New drug options for obesity
All drugs were used in combination with diet (healthy or 500 calorie deficit diets) and physical activity support. None of these agents are licensed for use in the UK at this time.
Orforglipron, a small-molecule non-peptide GLP-1 receptor agonist (ATTAIN-1 study; Wharton et al, 2025a)
● Daily oral dosing with no food or drink restrictions.
● Mean placebo-subtracted weight loss at 72 weeks: 9.1% with 36 mg top dose.
● Subgroup assessed with DEXA:
- Pooled orforglipron group: mean 13.8% fat loss, 4.5% lean mass loss, 19% visceral fat mass loss.
- Placebo group: 1.7% fat loss, 0.3% lean mass loss, 7.4% visceral fat mass loss.
● See Diabetes Distilled for more information on ATTAIN-1.
● Orforglipron is also being studied for type 2 diabetes, cardiovascular disease reduction, osteoarthritis and obstructive sleep apnoea.
Oral semaglutide 25 mg (OASIS 4 study) and 50 mg (OASIS 1 study)
● Daily oral dosing on empty stomach, and no food, drink or other medications for at least 30 minutes.
● OASIS 4: 25 mg dose – mean placebo-subtracted weight loss 11.4% at 64 weeks and improved quality of life scores (Wharton et al, 2025).
● OASIS 1: 50 mg dose – mean placebo-subtracted weight loss 12.7% at 68 weeks (Knop et al, 2023).
Subcutaneous semaglutide 7.2 mg (STEP UP trial; Wharton et al, 2025b)
● Once weekly subcutaneous injection, stepped up from 2.4 mg to 7.2 mg, without intermediate dose.
● 7.2 mg superior to placebo: 18.7% mean weight loss vs 3.9% with placebo over 72 weeks.
● 7.2 mg also superior to 2.4 mg:
- Mean extra 3.1% weight loss.
- More likely to achieve higher weight loss (i.e. 15%, 20% and 25%).
- More likely to achieve remission from prediabetes (post hoc findings, therefore exploratory only).
● Adverse events:
- Stepping up from 2.4 mg to 7.2 mg dosing produced minimal increases in gastrointestinal side effects.
- High rates of dysaesthesia (described as tingling, burning or itching), occurring in 22%, 6% and 0.5% with 7.2 mg, 2.4 mg and placebo, respectively.
- Serious adverse effect rates with 7.2 mg similar to placebo and lower than with the 2.4 mg dose.
- In an accompanying comment, Sattar and Lean (2025) remind that different people will require and tolerate different doses of incretin drugs, so it will be important to individualise drug choice when these are licensed.
● STEP UP T2D study in people with obesity and type 2 diabetes:
- 7.2 mg semaglutide superior to placebo: 9.3% placebo-subtracted mean weight loss (as expected, lesser weight reductions in type 2 diabetes compared with obesity alone).
- Greater reductions in waist circumference and HbA1c with 7.2 mg than with 2.4 mg.
- Safety and tolerability comparable between the two doses, apart from increased rates of dysaesthesia.
● Cardiovascular benefits have previously been demonstrated with semaglutide 2.4 mg (Badve et al, 2025), but it is not yet clear whether the higher dose will offer increased benefits.
Cagrilintide 2.4 mg once weekly – efficacy and safety sub-analysis of REDEFINE 1
● Cagrilintide is a long-acting analogue of amylin, a satiety hormone involved in food intake, body weight and glycaemia, which affects appetite regulation and, therefore, offers a different mechanism for weight loss from the GLP-1 RA drugs.
● As monotherapy in the REDEFINE 1 study (Garvey et al, 2025), cagrilintide 2.4 mg achieved a mean placebo-adjusted weight loss of 9.5% at 68 weeks.
- 31.6% of recipients achieved weight loss of at least 15%, compared to just under 5% with placebo.
● Cagrilintide was well tolerated, with mild to moderate gastrointestinal side effects (usually temporary) most common.
- Gastrointestinal effects led to drug discontinuation in 1.3% of cagrilintide recipients, compared to 0.6% with placebo.
● Cagrilintide will be further explored in the RENEW study programme.
EASD launches diabetes distress clinical practice guideline
The EASD launched the draft of its first evidence-based clinical practice guideline at the Annual Meeting, focusing on the assessment and management of diabetes distress among adults with diabetes. Led by Professors Jane Speight and Richard Holt, the guideline development panel included people with lived experience of diabetes from the outset.
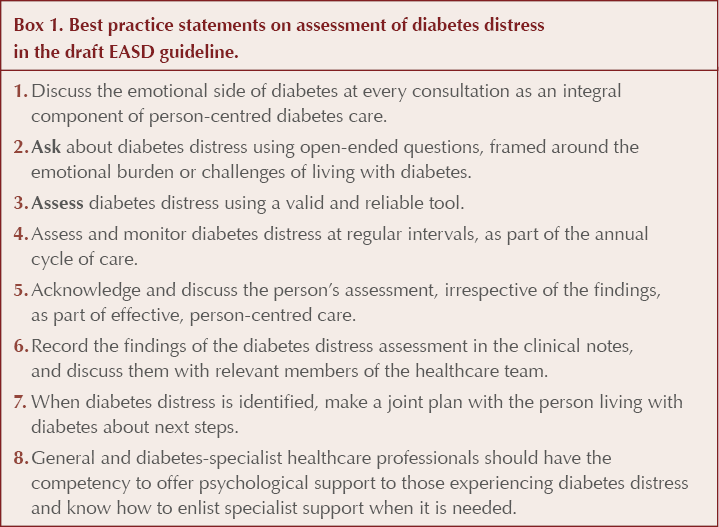
● Key recommendations include a series of eight best practice statements on assessment of diabetes distress (Box 1), followed by nine recommendations each for the management of diabetes distress in people with type 1 and type 2 diabetes, using psychological and psychoeducational interventions.
● Successful implementation of the guideline will require training, system-level support and integration into routine care.
● The guideline is out for consultation until 31 October 2025, with a view to publication in early 2026. The draft can be viewed here.
Obesity drug discontinuation rates are high
A population-wide study of new users of semaglutide for weight loss in Denmark, presented by Professor Reimer Thomsen (Aarhus University, Denmark), demonstrated that more than half discontinued therapy within 1 year.
● 18%, 31% and 42% stopped treatment within 3, 6 and 9 months, respectively.
● Age influenced discontinuation rates, with users aged 18–29 years more likely to stop within 12 months than those aged 45–59 years.
● Cost appeared to contribute – people living in low-income areas were 14% more likely to discontinue in the first year than those in high-income areas.
● Those with a history of gastrointestinal medicine use (who may thus have been more likely to have gastrointestinal side effects) and those with a history of psychiatric medication use were 9% and 12%, respectively, more likely to discontinue semaglutide within the first year than those without.
Reduced “food noise” with semaglutide 2.4 mg – INFORM survey
● Food noise is defined as a constant, obsessive and intrusive stream of food-related thoughts, separate from feelings of hunger, and has been reported by 57% of people living with overweight or obesity (WeightWatchers and STOP Obesity Alliance, 2024).
● A US survey of 550 people treated with semaglutide 2.4 mg for weight loss, using a validated food noise questionnaire, demonstrated a significant drop in food noise, from 62% to 16%, while taking high-dose semaglutide and other incretin drugs for weight loss.
● Previous research has also demonstrated reduced cravings for smoking and alcohol whilst taking semaglutide (Hendershot et al, 2025).
Tirzepatide for type 2 diabetes in children – SURPASS-PEDS trial
● In the Phase 3 SURPASS-PEDS trial, 99 children aged 10–17 years with type 2 diabetes were randomised to receive tirzepatide 5 mg or 10 mg or placebo.
● At week 30, mean HbA1c was reduced by 24 mmol/mol (2.23%) in the pooled tirzepatide groups versus an increase of 0.5 mmol/mol in the placebo group (P<0.001 for comparison). This efficacy was sustained up to 1 year of follow-up.
- 79% of tirzepatide recipients achieved an HbA1c <48 mmol/mol (6.5%).
● Mean BMI fell by 9.3 kg/m2 in the pooled tirzepatide groups, compared to a reduction of 0.4 kg/m2 in the placebo group.
● As with adult users, the commonest adverse effects were gastrointestinal symptoms.
● The study was simultaneously published in The Lancet.
Cannabis use quadruples risk of developing type 2 diabetes
● Electronic health records from 54 healthcare organisations across the US and Europe were used to compare almost 100,000 people with cannabis-related diagnoses (ranging from occasional use to dependence) with over 4 million matched controls.
● Over 5 years of follow-up, 2.2% of the cannabis group, but only 0.6% of controls, developed type 2 diabetes. Possible mechanisms could be increased insulin resistance and unhealthy dietary behaviours.
● The study is limited by its retrospective nature, inaccuracies associated with patient reporting of cannabis use and the imprecise measurement of cannabis exposure.
Type 2 diabetes doubles risk of sepsis
● In this long-term community-based study in Australia, among 1430 adults with type 2 diabetes and 5720 matched controls, over a mean follow-up of 10 years, 11.8% of the diabetes group developed sepsis, compared with 5.0% of controls.
● They were also twice as likely to have had a prior hospitalisation for sepsis at study enrolment.
● Those with early-onset type 2 diabetes were at particularly high risk, with those aged 41–50 years having a 14.5-fold increased risk of sepsis after adjustment for potential confounders.
● Potential mechanisms include elevated blood glucose leading to impaired immune function, higher infection risk in people with diabetes overall, and vascular damage and neuropathy leading to increased risk.





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025