Introduction
Diabetes and menopause are both cardiometabolic conditions. Low estrogen levels can affect insulin production and increase central adiposity, insulin resistance and the risk of developing type 2 diabetes.1,2
In women who are going through menopause, taking body-identical hormone replacement therapy (HRT) can reduce inflammatory markers, abdominal adiposity, insulin resistance and dyslipidaemia, and can reduce the incidence of new-onset type 2 diabetes.3 In women with pre-existing diabetes, HRT has been shown to improve fasting glucose, insulin resistance, mean blood pressure and LDL:HDL-cholesterol ratio.
When started early enough, the benefits of body-identical HRT are also widely considered to reduce the risk of heart disease, stroke, dementia, osteoporosis, colorectal cancer, and all-cause mortality.
Menopause classification
● The average age of menopause is around 51 years and is defined as twelve months after the last menstrual period.
● The perimenopause is the time leading up to this in which people may start experiencing symptoms and changes in their periods. It often occurs from 45 years of age but can be earlier.
● Menopause before 45 years of age is known as an early menopause.
● Before 40 years of age, it is often called premature ovarian insufficiency, which affects at least one in 100 women.
Symptoms of menopause
Many of the symptoms of menopause, hypo- and hyperglycaemia, and diabetic neuropathies overlap. It is, therefore, important for both the clinician and the individual to know what these symptoms are, how to identify them and what the treatment options are. For example, if a woman with diabetes is experiencing hot or cold sweats, the ability to test blood glucose levels at these times could identify whether the symptoms are due to hypoglycaemia or menopause, and whether they would be aided by a review of diabetes therapies or by HRT.
Menopausal symptoms have a negative effect on a person’s day-to-day life, and therefore their diabetes, as it is easier for people to make changes that can have a positive effect on health, such as making healthier food choices, increasing activity levels and optimising their medication and treatment, if they have a good night’s sleep and are not troubled by mental and physical health problems.
Symptoms of menopause include:
- Anxiety
- Low mood
- Fatigue
- Headaches/migraines
- Dizziness
- Sleep disturbance
- Body temperature changes
- Muscle aches, joint pains
- Cognitive changes
- Genitourinary problems
- Loss of libido
- Skin and hair changes
- Dry eyes
- Tinnitus
- Gastrointestinal changes
Benefits of using a menopause symptom questionnaire
The Menopause Symptom Questionnaire can be downloaded from here. Using this tool has the following benefits:
- Used to monitor symptoms over time, and thus response to treatment.
- Filled in prior to an appointment, which saves time during the consultation.
- Aids memory as often there are too many symptoms to remember.
- Acts as an ice-breaker for symptoms that may be difficult to bring up.
- Audit tool.
Hormones and HRT
Estrogen
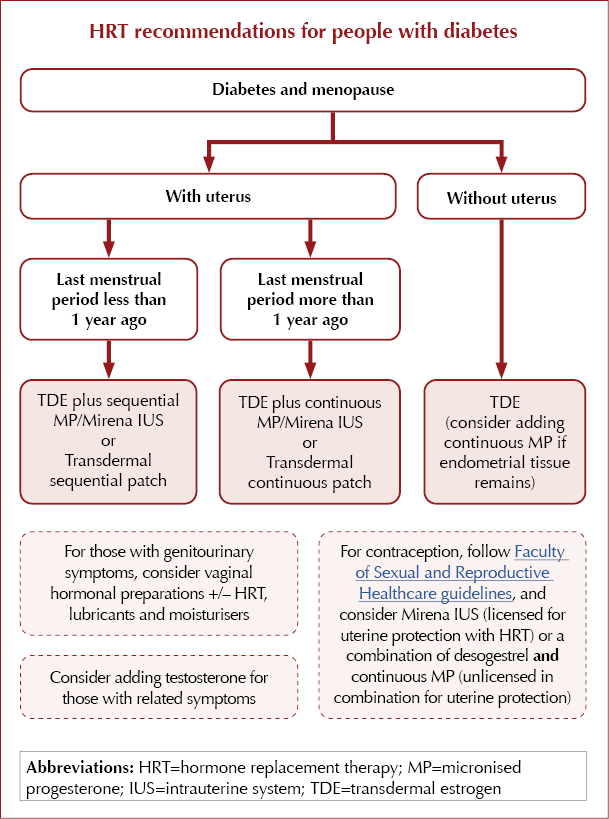
● Transdermal estrogen (TDE) does not carry an increased venous thromboembolism (VTE) risk.
● TDE comes in twice-weekly patches, daily gels or a spray.
● Giving TDE in a single preparation alongside oral or coil-delivered progesterone, rather than in a combination patch, enables easier dose titration.
Progesterone
● Low levels are associated with fertility and menstrual problems, anxiety, sleep disturbance, migraines and negative effects on bone health.
● Required when taking HRT for those with a uterus, as taking estrogen alone could cause endometrial hyperplasia.
● Considered in addition to estrogen if endometrial tissue remains following hysterectomy.
● Utrogestan, a plant-derived type of progestogen called “micronised progesterone” (MP), is identical in structure to the progesterone produced in by the human body and is often referred to as “body-identical”. It has not been shown to increase VTE risk or to carry the small increased risk of breast cancer associated with older synthetic progestogens.
● The Mirena coil is also not thought to confer an increased risk of VTE or breast cancer, and is licensed for contraception and the progesterone part of HRT.
Testosterone
● Plays an important role in muscle mass, bone strength, cardiovascular health, cognitive function, energy levels and mood, and can affect libido and sexual pleasure.
● Most research into the effects of low testosterone has been carried out in men. Low levels have been associated with an increased risk of type 2 diabetes, worse COVID-19 outcomes and chronic kidney disease, as well as effects on quality of life.
● The ovary makes around two to three times more testosterone than estrogen.
● Testosterone treatment is straightforward, with periodic blood tests and dose adjustment. Side effects are uncommon when levels are kept in the female range.
● Preparations available on the NHS (off-licence) for women include Testim, Testogel and Tostran, the latter of which is higher in strength. Androfeme is a plant-based cream dosed for women, and is currently available on private prescription.
A series of posters summarising the effects of these hormones in HRT, for healthcare professionals and patients, is available here.
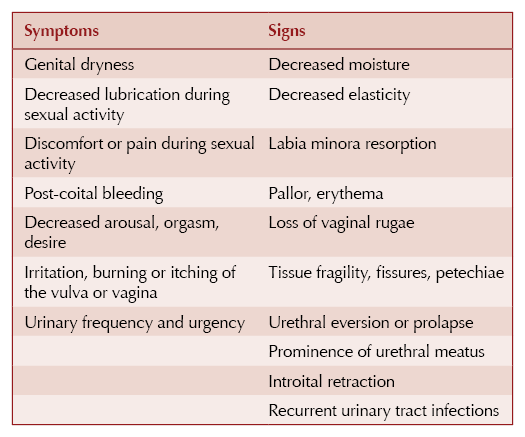
Genitourinary symptoms
● These are common in perimenopause and menopause.
● They are often associated with hyperglycaemia and neuropathic changes in those with diabetes.
● Genitourinary health is particularly relevant for women with diabetes, as they have an increased risk of genitourinary tract infections and bladder dysfunction.
● SGLT2 inhibitors used in the treatment of diabetes cause glucosuria. It is important to assess genitourinary health prior to starting SGLT2 inhibitors and during treatment, and to optimise HRT and vaginal estrogen as needed.
Genitourinary syndrome of the menopause (GSM)4
GSM is a comprehensive term that includes vulvovaginal and lower urinary tract symptoms related to low estrogen levels. Some women find HRT or vaginal hormonal treatments adequate for managing symptoms of GSM, but around 20% will require both treatment modalities.
Vaginal hormonal treatment
● Lowers vaginal pH, thickens endothelium, improves tissue blood flow, improves vaginal lubrication and maintains normal urogenital flora.
● May be given alone or alongside HRT.
● Comes in the form of pessaries, creams, gels and rings.
● The dose is very low and safe to be given with HRT.
● See the BSSM Position Statement for the Management of GSM for comprehensive advice on management.
Summary of messages
● HRT should be considered for all experiencing symptoms associated with the perimenopause and menopause.
● For most, HRT benefits outweigh risks.
● HRT has been shown to have cardiometabolic benefits.
● Transdermal estrogen does not carry an increased risk of VTE and can be considered for those with diabetes, hypertension, obesity and cardiovascular disease.
● HRT improves mental and physical wellbeing, which can lead to positive health changes.
● For those on diabetes medications that can cause hypoglycaemia, ensure access to blood glucose monitoring and reduce/adjust medication accordingly.
● The Menopause Symptom Questionnaire is a useful tool.
● Ask about genitourinary health and use vaginal hormonal therapy, alone or in conjunction with HRT, as needed.
● Those experiencing symptoms of low testosterone affecting quality of life should have a patient-centred approach to receiving testosterone treatment.
● HRT is cost-effective. Start it and see what happens to health, wellbeing and glycaemic control.





Daily oral GLP-1 receptor agonist in development results in significant weight loss but with no dosing requirements.
24 Sep 2025