Common risk factors for type 2 diabetes are also linked with the development of cardiovascular disease (CVD) (Leon and Maddox, 2015). Such factors include obesity, hyperlipidaemia and hypertension, with a clear correlation between diabetes progression and increased CVD risk (Grant and Cosentino, 2019). Chronic hyperglycaemia is also a precipitating factor for increased CVD risk (Leon and Maddox, 2015). With CVD being the cause of around 50% of deaths in people with concurrent type 2 diabetes, optimal glycaemic control is key (Einarson et al, 2018).
Many cardiovascular events resulting from CVD, such as myocardial infarction (MI) and stroke, could be prevented via methods of behaviour change (Office for Health Improvement & Disparities, 2022). General practice nurses (GPNs) are well placed to deliver such behaviour change interventions during everyday contacts. This article will explore the opportunities available to GPNs when delivering health-promotion strategies to reduce the overall risk of diabetes-related CVD.
Cardiovascular disease risk
NICE (2023a) recommends to assess cardiovascular risk using the QRISK® prediction model, which considers both modifiable and non-modifiable factors such as BMI, smoking status, blood pressure and medical history (Table 1).
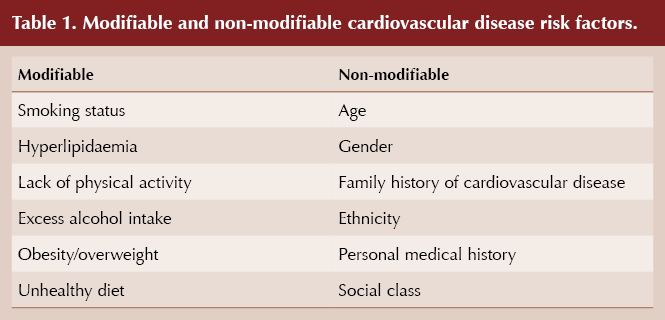
The third version of the QRISK model, QRISK3, has added several new CVD risk factors as variables, including corticosteroid usage, erectile dysfunction and migraine. These variables highlight opportunities for GPNs to implement preventative healthcare strategies in a variety of scenarios, such as contraception appointments, in which discussions around migraines are already best practice, and in diabetes reviews, where erectile dysfunction status should be determined and explored with male patients. Theoretically, these situations pose opportunities for the QRISK3 score to be calculated and discussed with appropriate counselling; however, time constraints are often a barrier (Keyworth et al, 2019), meaning subsequent follow-up appointments may be required.
It should be noted that CVD risk tools may underestimate risk in certain groups of people. It is, therefore, suggested that GPNs exercise clinical judgement in addition to using a system-generated score (Dueñas-espín et al, 2022).
Consideration of variables such as social determinants of health can also present GPNs with an opportunity to introduce preventative healthcare strategies, as socioeconomic deprivation is linked to increased levels of obesity (NICE, 2023c).
Making Every Contact Count
Public Health England (2016) developed the Making Every Contact Count (MECC) strategy to encourage the use of routine healthcare appointments to implement behaviour change interventions, with the aim of improving outcomes. MECC activities can be used by GPNs to promote health by focusing on behaviour change through brief interventions (BIs) or very brief interventions (VBIs), depending on the severity of the specific health need, such as smoking cessation or weight loss (Box 1).
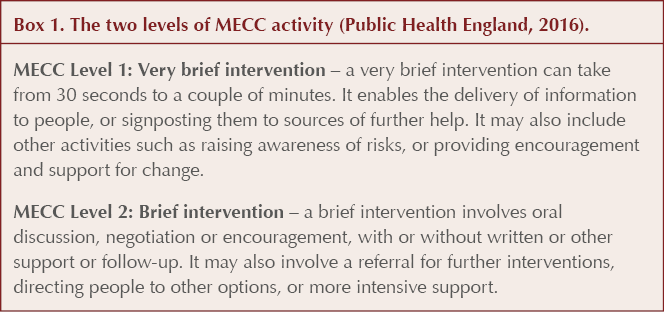
Aveyard et al (2012) suggest that BIs and VBIs can support small but cumulative changes in health behaviour to reduce CVD risk. However, it is thought that many GPNs lack the skills and/or confidence to support people with such interventions, which is a barrier to implementation of MECC (Lawrence et al, 2016). PHE (2016b) reiterates that MECC could potentially have a significant impact on population health and, consequently, should be prioritised when upskilling GPNs.
Whilst BIs and VBIs can facilitate positive discussions, Kessels (2003) suggests that people only retain around 50% of information from a medical consultation, and consequently patient decision aids are useful for the person to take home for future reference. However, it is essential that these should be supplementary to the discussion around options available, rather than replacing it (Scalia et al, 2021). The use of patient decision aids allows a GPN to improve a person’s knowledge of their health and to facilitate shared decision making, both of which are known to improve overall outcomes (Madsen and Fraser, 2015).
For fluidity and time efficiency, GPNs can prepare for appointments by printing a selection of patient decision aids and Diabetes UK Information Prescriptions, allowing non-internet-literate people equitable support in CVD risk reduction. In addition, Mills (2023) argues that advice alone is largely inadequate in facilitating behaviour change; therefore, it is essential that GPNs have a working knowledge of local services and offer immediate referrals.
NHS Health Checks
Obesity is well documented as a modifiable risk factor both for developing type 2 diabetes and for increased CVD risk. Similarly, weight gain in early adulthood is associated with increased risk of type 2 diabetes after midlife, suggesting that early intervention with diabetes prevention strategies would be beneficial to people at higher risk of type 2 diabetes (Sun et al, 2016). Ultimately, prevention of diabetes is key to reducing diabetes-related CVD risk, and GPNs are in a unique position to offer interventions intended to reduce such risks.
Currently, people at risk of developing type 2 diabetes can be identified during NHS Health Checks, developed to reduce national rates of heart disease, cerebrovascular events, type 2 diabetes and kidney disease (NICE, 2015). All UK residents aged 40–74 years who are registered with a GP and who have not already been diagnosed with one of these conditions are eligible for NHS Health Checks. However, despite the well documented benefits, including detection of risk factors such as hypertension and prediabetes, just 38.9% of eligible people attend for these checks (Tanner et al, 2022). GPNs are thus recommended to offer NHS Health Checks opportunistically during routine appointments to increase uptake and begin open conversations around CVD risk and the benefits of behaviour change.
Health Checks provide a unique opportunity to implement BIs or VBIs; however, these checks are often performed by unregistered healthcare professionals who may lack the confidence to instigate such strategies. Thus, in addition to GPNs, it is essential that training opportunities are offered to unregistered professionals such as healthcare assistants if they routinely perform NHS Health Checks. A simple training package in healthy conversation skills has been demonstrated to markedly increase use of person-centred skills which, in turn, support behaviour change (Lawrence et al, 2016). The relatively low cost of this training led to a disproportionately positive impact, which suggests a solution to the barrier of inadequate training.
National diabetes prevention programmes
To combat the increasing rate of type 2 diabetes diagnoses in the UK, NHS England designed a quality-assured intensive lifestyle-change programme for people diagnosed with non-diabetic hyperglycaemia (NDH). Although blood tests undertaken during NHS Health Checks identify a number of people eligible to attend the Healthier You NHS Diabetes Prevention Programme (Box 2), their success relies on attendance, which remains low.
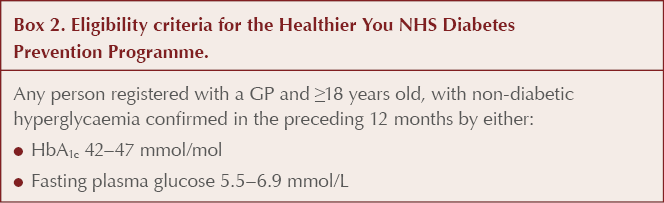
A systematic review of lifestyle-based diabetes prevention interventions demonstrated a 28% reduction in risk of progression from NDH to type 2 diabetes over a mean follow-up of 7.2 years, suggesting overall health benefits and reduction of associated CVD risk (Haw et al, 2017). However, a cost–utility analysis by Frempong et al (2022) confirmed that a large proportion of people referred to the Healthier You programme decline to attend, with the referral process identified as an influencing factor. Specifically, lack of communication of the risks associated with NDH and type 2 diabetes, and of the benefits of the programme, at referral was documented to affect uptake. Action by GPNs could negate these influencing factors by reviewing processes in practice to ensure that people diagnosed with NDH are counselled on the associated risks and the potential positive impact of attending a prevention programme.
Although some patients’ non-attendance is recorded as “declined”, not all of them may have actually done so. Qualitative data by Stokes et al (2019) found some people missed their initial Healthier You appointment in error or were simply unaware of being invited, with a 15% uptake when repeat invites were offered to those people who initially “declined” (Frempong et al, 2022). GPNs can influence attendance rates by facilitating searches to identify people who have not yet been invited or are recorded to have declined the prevention programme, then sending direct invitations via post, email or text message. Attendance to the programme should also be encouraged opportunistically by GPNs during routine consultations where preventative health VBIs or BIs are utilised.
Conclusion
Many interventions can reduce diabetes-related CVD through preventative healthcare strategies such as behaviour change interventions. Although GPNs are well placed to facilitate such interventions, the rates of success vary, with the main barriers to implementation identified as inadequate training and time constraints. A key finding from the literature is that adequate training in delivering interventions correlates directly with positive behaviour change (Lawrence et al 2016). This hypothesis extends to NHS Health Check appointments, which are often performed by untrained healthcare professionals who may lack the knowledge and/or confidence to broach behaviour-change topics using BIs or VBIs. Therefore, restructuring of staff responsibilities may be beneficial, with adequate training also proven to improve the quality of appointments.
The most effective approach to reducing diabetes-associated CVD is prevention of type 2 diabetes itself, with lifestyle-based prevention interventions resulting in a 28% reduction in risk of progression from NDH to type 2 diabetes (Haw et al, 2017). However, success relies on the at-risk individuals attending the programmes; therefore, GPNs have a role in encouraging attendance, either opportunistically or via targeted invitation (Frempong et al, 2022). Where prevention of type 2 diabetes is not possible, MECC can greatly improve clinical outcomes and, consequently, should be prioritised by GPNs.






Increased risk of new-onset heart failure in over-65s suggests caution is required before prescribing pregabalin for painful diabetic neuropathy.
14 Aug 2025