In July 2016, the diabetes multidisciplinary team at Bristol Children’s Hospital started teaching level 3 carbohydrate counting to children and young people with very newly diagnosed type 1 diabetes and their families to improve rates of carbohydrate counting and blood glucose levels. An audit was carried out to assess the impact of early education on carbohydrate counting. The proportion of those able to carbohydrate count by their first multidisciplinary team clinic appointment increased from 34% to 84%, despite a reduction in the duration between discharge and first follow-up appointment. The percentage achieving HbA1c <48 mmol/mol (6.5%) at 6 months increased from 25% to 64% and the mean HbA1c dropped from 56 mmol/mol (7.3%) to 45 mmol/mol (6.3%). Prioritising early level 3 carbohydrate counting education delivery by dietitians improves rates of carbohydrate counting and has a positive impact on glycaemic control in the months immediately after diagnosis.
Background
Prior to 2016, Bristol and Weston Paediatric Diabetes Service had routinely deferred the teaching of carbohydrate counting skills until a few months after diagnosis. This approach in part reflected the challenge of maintaining carbohydrate counting skills in a large team of ward-based nursing staff across several wards who provide care for children with newly-diagnosed diabetes alongside the specialist diabetes multidisciplinary team (MDT) in a busy tertiary children’s hospital. It also resulted from a lack of specialist diabetes dietetic time.
Investment in the diabetes MDT, which provided additional dietetic resources, enabled service development. The aim was to increase the proportion of children and their carers who were level 3 carbohydrate counting from diagnosis, with the expectation that this would result in a significant reduction in HbA1c by 6 months post-diagnosis. At the outset, in July 2016, guidelines and resources for ward staff and family members were updated to ensure consistency of information and advice delivered by both ward staff and members of the diabetes MDT.
An audit was subsequently carried out to determine the proportion of CYP and their carers able to carbohydrate count at their first MDT follow-up appointment and monitor the subsequent change in patients’ HbA1c levels 6 months after diagnosis. This service development remains in operation and is currently being re-audited.
The education package
The carbohydrate counting education package consisted of two sessions following discharge after initial diagnosis. The first carbohydrate counting session aimed to occur within a week of diagnosis. This 1-hour teaching session, delivered by a paediatric dietitian consisted of a test to check carbohydrate awareness and family-specific teaching on how to obtain carbohydrate values. Resources used to carbohydrate count were:
- Food labels
- A pictorial carbohydrate counting resource (Cheyette and Balolia, 2016)
- Weighing food and obtaining values by using the carbohydrate per 100 g value.
At the end of the first session, patients were given a food diary to complete at home. The food diary documents a family’s ability to recognise and count carbohydrates and the effect of ICRs on blood glucose levels. The diary was reviewed during the second session, which took place approximately 1 week after the first session. At this time, the dietitian offered the CYP and family members help with any difficulties that they might have had. The dietitian also adjusted the ICRs and provided further re-enforcement of the previous teaching, if required.
Audit
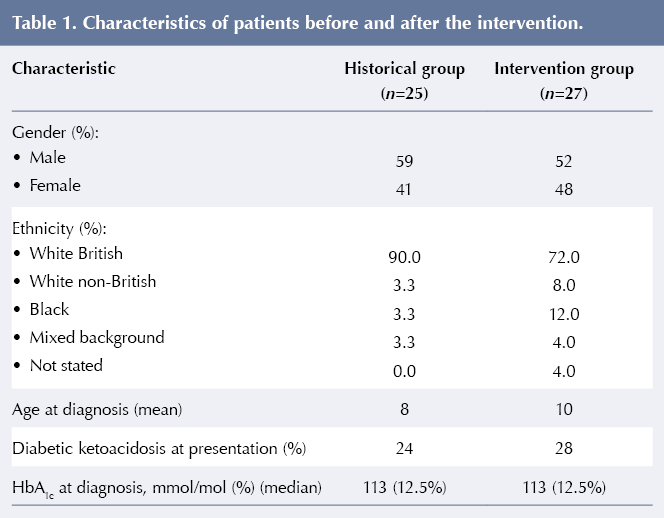
To test the effectiveness of this intervention, an audit of medical notes for all patients offered the new education package from July 2016 to January 2017 was undertaken. CYP with newly-diagnosed type 1 diabetes were numbered sequentially during this period and compared with a historical control cohort from between July 2015 and January 2016, before the education package was introduced. Carbohydrate counting education was delayed until a few months post diagnosis in the historical group due to limitations in dietitian/specialist nurse availability for early education. The historical cohort was treated with fixed insulin doses at diagnosis rather than ICRs as patients were given a standard blood glucose meter that could not offer bolus advice. No other changes in the management of CYP newly-diagnosed with type 1 diabetes were introduced during this period. To ensure we were testing the effect of implementing the new carbohydrate counting initiative, we excluded Bristol-based patients who had received their diagnosis and initial care in another trust/country (n=2). In total there were 52 patients: 25 in the intervention group and 27 in the historical cohort.
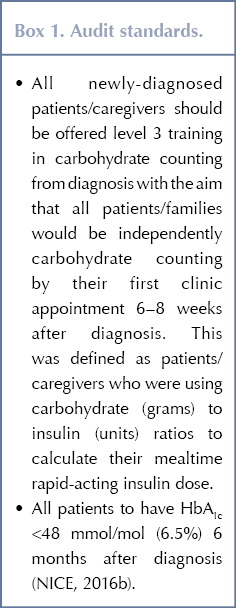
There were two audit standards, see Box 1. Details about CYP and their families’ engagement with the education package delivered by the dietitian and patients’ HbA1c results were collated using a bespoke database, the nursing and dietetic patient records. Once inputted in a Microsoft Excel spreadsheet, the data were anonymised in line with the University Hospital Bristol’s audit department guidelines and then analysed. An unpaired t-test was used for interval data comparing mean HbA1c and mean time to clinic follow-up. Fischer’s exact test was used for the nominal data comparing numbers of patients with an HbA1c below the agreed cutoff of 48 mmol/mol (6.5%) and comparing those in the two groups who could and could not carbohydrate count at their first MDT appointment. Figures were created using Microsoft Excel and statistics were performed using Graphpad.com free calculators.
Results
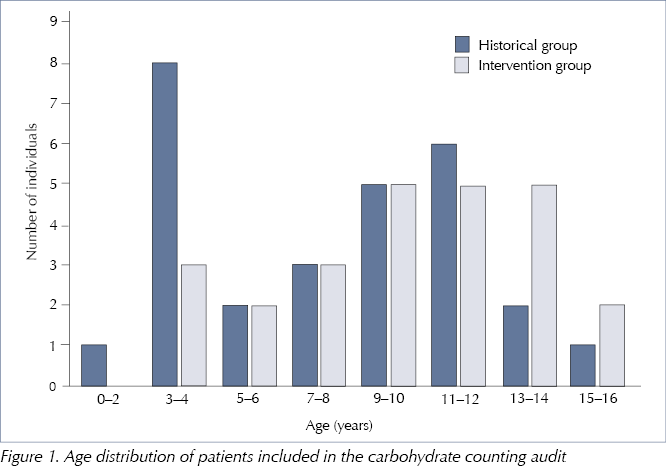
The two groups had similar demographics and clinical characteristics at diagnosis, see Table 1. Children in the historical control group were slightly younger than those in the intervention group, see Figure 1. No patients in either group were initiated on an insulin pump or continuous glucose monitoring during the audit period.
There was a significant reduction in the median number of working days from discharge to first dietetic appointment, from 25 days in the control group to 3 days in the intervention group (P≤0.0001). In the intervention group, no patient waited more than 10 days for an appointment with a dietitian; before the intervention, only five patients (19%) received an appointment within 10 days.
Historically, the first diabetes MDT meeting was scheduled 6–8 weeks after discharge following diagnosis. The average number of days before a patient’s first MDT appointment dropped from 57 days in the historical group to 31 days following the implementation of early education in carbohydrate counting. The proportion of patients/carers able to carbohydrate count at this appointment significantly increased, from 34% in the historical group to 84% in the intervention group (P=0.0005).
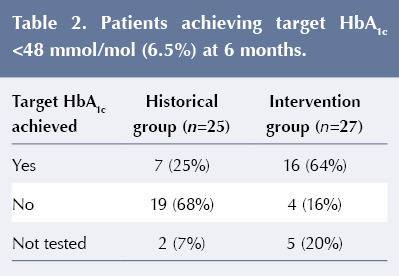
The proportion of CYP achieving an HbA1c of <48 mmol/mol (6.5%) at 6 months after diagnosis increased from 25% in the historical group to 64% in the intervention group (P=0.0008), see Table 2. The mean HbA1c recorded at 6 months was significantly lower following the intervention: 45 mmol/mol (6.3%) versus 56 mmol/mol (7.3%) (P=0.0008).
Discussion
Attempting to improve blood glucose levels early after diagnosis is key in improving long-term outcomes and introducing positive health behaviours that will continue into later life. The early introduction of carbohydrate counting aims to normalise blood glucose levels by titrating the child or young person’s meal-time insulin dose to the carbohydrate content of each meal rather than using a fixed dose based on size, age and the results of self-monitored blood glucose levels.
The two audit groups were similar in terms of gender, ethnicity, initial HbA1c and whether or not they presented with diabetic ketoacidosis. The historical group was slightly younger; however, we do not feel that this would have exerted a large effect on the outcomes measured. Our experience is generally that the engagement of families with young children with type 1 diabetes is better than from families with older children, where the children themselves are co-managing the carbohydrate counting.
The diabetes MDT considered that patients/carers should only commence level 3 carbohydrate counting when assessed as competent to do so. In the intervention group, four (16%) of the CYP and/or their carers were not carbohydrate counting at their first MDT clinic appointment, largely due to reduced numeracy or literacy skills. These individuals and their families have received ongoing support to work towards carbohydrate counting.
The improvement in the proportion of CYP/carers able to carbohydrate count at the first clinic occurred despite a concurrent decrease in the time between discharge and first follow-up clinic, which suggests that a greater proportion of CYP/carers learned to carbohydrate count in a shorter period of time. Given the similarities between the two groups and the lack of any other changes to our diabetes management, we believe that the greater proportion of patients able to carbohydrate count at their first MDT clinic appointment and the reduction in HbA1c at 6 months is most likely due to the introduction of the new carbohydrate education package. We cannot exclude the possibility that increased early contact with the MDT contributed to improved outcomes, but consider that the carbohydrate counting education package delivered in these early sessions was the major reason for the observed reduction in HbA1c.
As this audit was a retrospective case control study, there is the possibility of bias affecting the results; however, we used the objective measures of ICRs at clinics and HbA1c to minimise recall bias. The groups had similar demographic characteristics and diabetes severity at presentation and there had been no large structural re-arrangements of the diabetes team between the periods analysed, so we feel the reduction in HbA1c at 6 months is related to the intervention.
In the first 6 months post diagnosis, patients with type 1 diabetes often show a ‘honeymoon phase’, where normal blood glucose levels are more frequently achieved than in the longer term. The duration of the honeymoon period is variable and is dependent on lateness of diagnosis (ie whether patients present with diabetic ketoacidosis or not) and the effectiveness of early treatment (Abdul-Rasoul et al, 2006). This can make it difficult to assess the effect of an intervention on HbA1c. We compared the same 6-month post-diagnosis period in both cohorts, which would include any potential honeymoon phase, so the improvement in HbA1c between the groups is not likely to be due to this.
Our audit only initially examined the HbA1c at 6 months post diagnosis. Further monitoring of the HbA1c levels of these patients will be useful to determine whether this improvement is sustained. After the initial 6-month follow-up period there was a significant service reorganisation that included the introduction of point-of-care HbA1c testing. This change may have an impact on the data gathered and therefore effect the veracity of any data comparisons. A re-audit is currently being undertaken.
Conclusion
It is possible to deliver effective training in level 3 carbohydrate counting skills in line with NICE recommendations on an outpatient basis following discharge from a busy tertiary children’s hospital. Earlier introduction of carbohydrate counting was associated with a greater proportion of CYP achieving target HbA1c within 6 months of diagnosis. Longer-term follow-up will be required to determine whether this early reduction in blood glucose levels is sustained beyond the immediate post-diagnosis period.
Acknowledgements
The authors thank Carol Motteram and Gemma Martin for helping with data collection from Weston area patients.





NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022