Going to university and leaving home for the first time can be daunting for any young person. For someone with type 1 diabetes it’s even more of a challenge. JDRF has collaborated with Diabetes UK and NHS England to create the University Toolkit, providing students with all the information they need about looking after type 1 diabetes at university. The creation of the tool has been supported by research work by Dr Swe Myint and her team at Norfolk and Norwich University Hospital.
Identifying a clear need for support
A number of worrying problems experienced by young people attending university were identified by a national survey, overseen by Dr Myint, which was sent to 1865 current UK university students aged 18–24 years with type 1 diabetes. A total of 584 (31%) students from 64 hospitals and 37 university medical practices completed the questionnaire, which found that:
- 62% of students had kept routine diabetes care with their home team, whereas 32% had moved to the university provider
- Since starting university, 63% of respondents reported that their diabetes management was harder, and 44% reported higher HbA1c levels than before university
- At university, 52% had frequent hypoglycaemia, 9.6% reported one or more episodes of severe hypoglycaemia, and 26% had experienced diabetes-related hospital admissions
- Female students and those who changed healthcare provider were approximately twice as likely to report poor glycaemic control, emergency hospital admissions and frequent hypoglycaemia
- Females were more likely than males to report stress [odds ratio (OR) 4.78, 95% confidence interval (CI) 3.19–7.16], illness (OR 3.48, 95% CI 2.06-5.87) and weight management issues (OR 3.19, 95% CI 1.99-5.11) as barriers to self-care
- Despite these difficulties, 91% of respondents never or rarely contacted university support services about their diabetes.
These results made it clear that a comprehensive toolkit was needed to support young people with type 1 diabetes at university.
A collaborative opportunity
JDRF started developing the University Toolkit back in 2016 and became aware, through local engagement at a transition conference, that Dr Myint was working with Diabetes UK to offer a resource for the type 1 community focused on university. As soon as JDRF became aware that the NHS team and Diabetes UK were working together on a resource, they arranged a meeting in Norwich to discuss collaborating. JDRF wanted to ensure that resources were not duplicated, efforts and budgets spent efficiently, and that the final resource was as thorough and beneficial as possible to those affected by type 1. Working collaboratively on this was the best way of achieving this.
The original JDRF toolkit was mostly led by volunteers. Emma Cartwright, a patient with type 1 diabetes, supported the collaborative throughout the process. “When I decided to apply to university I had no idea where to start in preparing my diabetes for the move,” she said. “Moving to a new city, where I knew no one was scary enough without the added stress of changing consultants, registering for a GP and working out how to get a prescription. There were so many things to think about and I knew that there were probably so many things I was going to forget. A toolkit like this would have made my move to university so much easier. Just being able to see a list of all of the things I had to consider and knowing that I could always refer back to it would have been a great comfort in effectively managing my diabetes.”
The University Toolkit has been developed with input from students, graduates, parents, healthcare professionals and JDRF, Diabetes UK and NHS England staff and volunteers.
“Over 500 university students with type 1 diabetes have provided information on their experience of diabetes care at universities,” Dr Myint said of the research. “The University Toolkit is a true reflection of their experiences and a successful collaboration between healthcare professionals and leading charities.”
Anecdotal feedback has been positive throughout testing and checking, with diabetes specialist nurses saying: “This looks excellent. At the moment we do not have a pack like this, instead we have to provide separate forms and literature.” and that it is full of “User friendly, easy to access, clear messages. I have disseminated this email amongst my diabetes colleagues and will be sure to signpost this resource to all of my type 1 diabetes students.”
A user-friendly resource
The key message the collaborative wants to get across to those using the online resource is that type 1 diabetes is not an obstacle to university life. It has therefore focused on making the toolkit as user friendly as possible. From user feedback and focus groups, the collaborative learned that students wanted information electronically that is easy to access via the internet on various platforms (browser, tablet, phone etc). The toolkit has been built to be compatible with all formats and offers downloadable PDFs of each content section.
The tabbed layout of the home page, similar to an iPhone home screen, makes accessing relevant information quick and easy. There is also a smart search function that allows users to type in key words, which searches the toolkit content and titles.
Helping young people access assistance
There are a number of things you can do to help young people prepare for the move to university:
- Ask patients if they are planning to study away from home. If they are, offer to complete the professional transfer letter template – which is within the downloads section of the toolkit – with them. Suggest they make copies or photograph and email it to themselves using their phone in case the original version is mislaid
- Advise patients to find and register with a local GP practice/university health centre as soon as possible after arrival
- Discuss the pros and cons of staying with their current specialist diabetes team or changing to a hospital close to university
- Ensure they have been prescribed sufficient supplies before starting university and suggest they speak to accommodation or student services at their university to arrange to have a mini-fridge in their room for insulin storage
- Provide them with a medical exemption card and copies of old prescriptions
- Recommending getting a medical tag if they are not already wearing one
- Tell them about the University Toolkit. They can order promotional flyers of the toolkit here
Before starting
Young people can inform universities that they need additional support at the application stage. There is a box on the UCAS form that asks whether applicants have a disability. Although many young people with type 1 diabetes do not consider themselves to have a ‘disability’ or be ‘disabled’, this is the umbrella term used by universities which includes medical conditions like type 1 diabetes. You should point this out and advise young people to tick this box to let the university know that they have a medical condition that may require support. This may make things easier once they start and the university should automatically send further information support that is available. If they do not or have not ticked the box on the UCAS form, advise patients that they can notify the student support office before they start university or make an appointment to see them once they have started. They may also want to contact the university halls or accommodation and student support services before the start of their first term. The toolkit provides information on what to do before starting university, so it is worth sign-posting young people to this topic.
Other aspects to explore
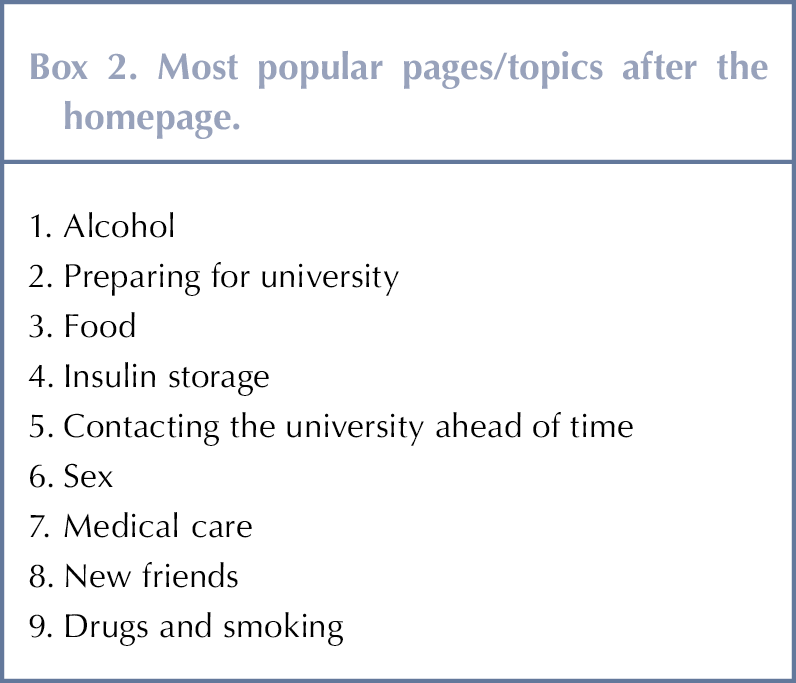
You may also want to let young people know that there are resources on smoking, drinking, drugs and sex that they might find useful. Young people may find it difficult to discuss such things with healthcare professionals, whether or not they intend to go to university, so it is worth raising awareness of the toolkit as a reliable and accurate source of information. Anecdotally, these topics have proven popular with a range of adults with type 1 diabetes.
There are also topics covering accessing GP and specialist care, which is useful in ensuring continuity of care, plus emotional wellbeing, studying abroad and managing sick days. Downloadable guides are available for friends and flatmates.
Initial feedback and numbers
To date the collaborative has received brilliant feedback from healthcare teams, who are using the University Toolkit beyond its initial remit. As it covers topics around lifestyle, it is proving useful to adult audiences with type 1 diabetes. This may be reflected in the current user demographics: the biggest audience is the 25–34 age group, followed closely by the target audience (people aged 18–24). Uptake is slightly higher in men than women. This is encouraging as a men are less likely than women to visit their GPs (Wang et al, 2013).
With your assistance, the collaborative hopes to increase traffic to the toolkit over time by reaching out to more young people and helping them better manage their type 1 diabetes.





NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022