The National Paediatric Diabetes Audit (NPDA) has demonstrated improvement in care and outcomes associated with paediatric diabetes care in England and Wales since 2010. However, variation at paediatric diabetes unit (PDU) level and between different patient groups persists. Future audit publications, including spotlight audit reports, will aim to elucidate the causes of variation. The National Children and Young People’s Diabetes Quality Network will support continuing improvement.
The NPDA is funded by NHS England and the Welsh Government, commissioned by the Healthcare Quality Improvement Partnership (HQIP) and delivered by a team at the Royal College of Paediatrics and Child Health (RCPCH). It was established in 2003 and has achieved participation from 100% of PDUs in England and Wales since 2012. The 2017–18 audit (RCPCH, 2019a) collected data from all visits to PDUs in England and Wales between 1 April 2017 and 31 March 2018. It included data pertaining to 29,752 children and young people (CYP) with diabetes, of whom 95.1% had type 1 diabetes, 2.5% had type 2 diabetes and the remainder had other rare forms of the condition.
The dataset (RCPCH, 2017) is designed to stimulate national improvements in the completion rate of health checks as recommended by the National Institute for Health and Care Excellence (NICE, 2015) for the diagnosis and management of CYP with type 1 and type 2 diabetes, and in diabetes management as indicated by glycated haemoglobin (HbA1c). Each PDU submits data from each visit to its service over the audit year via the secure NPDA data capture system. Results are published at national, regional, local health board/clinical commissioning group, and sustainability and transformation partnership level (RCPCH, 2019b; 2019c).
Key findings
Key health checks for diabetes
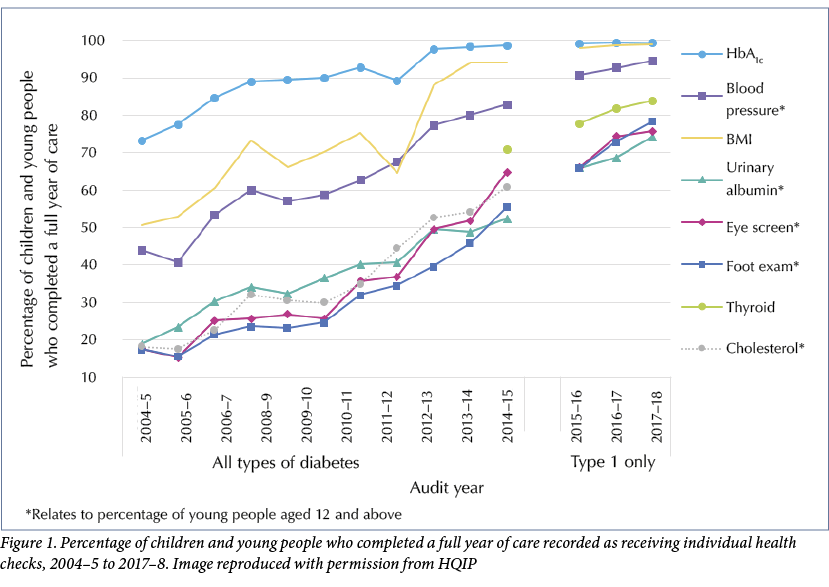
The 2017–18 audit showed continuing improvement in the completion rates of the seven key health checks for children and young people with type 1 diabetes, see Figure 1. Despite these improvements, less than half (49.8%) of CYP with type 1 diabetes and just over a quarter (25.7%) of CYP with type 2 diabetes aged 12 years and above received all seven key health checks within the audit year. However, at PDU level the percentages of those completing all seven checks ranged from 0% to nearly 100%; evidencing a need for targeted local efforts to improve performance.
Outcomes
HbA1c
Although the median HbA1c for all CYP with diabetes in England and Wales in 2017–18 has remained stable at 64 mmol/mol (8%) compared to 2016–17, this still represents a marked improvement over several years from a level of 72 mmol/mol (8.7%) in 2010–11, see Figure 2. Drivers for change include the development of a National Network, Best Practice Tariff in England and enhanced Health Board funding in Wales, quality assurance through peer review, and diabetes delivery plans.
The sharing of good practice among PDUs has led to less variation in clinical care, yet
there remain trends towards higher HbA1c among girls, adolescent young people, those of non-White ethnicity and in those living in more deprived areas. Multiple regression modelling evidenced the significant impact of each of these factors independently of one another. However, even after case-mix adjustment using such modelling there remains significant variability in HbA1c outcomes across PDUs, see Figure 3.
Diabetes-related complications
Albuminuria was found in 10.2% of young people aged 12 years and above with type 1 diabetes, and its prevalence was higher among those living in the most deprived areas. The percentage of albuminuria among those with type 2 diabetes was twice as high, at 22.1%, evidencing the highly aggressive nature of type 2 diabetes in the young.
Abnormal retinopathy screening was found in 12.8% of young people aged 12 and above with type 1 diabetes, although the prevalence fell between 2016–17 and 2017–18 from 14.8% to 12.8%. The risk of retinopathy among those with type 1 diabetes increased with age, was highest among adolescent females, and was slightly higher among those living in more deprived areas. Abnormal eye screening results were found in 5.6% of young people with type 2 diabetes; less than half the rate recorded among young people with type 1 diabetes.
Care at diagnosis
NICE guidance recommends providing carbohydrate counting and screening for coeliac and thyroid diseases at the time of diagnosis of type 1 diabetes (NICE, 2015). Four out of five CYP newly diagnosed with type 1 diabetes were screened for coeliac disease (80.2%) and thyroid disease (83.8%); an improvement from 79.8% and 72.6%, respectively, in 2016–17. Two-thirds (67.6%) of CYP are now receiving level 3 carbohydrate counting training at diagnosis.
Use of diabetes-related technologies
The use of pumps as a mode of insulin delivery in type 1 diabetes has increased over the past 4 years, with a reciprocal reduction in multiple dose injections, see Figure 4. Although insulin pump usage has increased, the gap between those living in the most and least deprived areas has widened in recent years, from 18.4% versus 26.3% respectively (a difference of 7.9 percentage points) in 2014–15 to 29.0% versus 41.1% in 2017–18 (a difference of 12.1 percentage points), as shown in Figure 4.
Usage of insulin pump therapy was associated with lower HbA1c compared to multiple daily injections. However, there were significant associations for increased insulin pump usage with younger age, female sex, White ethnicity, and living in less deprived areas; groups that are already associated with better HbA1c outcomes.
Use of a continuous glucose monitor with alarms was also associated with lower HbA1c. Similar to insulin pump usage, continuous glucose monitor usage was also associated with younger age, living in the least deprived areas and White ethnicity.
Conclusion
The 2017–18 NPDA has evidenced continuing improvements in diabetes care, including increases in the provision of recommended health checks (RCPCH, 2019a). The reduction in HbA1c between 2012 and 2018 has been impressive but more work needs to be done to continue this downward trend and reach the levels of diabetes control recorded in some other European countries (Charalampopoulos et al, 2018). NICE (2015) has set a ‘gold standard’ target HbA1c of <48 mmol/mol (<6.5%) in order to reduce the lifetime risk of micro- and macrovascular complications England and Wales; but with fewer than one in 10 (7.2%) CYP with type 1 diabetes achieving this in 2017–8, there is a long way to go. Furthermore, the variability in outcomes by PDU and in certain vulnerable groups remains an area open for quality improvement initiatives.
Next steps
The NPDA is publishing national and PDU-level spotlight audit reports in Autumn 2019 that will elucidate variation in the paediatric diabetes workforce and in support for the use of diabetes-related technologies between services. These reports will focus on:
- The workforce and structures within PDUs
- Diabetes-related technologies
- Parent and patient experience measures
- Research into the experiences of CYP with type 2 diabetes
Other upcoming publications include local and national reports on the data collected from 13,184 CYP and their parents who completed our 2019 patient and parent reported experience measure surveys, which aim to provide PDUs with feedback on potential areas for improvement and areas of achievement.
The audit will also be conducting engagement work with CYP with type 2 diabetes in conjunction with Diabetes UK in order to understand this group’s experience of their condition and their care.
Over 90% of all PDUs have signed up to the National Children and Young People’s Diabetes Quality Programme since 2017–18. Initial findings are showing that participation has a positive impact (Peng et al, 2018), which will hopefully be evidenced in the 2018–19 NPDA.
The NPDA has already developed a real-time data submission platform so that PDUs can submit at any time during the audit year and receive back an instant online progress report outlining their data quality and completeness (RCPCH, 2018). We would encourage use of this tool throughout the year to help review progress and impact of any quality improvement initiatives.








NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022