It is thought that 10–12% of type 1 diabetes (T1D) patients have first-degree relatives – parents, offspring or siblings – with T1D (Haller et al, 2005). The recent ISPAD guidelines put familial aggregation at about 10% and acknowledge a variation in incidence between countries, within countries and between differing ethnic populations (Mayer-Davis et al, 2018). While previous studies (Lorenzen et al, 1994; EuroDiab Ace Study group, 1998; Lebenthal et al, 2010) have looked at demographic data on parents, children and offspring with T1D, there are few clinical data on parental diabetes management following a child’s diagnosis.
When researching the literature, the authors were unable to find any previous studies looking at parental clinical data, such as clinic attendance and HbA1c levels, over the period following T1D diagnosis in their offspring. It was therefore decided:
- To examine parental engagement with the adult diabetes team following T1D diagnosis in their offspring
- To see whether parental HbA1c levels improved in the 2 years following diagnosis in their offspring
- To examine whether the offspring of parents with T1D had a lower HbA1c at diagnosis and in the following 2 years than a control group
- To compare rate of diabetic ketoacidosis (DKA) at diagnosis and episodes of severe hypoglycaemia in dyad offspring and a control group.
Methodology
This was a quantitative retrospective review of all children and parents with T1D attending Cork University Hospital (CUH). Patients were identified from records kept in the Children’s Diabetes Unit from 2009 to March 2018. These data were cross-referenced using CUH’s electronic hospital in-patient enquiry system. This provided a list of all children diagnosed with diabetes aged 0–17 years over the same time period. Forty-two parent–offspring pairs and 30 sibling pairs were identified. Among the parent–offspring group:
- Three families had a parent and two offspring affected by T1D
- One family had two affected parents and one offspring
- One family had three affected siblings
- One pair of monozygotic twins was identified.
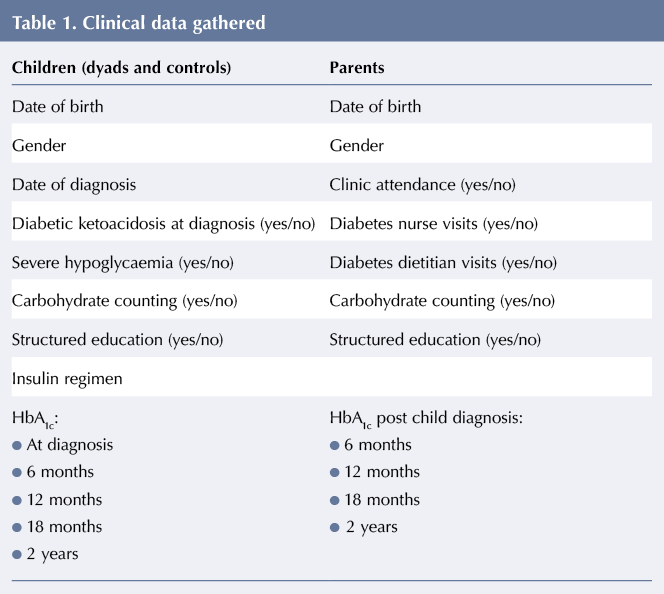
Dyads were included if a parent and child had T1D; both received diabetes care at CUH; and the child had T1D duration of at least 2 years, see Figure 1. For each child in the eligible dyads, the next age- and gender-matched child with newly-diagnosed T1D was assigned as a control. Clinical data, see Table 1, were extracted for the groups.
CUH defines DKA using the British Society for Paediatric Endocrinology and Diabetes criteria of pH <7.3 or bicarbonate <18 mmol/L with evidence of ketonaemia (blood ketones >3 mmol/L) or hyperglycaemia (>11 mmol/L) (Edge, 2015). Episodes of severe hypoglycaemia are defined using the International Society for Pediatric Endocrinology and Diabetes consensus guideline as a hypoglycaemic event associated with a loss of consciousness or seizure (Abraham et al, 2018; previously Ly et al, 2014). HbA1c levels in both children and adults are measured using a Tosoh G8 Analyser (Tessenderlo, Belgium) following the principles of cation-exchange high-performance liquid chromatography.
Parents were contacted in person, by phone and/or by email. They were given an information leaflet explaining the nature of the study and asked to complete a questionnaire. The questionnaire was designed to obtain information about parental characteristics, personal and familial history of diabetes, and engagement with diabetes services before and after their offspring were diagnosed. It consisted of 29 questions with yes/no answers or a list of options to pick from and parents were asked to tick the answers as appropriate. Informed consent was obtained from parents to access both their and their child’s medical records. The study was approved by the Clinical Research Ethics Committee at Cork Hospitals Group.
Statistical analysis
Data were collected and analysed using Microsoft Excel and SPSS version 22. Two sample t-tests and Pearson’s chi-squared test were used. A P-value of <0.05 was considered statistically significant.
Results
Three-hundred-and-seventy children and young people (CYP) with T1D (aged 1–17 years) attend CUH. All CYP diagnosed at CUH are started on multiple daily injections and educated on carbohydrate counting from diagnosis. Those attending from other centres are provided with carbohydrate counting education when they attend CUH.
CYP are offered structured education, in the form of the CHOICE programme, 6 months after diagnosis. The programme consists of 3-hour sessions provided over a 4-week period and aims to give CYP and their families or carers the skills and knowledge they need to manage their diabetes and reduce the impact of the condition on daily activities and lifestyle. There is an uptake rate of 70%.
Of the 370 CYP attending CUH, 161 (43%) were on continuous subcutaneous insulin infusion; to access this, CYP have to be carbohydrate counting and attend the CHOICE programme. CYP are seen in the outpatient clinic every 4–5 months and have their HbA1c measured at each clinic visit. The mean HbA1c was 64 mmol/mol (8%) in 2017.
During the course of this study, 61 (16.4%) CYP attending the clinic had a first-degree relative with T1D: 31 had a parent and 30 had a sibling with the condition. Only parent–child dyads were studied.
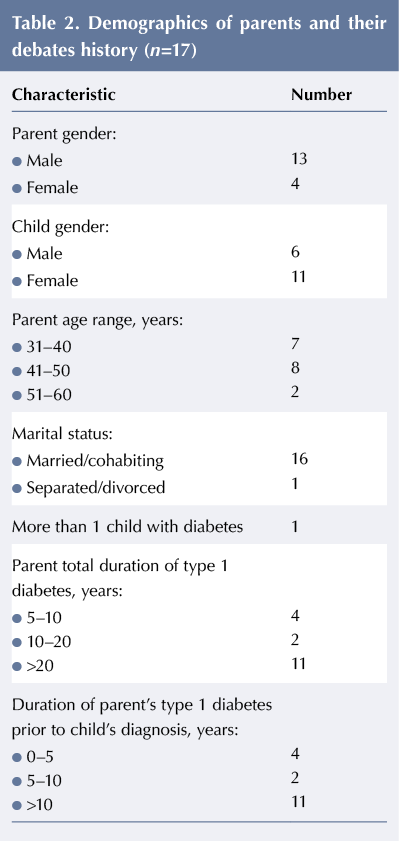
Demographic data and family history
Of the 28 parents in eligible dyads treated at CUH, 17 (13 male and four female; mean age 43.6 years) participated in this study, see Table 2. Eight parents in the dyads had a further first-degree relative affected by the condition: three had a parent, four a sibling and one a second child with T1D. Eleven parents were diagnosed >10 years prior to their child and two after their child. Eleven (64%) of the offspring were female. All participants came from a white European background.
The characteristics of the children in the dyad and control groups are given in Table 3. There was no difference in mean age at diagnosis; however, the mean HbA1c was lower in the dyad group.
Clinic attendance
At the time parents completed the survey, six (35.2%) were not attending any diabetes service: two of these individuals were waiting to be seen by the adult diabetes service, having decided to re-engage following their child’s diagnosis; a third individual, who was diagnosed after their child, had initially engaged with the service but had not attended any follow-up appointments. Of the 11 parents that do attend the diabetes service, five were seen at least twice per year and six are were seen annually during the study period. Thirteen of the parents had not seen a diabetes nurse and/or diabetes dietitian since 2009.
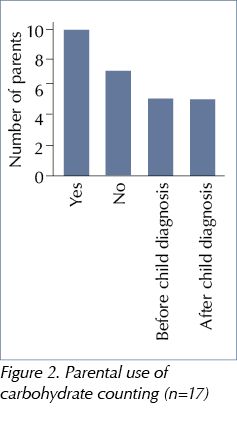
Carbohydrate counting and structured education
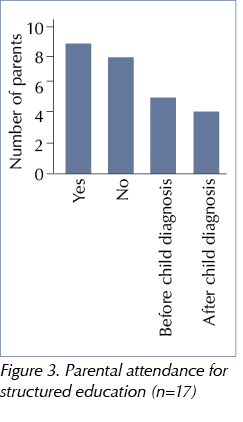
The questionnaire revealed that 10 parents were carbohydrate counting for their own T1D management, five of whom had started after their offspring received their diagnosis (including one parent diagnosed after his child), see Figure 2. Nine had completed a diabetes structured education programme, with four attending the Berger programme offered by adult services following their child’s diagnosis, see Figure 3.
Twenty-six children in the dyad group were carbohydrate counting compared to 24 children in the control group. Twelve of the dyad group and 15 of the control group had attended a structured education course.
HbA1c
Thirteen parents were on multiple daily injections and four were on continuous subcutaneous insulin infusion. No statistically significant changes were seen in parental HbA1c levels in the 2 years following T1D diagnosis in their offspring, see Figure 4. No HbA1c measurement had been recorded for four patients following their diagnosis; however, two of these parents had been diagnosed after their child. The majority of parents (10) only measured their HbA1c levels annually, which may explain the low number that had their HbA1c measured at 6-monthly intervals.
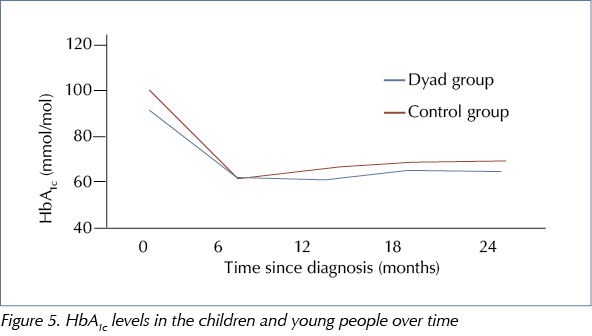
The mean HbA1c level in children at diagnosis was non-significantly lower in the dyad group, see Table 3. In the 2 years following diagnosis, the two groups of children had similar HbA1c levels, see Figure 5.
DKA and severe hypoglycaemia
Fourteen (50%) children in the control group presented in DKA at diagnosis compared to seven (25%) in the dyad group (P=0.053).
In the 2 years post diagnosis, there were three episodes of severe hypoglycaemia in children in the dyad group and four in the control group. This difference was not significant.
Discussion
The rate of T1D among first-degree relatives, at 16.4%, is higher than in previous studies. Roche et al (2005) and Metcalfe and Baum (1992) gave rates of between 8% and 10% in participants from the same geographic region as the current study (the UK and Ireland). An Israeli study including Ashkenazi Jews (48.5%), non-Ashkenazi Jews (44.3%) and Muslim Arabs (7.2%) found a total familial prevalence of 9% (parent–off spring 4% and sibling pairs 5%) (Lebenthal et al, 2010). No specific reason was found for the high numbers of first-degree relatives with T1D attending CUH. One theory is that the increased prevalence among first-degree relatives may correlate with the increased incidence of new T1D patients diagnosed at CUH over the past decade: 28 cases in 2007 versus 51 in 2017.
The male preponderance among parents and female preponderance among offspring corresponds with results from previous studies showing that T1D is two to three times more common in the offspring of men than women (Gale and Gillespie, 2001). In a review of the literature, Gale and Gillespie (2001) found children of fathers with T1D were more likely to develop T1D than those with mothers with T1D and that fathers are more likely to transmit diabetes to their daughters.
Currently, six of the 17 parents are not attending any diabetes service. Five of these had previously attended the service but seem to have been ‘lost’ in their young adult years due to missed appointments. In an audit of their practice, Casey et al (2014) found that young adults missed on average three out of seven appointments offered over a 24-month period. A similar study by Mahmood et al (2010) showed that 15% of young adults only attended one in every three appointments. The sixth patient not attending any service was diagnosed at CUH but had not attended any follow-up appointments at the time of this study. In CUH, only eight (48%) of the parents had attended an appointment in the 2 years prior to this study. Only four parents had seen an adult diabetes nurse or dietitian since 2009. The adult service offers the opportunity to see a diabetes nurse or dietitian between consultant clinic appointments, and uptake is disappointing. The reasons for poor engagement among adults may be multifaceted, owing to the different characteristics of this group. Presently, there is no joint paediatric–adult transition service in CUH. This can lead to poorer outcomes, as the lack of continuity in care may lead to increased non-attendance and in patients becoming ‘lost’ to services (NICE, 2016). The provision of a transition service is a priority, though its implementation will be challenging as it requires input from all multidisciplinary team members and may involve changes to the structure of the existing service. The present clinic model may not be suitable for all adults due to education/work, family and other life commitments. Furthermore, the interval between appointments at CUH is currently 9–14 months. This finding is not unique, as diabetes care for adults in Ireland can be unstructured and ad hoc, with only 42% of services currently offering adults with TID the recommended 6-monthly reviews (Department of Health, 2018).
The increase in the number of parents who commenced carbohydrate counting and attended structured education for their own diabetes following their child’s diagnosis is a positive finding. Presently all newly-diagnosed adults are added to a waiting list for structured education, but due to a deficit in resources the waiting period is 18–24 months, with attendance rates varying between 50% and 70%. Among the parents in this study, nine (52%) have attended a structured education course – four after their child was diagnosed with diabetes.
Parental mean HbA1c was 65 mmol/mol (8.1%) in the 2 years after the diagnosis of their offspring. CUH does not have a database for adults with T1D, therefore no comparison was able to be made with the general T1D population. However, this HbA1c compares favourably with the average 81 mmol/mol (9.6%) measured in young adults with T1D (18–25 years) over a 24-month period (Casey et al, 2014) and is similar to the 67.5 mmol/mol (8.3%) reported for patients aged 30–60 years with T1D by the 2016 Scottish Diabetes Survey (Scottish Diabetes Survey Monitoring Group, 2017). The percentage of adults not having their HbA1c recorded in the current study (11%) was similar to the Scottish Diabetes Survey (just under 10%).
The lower HbA1c levels at diagnosis in CYP who had a parent with diabetes may be due to the earlier recognition of diabetes; questionnaire responses indicated that the majority of parents in the dyads felt that they recognised their child’s symptoms. Despite this, both the dyad and control groups saw similar improvements in HbA1c in the 2 years post diagnosis and, when compared to the general paediatric T1D patient population, the HbA1c levels were broadly similar. A mean of 64 mmol/mol (8%) was observed in 2017.
Of concern is the fact that seven (25%) children in the dyad group presented in DKA at diagnosis. This rate is lower than the control group, and one reason for this may be earlier recognition of the symptoms among parents and carers. However, five out of the 17 parents with T1D did not recognise their child’s symptoms. Over a 6-year period, 38% of all newly-diagnosed patients presented at CUH in DKA. The presence of DKA results in a longer average hospital stay of 6.5 days compared to 3.5 days in newly-diagnosed T1D patients without DKA (Finn et al, 2019).
The rate of severe hypoglycaemia was low in both groups. The increased use of technology such as sensor-augmented pumps, continuous glucose monitoring and flash glucose monitoring have helped to reduce the number of CYP presenting with severe hypoglycaemia.
Although 16 out of 17 parents responded that the education provided to their children improved their own diabetes care, no improvements were seen in parental clinic attendance or HbA1c levels. The present challenges resulting from increased intervals between adult diabetes clinic appointments leads to difficulties in ascertaining whether having a child with T1D makes any difference to these factors. There is no local or national register that can be used to compare outcomes. The development of a register to obtain accurate data is a priority and a national diabetes register for the Republic of Ireland is currently in consideration.
This study had a high response rate among parents (60%) and is one of the first to consider parental outcomes in familial diabetes. It looked at parent–child T1D dyads in just one centre, was retrospective and had a small sample size. Further investigations looking at larger populations across multiple centres should therefore be carried out. A mixed methods approach could be undertaken looking at qualitative as well as quantitative issues, such as family burden and parental emotional distress. When considering emotional distress and family burden, it would be useful to determine whether parents prioritised their children’s diabetes management over their own diabetes self-management. Future research should analyse HbA1c levels over a longer period of time and rates of DKA in the years post diagnosis.
Conclusion
The diagnosis of T1D in a child did not result in improvements in parental clinic attendance or HbA1c levels but was associated with a perceived improvement in self-management. Aside from the lower rate of DKA at diagnosis, having a parent with T1D was not found to be advantageous to children with regards to diabetes management.








NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022