Type 1 diabetes is a serious chronic condition that can cause microvascular and macrovascular complications. People with diabetes who are able to maintain glycaemic control are able to reduce the incidence of complications, comorbidities and death (Herman et al, 2018). Education following diagnosis is important to help individuals understand how to manage their diabetes, which promotes good glycaemic control (Hopkins et al, 2012). Our study was to see whether increasing the frequency of initial follow-up after the diagnosis of type 1 diabetes improves the long-term glycaemic control, from 3 months until 4 years after diagnosis.
Background
Current NICE (2016) guidance recommends that children and young people (CYP) with type 1 diabetes, and their family or carers, should have education from diagnosis. Education topics should include insulin therapy; blood glucose monitoring; effects of diet, exercise and intercurrent illness; and detecting and managing hypoglycaemia and hyperglycaemia. There is no current NICE standard for frequency of initial follow-up, although ongoing follow-up is expected to occur four times per year (NICE, 2016).
NICE (2016) recommends an HbA1c target of ≤48 mmol/mol (6.5%) to minimise the risk of long-term complications. This was adjusted in 2015 from the previous NICE guidance (2004), which recommended aiming to achieve an HbA1c ≤58 mmol/mol (7.5%; Dalton et al, 2015). The National Paediatric Diabetes Audit (NPDA, 2018–19) showed approximately only one in ten CYP with type 1 diabetes manage to achieve a target of ≤48 mmol/mol. The present study also looks at CYP achieving a HbA1c of ≤58 mmol/mol, recognising that, while not ideal, there is still evidence that this helps to reduce long-term complications when compared with a higher HbA1c (Nathan et al, 2014).
In Gloucestershire, standard practice prior to November 2013 included hospital admission for education at diagnosis, carbohydrate counting from diagnosis and use of an expert meter. There was no standard for frequency of initial follow-up. The diabetes multidisciplinary team (MDT) in Gloucestershire wanted to improve initial follow-up as there was a desire to improve education and enable better self-management. Aggressive management of hyperglycaemia early in diagnosis is thought to be important for long-term control, also referred to as the “metabolic memory” effect (Testa et al, 2017). Furthermore, the team wanted to standardise care for all people with diabetes following diagnosis.
Aims
Our aim was to see if increasing the frequency of initial contact with CYP who have been newly diagnosed with type 1 diabetes increases the number of individuals who achieve the suggested target HbA1c of ≤48 mmol/mol or ≤58 mmol/mol at 3 months, 6 months, 12 months, 2 years and 4 years.
Methods
This was a retrospective study analysing HbA1c levels following an increase in the initial contact received following diagnosis. This research consists solely of retrospective analysis of routinely collected, anonymised data following a change in clinical practice. Therefore, ethics committee approval was not necessary.
The intervention starting in November 2013 was for CYP with newly diagnosed type 1 diabetes to have four or more contacts in the first 60 days. This 60-day period started after hospital discharge, following their initial diagnosis. The type of contact included was face-to-face time with a consultant, nurse or dietitian in clinic, at home or in a ward setting.
Thirty-two CYP were selected chronologically prior to the intervention, from 9th May 2012 to 2nd November 2013, and labelled as the “historical group”. Thirty-two CYP were then selected after the intervention date, between 8th November 2013 and 13th January 2015, and labelled as the “intervention group”. CYP were excluded if they were transferred into or out of the Trust in the first four years following diagnosis. They were also excluded if they were in the historical group and had received four or more contacts in the first 60 days, or if they were in the intervention group and had received fewer than four contacts in the first 60 days. There were no other clinical or service changes in this time period. All CYP were younger than 16 years of age at diagnosis.
The types of contact excluded were psychologist appointments, hospital admission for illness (not education), nurse visits to the school or nursery, telephone calls and the initial inpatient stay. A diabetes database was used to collect information. Data were compiled in a Microsoft Excel spreadsheet and were anonymised.
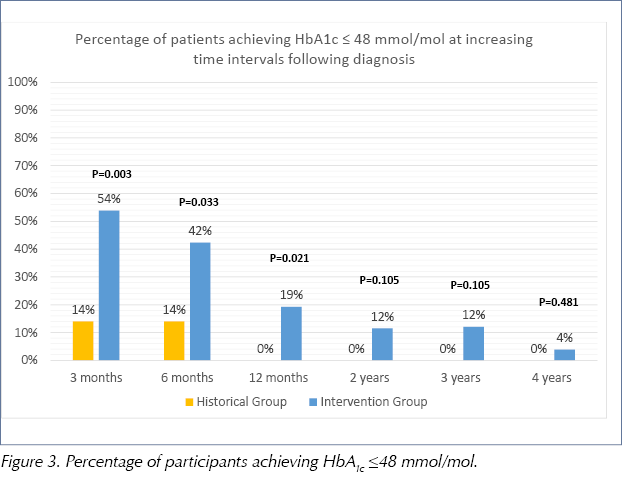
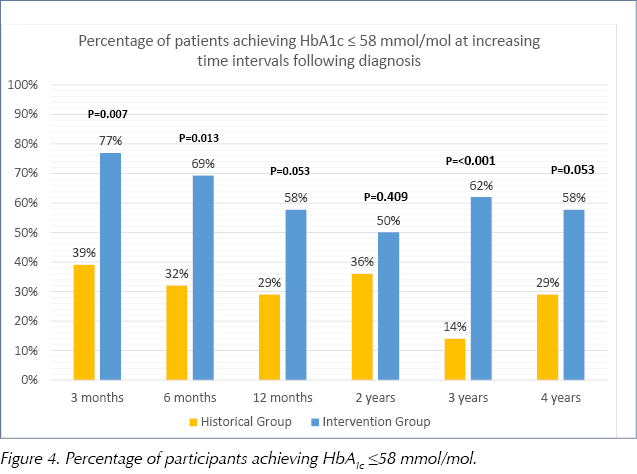
HbA1c levels were taken at routine clinic follow-up at 3 months, 6 months, 12 months, 2 years, 3 years and 4 years following diagnosis. The percentage of CYP who achieved HbA1c levels of ≤48 mmol/mol, and also ≤58 mmol/mol, at these time points were plotted on a bar chart. P-values were calculated using Fisher’s exact test.
Results
A total of 64 CYP were analysed between 9th May 2012 and 13th January 2015. Ten CYP were excluded; two CYP were transferred into or out of the Trust, four were in the historical group and had received four or more contacts in the first 60 days, and four were in the intervention group and had received fewer than four contacts in the first 60 days. This left 28 CYP in the historical group and 26 CYP in the intervention group. Both groups had similar baseline demographics, which are shown in Table 1.
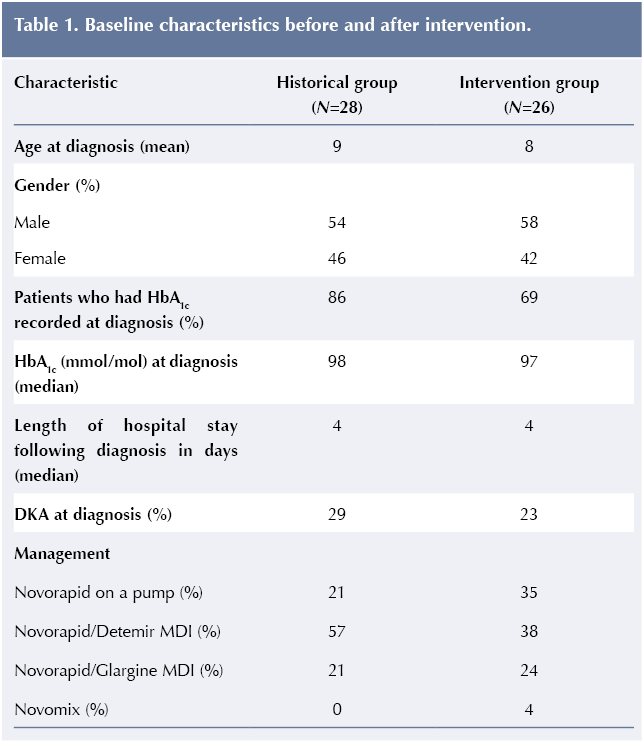
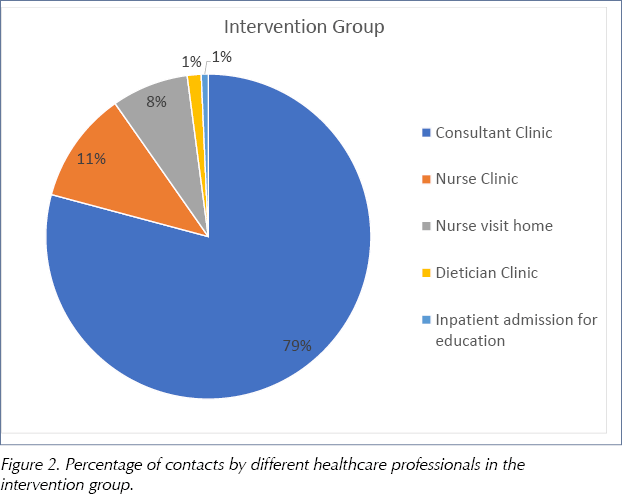
In the historical group, CYP had a mean of two contacts with a consultant, nurse or dietitian in the first 60 days. In the intervention group, they had a mean of five contacts. In the historical group, all CYP were seen at least once by a consultant. Ten (36%) of the CYP saw a consultant twice. In the intervention group, all CYP saw a consultant at least three times, with 11 (42%) seeing a consultant four times. In the intervention group, 79% of contacts were with consultants compared with 59% of contacts in the historical group (Figure 1 and Figure 2).
The number of CYP achieving an HbA1c of ≤48 mmol/mol was higher at all time points in the intervention group compared with the historical group. At 3 months following diagnosis, 54% of CYP in the intervention group achieved an HbA1c ≤48 mmol/mol compared with 14% in the historical group (P=0.003). At 6 months, 42% of CYP in the intervention group had achieved an HbA1c ≤48 mmol/mol compared with 14% in the historical group (P=0.033). In the intervention group, 19% achieved an HbA1c ≤48 mmol/mol at 12 months (P=0.021), 12% at 2 years (P=0.105), 12% at 3 years (P=0.105) and 4% at 4 years (P=0.481) following diagnosis. At 12 months, 2 years and 4 years, no CYP in the historical group achieved an HbA1c ≤48 mmol/mol (Figure 3).
The number of CYP achieving an HbA1c of ≤58 mmol/mol was higher at all time points in the intervention group compared with the historical group. At 3 months following diagnosis, 77% of individuals in the intervention group achieved an HbA1c ≤58 mmol/mol compared with 39% in the historical group (P=0.007). At 6 months, 69% of CYP in the intervention group had achieved an HbA1c ≤58 mmol/mol compared with 32% in the historical group (P=0.013). A higher percentage in the intervention group achieved an HbA1c ≤58 mmol/mol at 12 months (P=0.053), 2 years (P=0.409), 3 years (P<0.001) and 4 years (P=0.053) following diagnosis (Figure 4).
Discussion
These results show a statistically significant increase in CYP achieving HbA1c levels of ≤48 mmol/mol in the intervention group at 3, 6 and 12 months, compared with the historical group. There was also a statistically significant increase in CYP achieving HbA1c levels of ≤58 mmol/mol in the intervention group at 3 and 6 months. Following the intervention, the number of contacts received by CYP in the first 60 days increased on average from two to five appointments. The majority of appointments were made by consultants in both groups and the proportion of consultant appointments increased in the intervention group. It is not known whether increasing the contact with nurses or dietitians would have the same effect, and further investigation is needed.
When feedback was sought from the diabetes MDT, it was observed that knowledge levels were improved and this improvement was achieved at a faster rate than had previously been seen. It was also observed that CYP were more confident in self-managing their condition sooner.
Both the historical and intervention groups had similar baseline characteristics in terms of age, initial inpatient stay, gender, initial HbA1c and occurrence of diabetic ketoacidosis (DKA) at diagnosis. This helps minimise bias affecting the results. Unfortunately, some CYP did not have a HbA1c recorded at diagnosis. This may have been due to lack of understanding of the importance of an initial HbA1c within the admitting teams. The unavailability of these data may skew results as, if the missing HbA1c data were high, we may not know if some CYP were more unwell at diagnosis.
Unfortunately, we were not able to include data on socioeconomic status as it is not routine to ask families their income or occupation. However, there was no reason to believe that there was a difference between the historical and intervention group.
There was slight variance in insulin usage between the two groups, with three more children (14% more) using insulin pump therapy in the intervention group, compared with the historical group. While the NPDA data (NPDA, 2020) suggest a trend that CYP who use insulin pump therapy achieve lower HbA1c targets versus those who use multiple daily injections (MDI), the data do not account for confounding variables. The SCIPI trial (Blair et al, 2019) also shows no clinical benefit in outcomes in the first year after diagnosis when comparing insulin pump therapy with an MDI regimen. Actual numbers for variance within this study are low and we do not feel this impacts the overall strength of the intervention results.
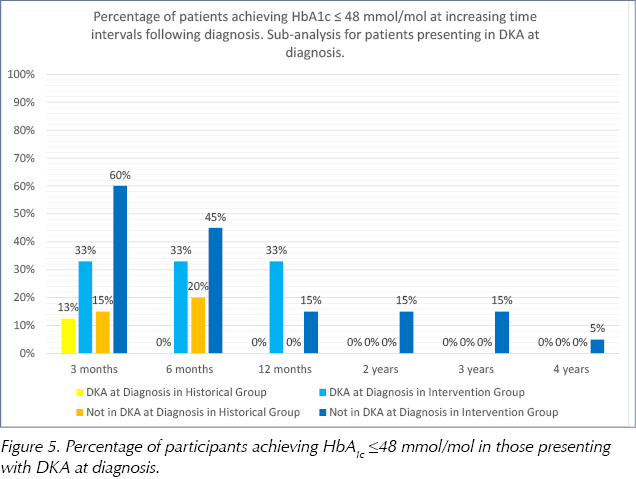
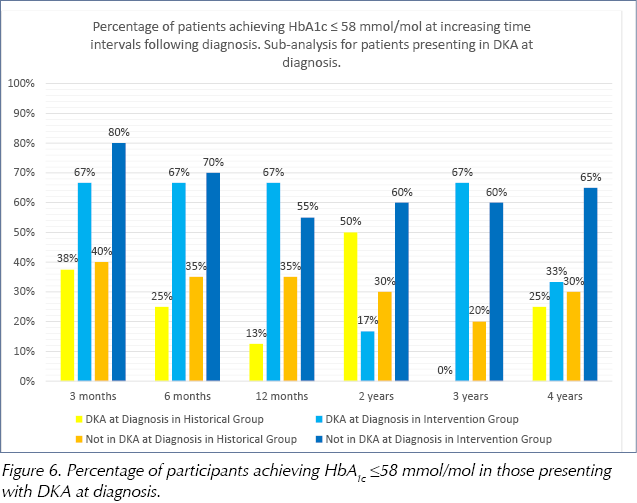
Looking at a subanalysis of those presenting in DKA or not in DKA, an improvement in percentage of CYP achieving a target HbA1c of both ≤48 mmol/mol and ≤58 mmol/mol can be seen in both groups at almost all time points (see Figure 5 and Figure 6). This further highlights the importance of the good education and training that has been achieved through increased initial follow up. It is, therefore, reasonable to conclude that CYP achieving an improvement in HbA1c did so as a result of the intervention.
Initially, the team had planned for the intervention group to have even more contacts in the first 60 days. Ideally, CYP would have had weekly consultant appointments for the first six weeks. Due to lack of diabetes MDT resources and clinic slot availability, this was scaled back to the intervention described. Further work has been done to try and achieve weekly consultant follow-up for the first six weeks. A “hidden slot” in the consultant clinic timetable has been added to allow any newly diagnosed CYP to be seen. This might explain why the majority of the increase in contact appears to be with consultants.
Future work could look at whether the improvement in HbA1c seen in this study continues with further increases in early face-to-face contact, as we had previously planned. This would be difficult to compare with the current cohort of individuals as there have been a number of further quality improvement measures and clinical practice changes. As part of the Royal College of Paediatrics and Child Health Quality Improvement Collaborative for CYP with Diabetes, several interventions have been implemented to improve the clinic experience and enable better self-management. Examples of this include a clinic goals sheet, downloading data at home or in clinic ahead of the appointment, nurse- and dietitian-led download clinics, and an alternative clinic layout.
After diagnosis with type 1 diabetes, residual beta-cell production of insulin makes optimal diabetes control more achievable. As the “honeymoon period” ends and the ongoing psychosocial demands of a chronic health condition manifest, maintaining good control becomes harder to attain (Ye et al, 2017; Tang et al, 2019). Therefore, as expected, in both the historical and intervention groups, the number of CYP who achieved an HbA1c of ≤48 mmol/mol decreased over time. Following our intervention, however, more CYP were achieving this target and more were sustaining it for longer.
In this study, we have shown that increased early contact improves glycaemic control. There are currently no guidelines for frequency of initial follow-up in CYP with newly diagnosed type 1 diabetes. Other diabetes centres that do not have as many early contacts may find this intervention useful to help improve early glycaemic control. This approach may also be applicable to the management of other chronic conditions and may be investigated further. Not all chronic conditions, however, have a good measure of long-term control such as HbA1c, and so this may make it harder to interpret.
Conclusion
Increasing the frequency of initial follow-up by consultants after diagnosis of type 1 diabetes in CYP helps improve the long-term glycaemic control up to 4 years following diagnosis. Further investigation may show that increased contact beyond what we have looked at may be of additional benefit.
Acknowledgement
The authors thank Chris Foy for his help as statistician in the preparation and revision of this manuscript, and the Gloucester Diabetes MDT.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022