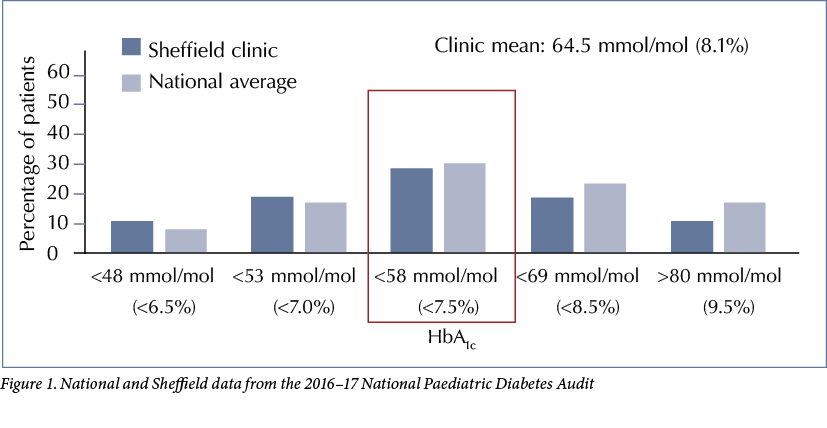
The Sheffield Children’s Diabetes Team looks after approximately 240 patients with type 1 diabetes aged 0–17 years. Historically the team has always performed well in terms of measured outcomes. In the 2014–15 National Paediatric Diabetes Audit (NPDA) data we ranked in the top five units in the country, with a mean HbA1c of <65 mmol/mol (<8.1%). In subsequent years our ranking slipped, however, with increased mean HbA1c levels and fewer patients achieving HbA1c <58 mmol/mol (<7.5%). Our 2016–17 results were slightly above the national average but the mean HbA1c had increased to 64.5 mmol/mol, see Figure 1.
As a result of this downward trend, we applied to participate in the Royal College of Paediatrics and Child Health’s Diabetes Quality Improvement (QI) pilot project. Our successful application afforded us the opportunity to address our relatively poor outcomes using QI methodology. It also gave us the impetus and drive to implement the changes necessary to benefit our service users, and early data are encouraging.
QI aim
Our aim was to empower, encourage and educate young people with diabetes – and their families – to confidently manage their diabetes to live happy, healthy and successful lives and to achieve a target HbA1c of 48 mmol/mol (6.5%) at 3 and 12 months post diagnosis.
Identifying areas to improve
The recognition that excellent control in the first year after diagnosis leads to better long-term outcomes was the impetus for change. The Diabetes QI pilot project introduced us to QI methodology, which acted as a vehicle for change. Over two weekends and two separate weekdays the whole team – including the administrator, nurses, dieticians, psychologist and doctors – explored QI techniques to help drive and sustain change. We identified a particular need to change our current ways of managing and providing education for newly-diagnosed patients in order to reduce the proportion of patients with poor control in the 12 months following diagnosis.
In order to identify areas on which to focus our QI work, we looked at various patient/family surveys that had previously been undertaken and identified a number of areas to take forward. Our knowledge survey revealed patient and carer confusion in areas central to excellent diabetes control, such as blood glucose targets, quality of and access to out-of-hours advice, and sick day rules. We therefore identified a need to provide our patients and their families with individualised, bespoke education to enable and empower them to manage their diabetes effectively.
Initiatives implemented
The QI methodology empowered us to identify relatively small projects to implement sequentially and to ‘be brave and fail fast’. Each initiative is led by a subgroup from within the team, with input from all team members.
QI initiatives started to be implemented from the end of 2017. Patients are recruited prospectively from diagnosis. The initiatives implemented to date are:
- Carbohydrate counting from diagnosis: Dietitians developed the carb counting resources, which utilise food labels and pictorial resources. They also led on up-skilling the inpatient ward staff. All 48 members of the ward nursing team and ancillary staff have now been trained to support inpatients and their families with carb counting in the absence of diabetes team staff. When in the community, telephone advice is available from one of the diabetes consultants 24 hours a day, 365 days of the year. This initiative was launched on 7 December 2017.
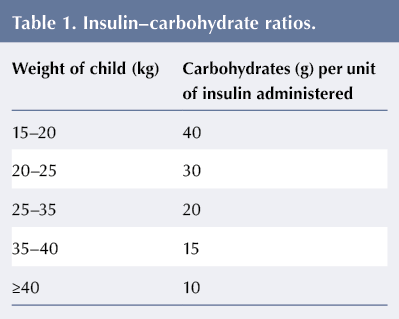
Historically our practice has been to keep admission after diagnosis with type 1 diabetes to a minimum (if at all). Patients are now initially kept in for carb counting training, which starts at their first meal after admission to the ward. No fixed insulin doses are used at all. Insulin–carbohydrate ratios are calculated based on the weight of the patient rather than his/her age, see Table 1. Blood glucose is measured before the meal. If >8.0 mmol/L, a corrective dose of insulin is required in addition to that needed for carbohydrate intake. Corrective insulin doses for various blood glucose levels are given on a weight-specific chart, eg the chart for children weighing 15–20 kg. Patients are given a total dose of rapid-acting insulin 15 minutes before eating.
- Micro-teaching in the clinic: A list of 25 topics has been developed based on feedback from the patient survey. Examples of topics covered include:
– Treating hypoglycaemic events
– Insulin before meals
– Exercise
– Broken pumps
– Sick day rules
– Periods
– Ramadan (materials are available in English and Arabic)
– Alcohol consumption.
We present a bite-sized teaching topic chosen by the patient and his or her family; discussion is facilitated in the waiting area before each clinic appointment by a member of the team (a ‘diabetes educator’). - Agreed team targets: Targets have been set to ensure that we all give exactly the same advice and to eliminate inconsistency, eg blood glucose levels before and after meals and at bedtime, etc.
- diasend® downloading at home from diagnosis: We encourage families to take an active role in interpreting their own data, thereby enhancing self-management skills. While the child or young person is an inpatient, he/she or his/her family is provided with a cable and advice on how to download and interpret information. This initiative has been implemented with the aim of providing a springboard for our next project: telephone clinics.
The progress of each of these projects is continually monitored with selected metrics displayed on run charts and discussed fortnightly at our QI breakfast-meetings. To maintain a tight focus on blood glucose control, our run charts monitor average blood glucose at 7 and 30 days after diagnosis and HbA1c at 3, 6 and 12 months post-diagnosis. Ongoing analysis of our data so far suggests that average blood glucose at 30 days is the best predictor of HbA1c at 12 months. This has allowed the Children’s Diabetes Team to target those not achieving good control at 1 month by offering additional support and exploration of perceived barriers to good control.
Impact to date
In Year 1, 34 CYP with newly-diagnosed type 1 diabetes benefited from the new initiatives. So far in Year 2, we have included 17 newly-diagnosed patients. All metrics collected in relation to our patients are reviewed at the regular biweekly QI meetings and any trends and outliers are identified, discussed and – where necessary – investigated.
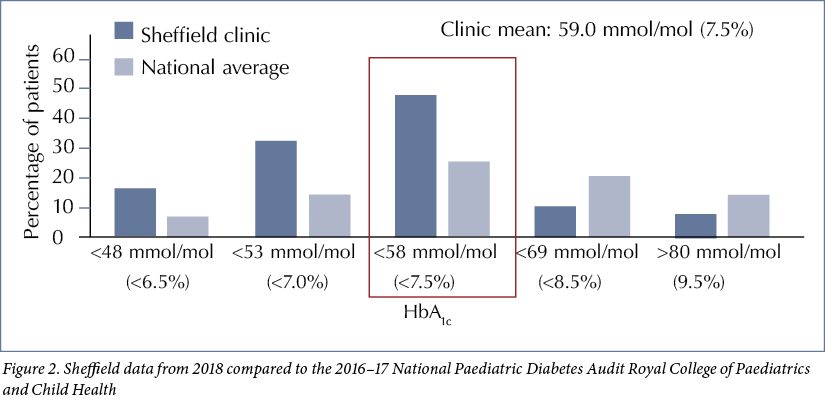
While the initial focus of our QI journey was on our newly-diagnosed patients, the impact on the control of these patients and the ripple effect of agreed targets and microteaching on our entire clinic population has been significant. Recent HbA1c data suggest that 52% of all our patients now achieve HbA1c <58 mmol/mol compared to the nadir of 28.6% in 2016–17, see Figure 1, and our clinic mean HbA1c has fallen from 64.5 mmol/mol (8.1%) to 59.0 mmol/mol (7.5%), see Figure 2. This is a significant improvement in mean HbA1c compared to NDPA audit data from previous years, which served as control data.
We have kept our entire clinic population abreast of our QI work by means of regular newsletters and updates on social media. Social media has given us immediate responses, and the feedback from families has been extremely positive. In the clinic, a token voting system has been implemented to elicit additional feedback. A question is posed to all clinic attendees, eg ‘What is your experience of micro-teaching in the waiting area?’ or ‘What are your experiences of diasend downloading at home?’, and the question is changed every few weeks. Responses are collated and discussed at QI meetings. Through these measures, regular feedback is informing us about how initiatives are being received by patients and their families.
The ward staff members have been extremely enthusiastic in facilitating the implementation of carb counting at diagnosis and Accu-Chek Aviva Expert blood glucose meters are issued to all patients/families so they can track blood sugar levels. Those patients and their families experiencing any difficulties with carb counting receive as many extra sessions as required with a dietician. The number of meals that are carb counted with a member of the diabetes team before a newly-diagnosed patient is discharged is recorded to monitor levels of support and education patients and their families have received.
Input from the ward staff members is invaluable. By working with them as part of the extended team we have learned to ‘be brave and fail fast’, so that good ideas can be tried and if necessary modified, helping to fuel and maintain enthusiasm for planned change. Any difficulties in implementing or maintaining any of the initiatives are discussed as a team, solutions are sought and changes to approach made – which is exactly what QI methodology is all about. The hospital management team has been supportive of our QI work, which we have shared widely via our communications team both internally, within the trust, and externally within the paediatric diabetes community and beyond. However, perhaps the biggest immediate impact has been on the way the members of the Children’s Diabetes Team works together for our patients. The QI initiatives have been hard work but have pulled an already high-achieving team closer together in striving for a common aim for our patients and have resulted in changes in the ways we work. There has been no investment in personnel to expand the team and there is no doubt that individuals within the team are working harder than ever with more frequent face-to-face contact with patients in clinic and at home.
Looking to the future
In the future, we plan to make a number of further changes to enhance the services we provide. We intend to expand the list of micro-teaching topics available. We also plan to instigate diasend downloading at home for all – not just newly-diagnosed – patients at least every 2 weeks. Patients and their families will receive feedback based on downloaded data from a member of the diabetes team via email or telephone. In preparation for this, we are offering planned drop-in sessions at the Children’s Diabetes Team administration base and during some clinics to facilitate home downloading and to offer the opportunity to download between clinic appointments if patients and their families do not have the necessary technology at home or in school. Depending on the uptake and effectiveness of this project, more formal telephone clinics may be initiated.
The current limiting factor for change is manpower. Without expansion of the team, priority will have to be given to the interventions that seem most effective based on metrics and feedback from patients and their families.
Summary
Our QI work is being constantly evaluated through the collection of agreed metrics for all our newly-diagnosed patients. The ‘ripple effect’ within our total clinic population will be evidenced by NPDA data in perpetuity. Early indicators are that our outcomes are already improving for all of our patients.




NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022