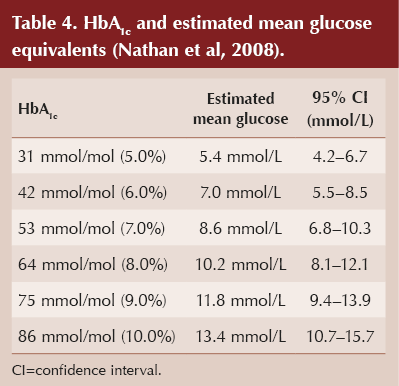
Individuals with diabetes sometimes share self-monitored capillary glucose readings that do not seem to correspond to their current HbA1c value (being either much higher or much lower than expected). Although a linear relationship between mean glucose and HbA1c levels across a range of glycaemia has been proposed (see Table 4), it is important to note that individuals with the same HbA1c value may have glucose concentrations across a broad range, and the estimated mean glucose ranges for various HbA1c levels overlap. This has important practical implications because, for example, a person recording a mean glucose level of 8.3 mmol/L could have an HbA1c anywhere between 42 and 64 mmol/mol, which would require different approaches to management.
Conclusion
Although HbA1c offers a number of practical advantages and has come to be regarded as the gold standard for both diagnosing and monitoring diabetes, it is important to recognise its limitations. It is not appropriate for diagnosing diabetes in certain clinical circumstances, and there are conditions that can give rise to falsely high or low results. In these situations, alternative methods of assessing glycaemia should be considered, including the measurement of fructosamine, self-monitoring of capillary glucose or, where appropriate, continuous glucose monitoring.
Additional information
LabTestsOnline (https://labtestsonline.org.uk/tests/hba1c-test) provides more detailed information, including how the HbA1c test is used, when it is requested and what the results mean, as well as answering other commonly asked questions about the HbA1c test.
As part of its series of Information Prescriptions, Diabetes UK has produced a single-page document explaining what HbA1c is, when a high HbA1c is a problem and how a person can lower their HbA1c. These can be personalised to include individual HbA1c target levels and goals, downloaded and saved into the person’s electronic medical record, and even shared via email or text. Information Prescriptions are available at: https://www.diabetes.org.uk/for-professionals/supporting-your-patients/information-prescriptions/information-prescriptions-qa





