The proactive management of people with long-term conditions, including the promotion of self-care, is a key priority for the NHS. Primary care has the central role in delivering integrated and personalised care and in implementing policies that target “at-risk” individuals (Goodwin et al, 2010). But at what cost? Long-term conditions management can be seen as a black hole for resources, staffing and energy. It can feel like the focus is just on “more for less” and innovation can be stifled in the race to control the bottom line. But are there opportunities available that have not been considered? Are there resources that might provide answers to some of the questions of how, when and where we improve diabetes care?
The Pharmacy Integration Fund was designed to support the transformation outlined in the Five Year Forward View (NHS England, 2014; 2016) and has been used to support the development of clinical pharmacy practice and drive the greater use of pharmacists and pharmacy technicians in new, integrated local care models. This has resulted in pharmacists becoming an important part of the general practice team and there being a greater focus on the clinical skills of community pharmacists. Pharmacists, however, are late to the game when it comes to being part of the diabetes multidisciplinary team (MDT). Nurses and doctors have achieved huge advances in care for this population of patients and are rightly recognised by both patients and professionals as the “go to” members of the team.
Pharmacists have traditionally worked in the background in a more supportive role, perhaps enabling or improving medication use and choices, or developing guidelines and policies. They are neither doctors nor nurses, but possess a range of skills that can complement the existing MDT – particularly regarding the management of complex medication regimens, alterations according to comorbidities, the licensing, supply and availability of medications, and de-prescribing. It is these skills in medicines optimisation that could perhaps now help with the sometimes overwhelming numbers of patients that we face.
Studies have shown that both GP practice and community pharmacists can provide benefit in the treatment and support of patients with type 2 diabetes (Ali et al, 2012; Langran et al, 2017). Community pharmacists are accessible whenever patients need them, without appointment at evenings and weekends – who better to support patients in lifestyle improvement and to answer questions about their condition or treatments? The NHS England Community Pharmacy Contractual Framework funds two services – Medicines Use Reviews (MUR) and the New Medicines Service (NMS) – that specifically aim to enable patients to improve self-care and to encourage them to take prescribed medication. Both MUR and NMS are advanced services that can be provided by any pharmacy that meets set criteria and undertakes simple training that is available to all. Approximately 90% of pharmacies in England currently offer the NMS (Pharmaceutical Services Negotiating Committee, 2018). Have you ever considered referring patients to these?
GP practice pharmacists are already working to improve prescribing habits and improve medicines safety. A recent study showed that GP pharmacists who reviewed the use of sulfonylureas in older adults with tight glycaemic control were able to stop use of the drug in 42% of patients and adjust doses in a further 17% (Diabetes Times, 2018). It is becoming common for these pharmacists to run clinics reviewing patients with diabetes – are you making the most of these skills?
There are, however, no formal training schemes to produce pharmacists with specialist diabetes skills and there are very few current specialist pharmacists available to train or mentor those that do express an interest. So how can we be confident that pharmacists, wherever they are based, know enough about diabetes to help both the MDT and patients?
The UK Clinical Pharmacy Association (UKCPA) Diabetes & Endocrinology Group has launched a competence framework to aid this development. Based on the nurse framework designed by TREND-UK, this document is designed to ensure parity between different professions and reduce variations in care. The Integrated Career and Competency Framework for Pharmacists in Diabetes (Diabetes UK, 2018) can be used to support a pharmacist career pathway that encompasses experiential learning and skills development, focusing on the individual pharmacist’s learning objectives and skills. The framework was supported and funded by UKCPA, and endorsed by Diabetes UK, TREND-UK and the Primary Care Diabetes Society.
The framework allows pharmacists delivering diabetes care to identify their current skills and knowledge, and develop a portfolio of practice. It also enables them to plan their careers in a more structured way and supports their continuing professional development by identifying individual development and training needs. This will allow pharmacists to develop alongside nurses and doctors as an integral part of the MDT and ensure that they are competent to take on the roles expected of them.
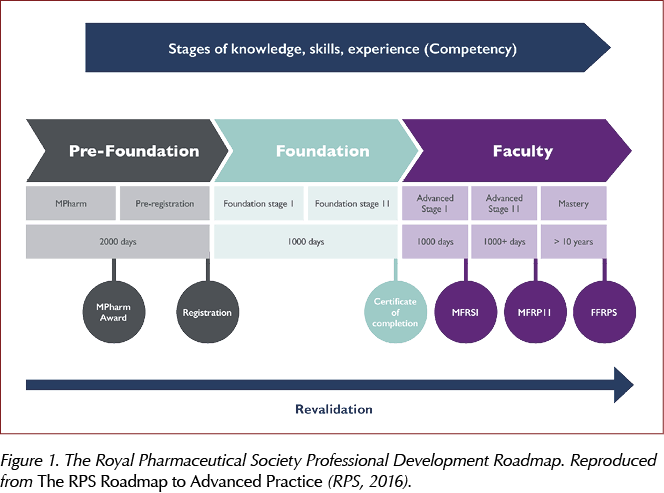
The clearly defined competency levels match the roadmap to advanced practice used by The Royal Pharmaceutical Society (RPS) to support career progression in pharmacy (Figure 1; RPS, 2016). The roadmap highlights the stages throughout a pharmacist’s career. However, when starting to specialise in a new discipline, regardless of years of practice as a pharmacist, it is logical to start at the beginning. Therefore, the first 1000 days of practice in diabetes shows foundation knowledge with an expected progression to higher levels of skills and knowledge over time as the speciality develops. This doesn’t detract from the pharmacist’s skills as a whole and, in fact, it would make sense that a more experienced practitioner would be able to specialise and develop faster owing to their previous practice and established skills.
There is opportunity for creativity and flexibility; it is not expected that all competencies will be met, even in highly specialised practice. Different sectors and individuals have different requirements and the framework allows each person to identify areas for their own practice. As a result, no matter where practice takes place, this can be used to show commissioners and colleagues alike what the pharmacist can offer to the team and the level of care they can deliver to people with diabetes. The framework is a tool, but perhaps it can open doors to get us all working together more efficiently, knowing that patients will receive great care, regardless of who they turn to for help.
Much like nurses and doctors starting out in their professions, to develop further, pharmacists will need support and encouragement to step out of traditional roles to become essential members of the MDT. This is more than achievable as a team. So I challenge you: How can a pharmacist help your service to meet the ever-increasing demands of diabetes management in primary care?





Quantifying the risk of worsening glycaemia, and how should healthcare professionals respond?
22 Apr 2024