Children and young adults who are newly diagnosed with type 1 diabetes can present acutely in diabetic ketoacidosis (DKA) if symptoms are not recognised early, with those <6 years of age at increased risk. It can lead to death as a consequence of cerebral oedema (Usher-Smith et al, 2011; Poovazhagi, 2014).
Globally in 2020, healthcare has been dominated by the COVID-19 pandemic. The necessary public health measures have had some inadvertent, negative consequences in paediatric care, with reports of late presentation of DKA being the commonest across UK emergency departments (Ashikkali et al, 2020; Royal College of Paediatrics and Child Health, 2020). Additionally, Kamrath et al (2020) found significantly higher numbers presenting in severe DKA during the first two months of the COVID-19 pandemic compared to previous years. Our team started to observe a similar trend across our county cohort, which led to a clinical review of our newly diagnosed patients between April and December 2020.
Clinical review
Data
From the 1 April to 31 December 2020, our county had 30 patients newly diagnosed with type 1 diabetes, compared to 28 for the 2019/20 National Paediatric Diabetes Audit year, ending March 2020. The majority (28/30) had a typical history of polydipsia and/or polyuria, with seven patients (aged 5 years 11 months to 13 years 7 months) reporting new-onset bed-wetting. Other symptoms of weight loss and tiredness varied between patients, but those who reported lethargy and vomiting presented in DKA. The classifications of DKA and management of these individuals were based on the interim DKA guideline by the British Society for Paediatric Endocrinology and Diabetes (BSPED, 2020), as our Trust guidelines aligned with the update from April.
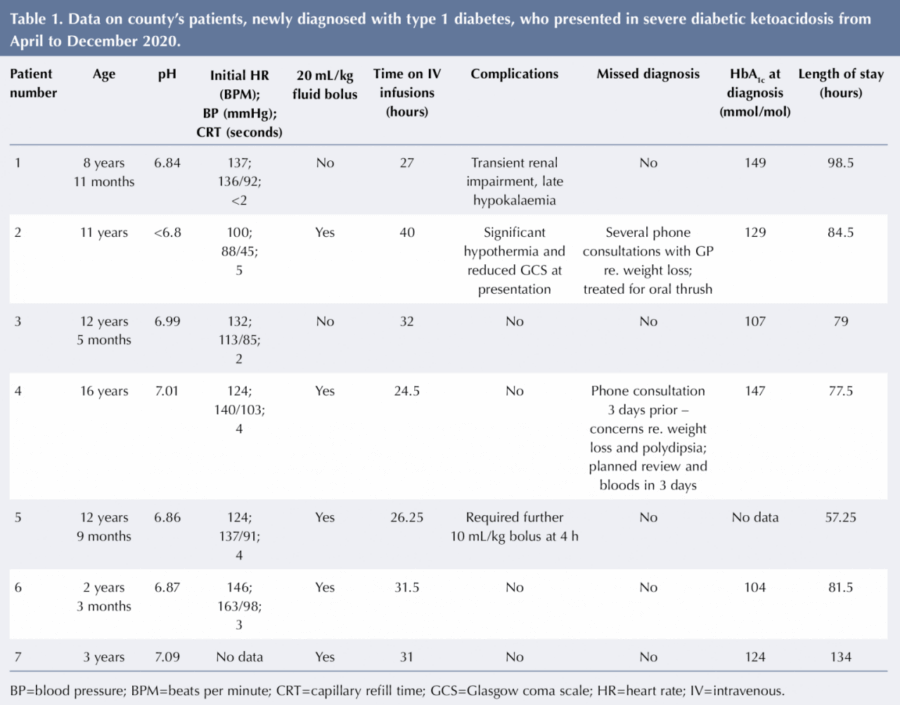
During the 9-month period, 14 patients (46.6%) presented in DKA compared to eight (28%) in the preceding year. Six (42%) of those in DKA were <6 years old, with only one additional patient <6 years presenting not in DKA. Of those presenting in DKA, seven out of the 14 were in severe DKA (pH <7.1), which was significantly more than the preceding year, with only one patient in severe DKA (7/30 vs 1/28; Fisher’s exact test, P<0.05). Five of those who presented in severe DKA were aged between 8 years 11 months and 16 years. 71% of those presenting in severe DKA required a 20 mL/kg fluid bolus of 0.9% sodium chloride after initial assessment owing to concerns of clinical shock, with no clear correlation to severity of acidosis at presentation (see Table 1).
Patient 2 presented after collapsing at home with significant hypothermia and reduced Glasgow Coma Score on admission to resus. He was discussed with the regional paediatric intensive care retrieval team, but remained under high dependency unit (HDU) care on the paediatric ward, and neurologically improved after active warming and commencing DKA treatment. His acidosis was initially slow to correct, which was likely due to under-estimation of his weight. His condition improved once fluids were adjusted for his true weight.
Patient 5 required a further 10 mL/kg 0.9% sodium chloride bolus at 4 hours because of concerns of inadequate circulation, but his fluids also needed readjusting to true weight once measured. Patient 1 had mild renal impairment, which continued after intravenous (IV) infusions had been stopped. She was encouraged to drink and subsequently developed transient hypokalaemia. This corrected with a short duration of oral potassium supplements.
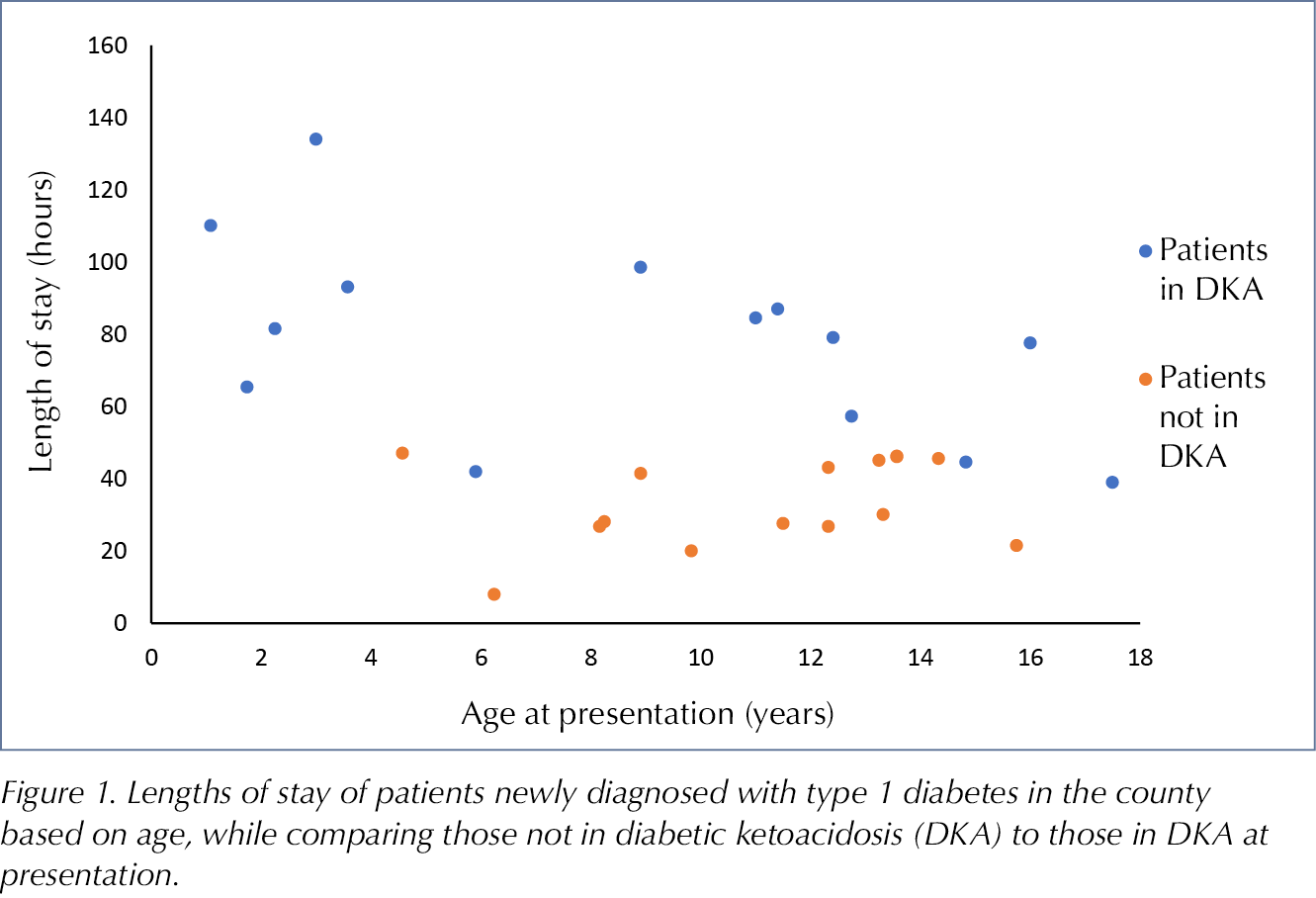
The patients in DKA required an average of 23.625 hours (range 13–40 hours) on IV infusions of fluids and insulin, which required HDU care on our general paediatric ward. Table 2 and Figure 1 show the length of stay for all patients, except one who presented not in DKA and for whom there was incomplete data. Those who presented in DKA had a significantly longer average length of stay compared to those who were not in DKA (78 hours vs 33.5 hours; t-test, P<0.001). For those <6 years old, the average length of stay was 81.8 hours. The average length of stay for all newly diagnosed patients was 55 hours compared to 38.9 hours in 2019/20. The patient who stayed for 8 hours had a parent who was a health professional experienced in diabetes management and wished to continue management as an outpatient.
There were six individuals who had a missed/delayed diagnosis of type 1 diabetes. Two of these subsequently presented in severe DKA and one in moderate DKA. For all three, the prior GP consultations had been via telephone and symptoms in keeping with diabetes had been described. Patient 2 had previously consulted their GP on a few occasions with concerns about significant weight loss. The GP was unable to see patient 4 face to face on the day of their telephone consultation, but had arranged follow-up review with bloods a few days later, which is when referral to hospital took place. For two of the patients who did not present in DKA, the diagnosis was delayed as fasting bloods, including HbA1c, were arranged 2 weeks after the initial face-to-face consultation, rather than immediate referral being made, despite one patient having glucose and ketones in their urine.
Discussion
In our newly diagnosed cohort, the majority of patients <6 years old presented in DKA, which is in keeping with previously published data of an increased risk in younger patients (Usher-Smith et al, 2011; Wolfsdorf et al, 2018). The reason for this is not clear, but is likely to be a combination of a less conventional clinical course in younger patients (so diabetes is not always considered by clinicians), and their immature compensatory mechanisms being less able to cope with the dehydration and acidosis that ensues (Usher-Smith et al, 2011). This was reflected in our two patients <2 years of age who presented with some non-specific symptoms, including parental concerns about lethargy and being unsettled, that had only been present for a short period but which quickly led to ketoacidosis. Diabetes was not the initial diagnosis considered for these individuals, but detailed assessment, including blood glucose testing for vomiting in the first patient and a urine dipstick test due to urinary frequency with fever in the second, led to the diagnoses. DKA would have been missed in the latter patient, however, had there not been an incidental fever, as the plan was to send her home with open access. This highlights the challenge of diagnosis in this age group.
A significantly higher proportion presented in severe DKA during this time period compared to the previous year, which parallels the findings from other studies (Kamrath et al, 2020; Unsworth et al, 2020). Interestingly, there were more who presented in severe DKA in the >8 years of age group, with the majority having experienced prolonged common symptoms of diabetes. It has been theorised that this relates to this age group not highlighting symptoms to parents. However, this was not the case for some of our patients, as it was parental concern over weight loss that prompted them to seek medical advice (Cherubini et al, 2020).
Five out of the seven in severe DKA were given a 20 mL/kg 0.9% fluid bolus in accordance with the BPSED interim guidelines (2020), as they were deemed to be clinically shocked with tachycardia, prolonged central capillary refill time and cool peripheries. However, NICE (2020) has suggested these signs are expected effects of ketoacidosis, and presenting shocked due to DKA is uncommon. Alongside a weak, thready (low volume) pulse, they deem hypotension a key sign of shock, which would have meant only one of our patients met the criteria for receiving a 20 mL/kg bolus. This patient, however, was significantly compromised at presentation, which may suggest that although blood pressure is an important clinical sign of shock, it should not detract from a clinician’s clinical judgement on circulatory failure. Children can compensate for some time with inadequate circulation and, as seen in our patient, hypotension may be the late stage of their clinical courses. Adequately resuscitating them prior to this would hopefully, therefore, prevent further deterioration (Samuels and Wieteska, 2016).
Prior theories suggested that fast fluid corrections cause osmolality changes and subsequent cerebral oedema (Duck and Wyatt, 1988). The PECARN study disproved this notion, demonstrating neurological sequelae in patients with DKA was not notably linked to the rate of fluid administration. This was reflected in our data, with no patients, including those who received a 20 mL/kg bolus, displaying any neurological signs during their treatment (Kuppermann et al, 2018). ISPAD echoes the findings in its updated guidance, and emphasises the importance of reinstating adequate blood volume and rehydration to compensate for losses (Wolfsdorf et al, 2018). This was reiterated in the BSPED interim DKA guidelines (2020).
On reflection, two of our severe DKA patients were initially inadequately rehydrated. This was due to calculating initial fluid requirements based on estimated weights that were significantly lower than true weights. This led to slow resolution of acidosis for one patient and another receiving an additional fluid bolus. This highlights the importance of accurate fluid calculations to sufficiently restore fluid losses.
The length of stay for our patients was longer than the previous year, but this is to be expected with a larger proportion presenting in DKA. Unsurprisingly, those in DKA had a longer admission, but they also required HDU care whilst on IV infusions, meaning larger cost implications due to more intensive nursing care. There was pressure on the multidisciplinary team owing to the increased number of new cases requiring reviews on the ward, followed by multiple virtual or home visits for extensive education after discharge. Families were eager to get home due to the distance some lived from the acute hospital and the challenges created by visiting restrictions. A new diagnosis of diabetes can create a psychological burden on the child/young person and their family, and this is now multifactorial during the COVID pandemic, with limited visiting, the initial unknown effect of COVID-19 on those with diabetes, and the added anxiety of going to nursery or school during this time (DiMeglio et al, 2020; NICE, 2020). These factors are difficult to measure but will have the greatest significance to our families, so must not be forgotten.
Misdiagnosis has been well recognised in those presenting newly diagnosed with type 1 diabetes, with one study finding a third of their patients had seen a doctor within a week prior to diagnosis (Bui et al, 2010). Twenty percent of our patients had sought medical advice in the days to weeks prior to diagnosis. The highest proportion is often seen in the younger age groups and misdiagnosis has been linked to likelihood of DKA at presentation (Bui et al, 2010; Usher-Smith et al, 2011; Muñoz et al, 2019). This was not reflected in our data, with all six patients being teenagers and half presenting in DKA. Our review period, however, did involve a national shift in clinical practice due to the COVID-19 pandemic. Primary care had to rely mainly on virtual consultations.
There have also been reports of delayed contact with health providers by parents owing to apprehension of catching COVID-19, although this was not reported by any of our parents (Elbarbary et al, 2020; Lazzerini et al, 2020). For some of our cases, the diagnosis of diabetes had not been considered in primary care despite the commonest symptoms being described, suggesting a lack of awareness of this condition. There were, however, also cases where diabetes must have been considered, as subsequent fasting bloods were arranged, suggesting a lack of awareness of same-day referral to secondary care as per NICE guidelines (2020).
The issues raised from our cases have already been actioned, with letters sent to the relevant teams, and a countywide reminder being given regarding when to consider diabetes in children and young adults and the need for immediate referral. Although we had patients misdiagnosed, there was still a large proportion of cases where typical symptoms of diabetes had been present for some weeks before families sought medical advice. There were only two documented cases where the parent recognised the symptoms suggestive of diabetes. It has been eight years since Diabetes UK (2012) launched the “4 Ts” of diabetes campaign and, with minds distracted currently by other health concerns, is it time for a refresher on the common signs and symptoms of diabetes? Cherubini et al (2020) suggest that, for this to be successful, it should capture the attention of a high proportion of relevant people, which needs to be the general public, schools and health professionals, and outcomes should be monitored with regular reviews to keep it present in people’s minds.
One of the aspects we have not considered is the longer-term consequences of presenting in DKA at diagnosis. Although none of our patients developed overt cerebral oedema during treatment, we have not subsequently assessed them for difficulties with executive functioning skills, which can manifest later due to changes in the brain microstructure (Kuppermann et al, 2018). Another possible long-term effect of presenting in DKA is poor glycaemic control, which Duca et al (2017) reported as a poor prognostic factor independent of other cofounding factors. Chronically high HbA1c into adulthood leads to significant morbidity, so it would be interesting to monitor the follow-up HbA1c results of our patients to see if there is a difference between those presenting in DKA and non-DKA (NICE, 2020).
Conclusion
Our county had significantly more patients presenting in severe DKA at diagnosis during the COVID-19 pandemic compared to the previous year, but luckily there were no associated acute complications and more time is needed to evaluate longer-term implications. Although misdiagnosis was seen for some patients, the majority had not sought medical attention prior to presentation and there seemed to be a lack of knowledge of diabetes. This would suggest a re-education of the general public and health professionals on signs and symptoms of type 1 diabetes is needed imminently.
Acknowledgements
The author would like to thank Birmingham City University and the Collaborative LBR7587 Team; the paediatric diabetes multidisciplinary team for Worcestershire Acute Hospitals NHS Trust; and the acute paediatric team based on Riverbank Ward at Worcestershire Royal Hospital.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022