Many approaches to providing additional support have been reported, with varying degrees of impact. This article presents an example of an intervention that University College London Hospital (UCLH) has devised that has been in place for over 20 years. UCLH is a specialist diabetes centre that receives tertiary referrals for adolescents struggling to manage their diabetes. Its four-stage plan consists of a planned admission underpinned by psychological approaches, such as solution-focused working, during which the team and child/young person explore what works, what is helpful and how this can be built upon. It is available for CYP, no matter what insulin treatment regimen they are using. The uptake has been higher in the adolescent age group. Over 85% of those admitted for the four-stage plan have been adolescents. In the current financial climate, with pressure to meet targets, hospital admission may seem an expensive solution so it is not undertaken lightly. It is initiated following an agreed pathway of nurse-led clinics, continuous glucose monitoring and psychology appointments for patients with HbA1c >80 mmol/mol (9.5%).
Background
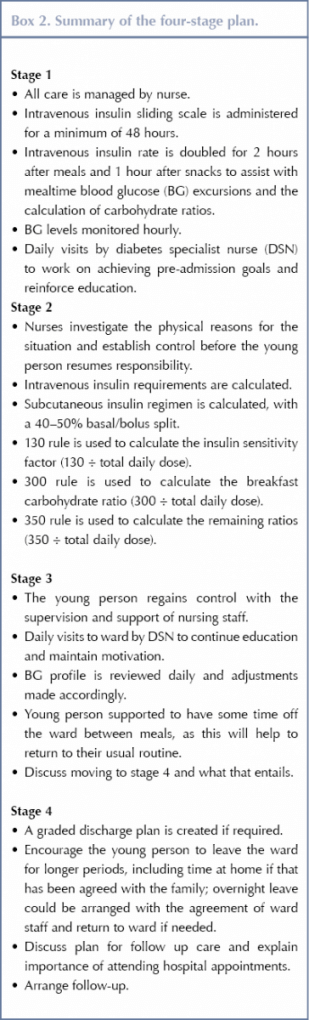
The four-stage plan evolved over 20 years ago when improvements in diabetes management were found following inpatient admissions investigating the cause of deterioration in glycaemic outcomes (Diabetes Control and Complications Trial Research Group, 1993). UCLH found that routine outpatient clinic appointments were ineffective and had poor attendance. The four-stage plan is a process by which CYP with T1D have a pre-booked admission to the hospital. Initially admission was up to 3 or 4 weeks; the average stay is now up to 2 weeks, as longer admission times proved unhelpful in terms of achieving improved glycaemic control and are financially prohibitive. The aims of the four-stage plan are given in Box 1 and the stages are outlined in Box 2.
A committed multidisciplinary team is required to young people on the four-stage plan. A solution-focused, motivation-based approach is adopted (Lange et al 2007). A committed multidisciplinary team consisting of their diabetes consultant, diabetes specialist nurses, diabetes specialist dietitians and psychologists (if therapy has been initiated) is required to adequately support young people with type 1 diabetes (Lange et al 2007).
A solution-focused, motivation-based approach is adopted. There have been improvements in glycaemic control using this approach. Rather than berating young people for not adhering to treatment regimens, there should be more focus on their achievements (Viner at al, 2003). Young people feel that an increase in positive reinforcement during clinic appointments could lead to increased motivation to improve their diabetes management (Archibald and Ashford, 2018). Wang et al (2006) attributed their findings that motivational interviewing failed to demonstrate improvement in metabolic control to the potential proficiency of the motivational interviewing training diabetes teams received. Young people have also suggested that clinicians help them to find solutions and to set realistic targets to manage their diabetes (Archibald and Ashford, 2018).
There is a wealth of evidence pertaining to the difficulties adolescents with T1D endure (Bartoscas, 2007; Viner 2008; Markowitz and Laffel 2012; Dovey-Pearce and Christie, 2013; Cameron et al 2014; Delameter et al, 2014, 2018), indicating that more attention and support from diabetes healthcare teams is required. Adolescence is a notoriously stressful stage of development for young people, occurring at a developmental stage that is extremely turbulent – not only due to the physical growth and hormonal changes, which can have a significant impact on glycaemic control, but also social and psychological changes that are taking place simultaneously (Cameron et al, 2014). Young people may rebel against the rigid routine that diabetes affords, paying no attention to the consequences to their health (Lewis, 2013).
Adolescence is associated with an increased incidence of anxiety, depression and psychological distress (Delameter et al, 2018). A systematic review and meta-analysis found that 30% of CYP with T1D had depressive symptoms, the levels of which were correlated with glycaemic control and three-way interactions between HbA1c, blood glucose monitoring frequency or diabetes-specific stress and depression (Buchberger et al, 2016). The same study reported that symptoms of anxiety were present in up to 32% of CYP with T1D.
During adolescence, parents take a step back and young people are discovering their identity and striving for independence. However, diabetes is often found to be much more demanding than anticipated and parental support is paramount to guide the young person through this turbulent period (Cameron et al, 2014). Both the degree of parental involvement and the timing of the transfer of responsibility of care can influence glycaemic control. Both intrusive and diminished parental involvement has been associated with poor outcomes (Wysocki et al, 2006). The NICE (2016) guidelines recommend asking the young person how they would like their parents/carer to be involved, and this should be reviewed on a regular basis.
Borus and Laffel (2010) suggest that education at diagnosis is often directed towards parents, so the child does not appreciate the enormity of what managing diabetes entails until he or she takes over. Consideration must therefore be given to when this handover of care occurs. Hilliard et al (2011) suggest that post diagnosis-related stress can result in reduced parental understanding of diabetes management and increased childhood behavioural problems. Fear of hypoglycaemia in both parents and young people is also a significant contributory factor in poor glycaemic control (Barnard et al, 2010). Successful education empowers and motivates young people, promoting skills in self-management that can be utilised in their lives (Von Sengbusch et al, 2006). Through such education, young people often realise that they know more than they appreciated, which increases their confidence, enabling them to become an expert in their healthcare and promote self-management of their condition.
The four-stage plan
Frequent hospital admissions with unexplained hypoglycaemia, diabetic ketoacidosis and apparent insulin resistance are precursors for referring a young person to undertake a four-stage plan. Prior to admission, the diabetes team clearly outlines what the plan entails to the young person and his/her family. The ward staff are informed and a bed is booked. The young person and his/her family are encouraged to set realistic, achievable goals.
Stage 1
The young person is admitted on an agreed date and a timetable for the admission is drawn up. Intravenous insulin is administered using a sliding scale for a period of at least 48 hours. The objectives are to calculate the participant’s current insulin requirements, determine whether intravenous insulin controls blood glucose levels, to eliminate potential medical causes for poor control, and to re-establish insulin sensitivity.
Education is a key element of the admission. Education is tailored towards the goals set by young person. Young people find this more beneficial as it gives them the opportunity to review their knowledge and skills in managing their diabetes (Borus and Laffel, 2010). However, there are areas that need to be affirmed, such as managing hypoglycaemia, hyperglycaemia, sick days and exercise, and assessing carbohydrate counting skills. Their knowledge is assessed by reinforcing overall management of their diabetes and focusing on the areas that are proving to be difficult. This is done by using locally developed resources based on current guidelines (Phelan et al, 2018). Knowledge is reassessed as an ongoing process at every nurse-led clinic during follow-up and medical clinics.
A planned education programme is compiled around the ward activities and school, according to the availability of the diabetes team. The paediatric diabetes specialist nurse and paediatric diabetes dietitian see the patient daily to provide consistent, current information. Guidance suggests that structured education programmes, such as those implemented in CASCADE (Christie et al, 2016), the Kids in Control of Food (KICK-OFF) study (Price et al 2016) and Families, Adolescents, and Children’s Teamwork Study (FACTS; Murphy et al, 2007), influence improvements in diabetes control and management, although evidence has failed to demonstrate significant effects on glycaemic control. Such programmes are associated with improvements in quality of life, which must be a contributory outcome when considering living with a lifelong condition such as T1D.
Psychology is incorporated into the plan if the young person has agreed and therapy has already commenced. Psychological review does not, however, include a measure of quality of life. Flannery et al (2017) argue that measuring the outcomes of psychological well-being does not allow for personal experiences and that existing tools are not specific enough to capture a meaningful measure of well-being. Patient-centred care means listening to the stories and life experiences of young people (Flannery et al 2017).
Stage 2
Subcutaneous insulin doses are calculated using intravenous requirements and insulin sensitivity is resumed. The basal requirement, carbohydrate ratios and blood glucose targets are then set. Nurses provide all of the care at this stage. They determine whether improved glucose management with increased time in target range is achievable or whether there are any physical reasons for the young person’s raised glucose levels. If this is challenging, it provides a basis for reflective discussion about the self-management challenges faced by the young person. Care is taken to avoid judgemental discussions around diabetes management (Viner et al, 2003).
Diabetes is a relentless, ever-present part of the young person’s life, so this time provides the opportunity for him/her to have a ‘diabetes holiday’ and a break from the daily turmoil. Young people are given time to talk and encouraged to participate in decision-making to maintain a degree of control over the process (Viner, 2008).
Stage 3
The young person starts to resume responsibility for diabetes management when his/her blood glucose levels are closer to their target levels. Ward nurses provide the young person with support and prompts regarding carbohydrate counting, cannula site rotation and the performance of blood glucose checks. The paediatric diabetes specialist nurse, paediatric diabetes dietitian and psychologist will see the young person, as agreed on their timetable, to continue education and assess progress.
At this point, consideration is given to whether a graded discharge process required. Graded discharge may be needed as young people may have difficulties with travelling to and from hospital and the logistics of retaining their bed on the ward could interfere with this.
Stage 4
Once glycaemic control is maintained, the young person resumes full responsibility for his/her diabetes and is encouraged to take time away from the ward, which could involve overnight stays at home as part of the graded discharge process. This provides time for the young person to reflect on what has gone well while he/she is at home, continues positive reinforcement and motivation, and demonstrates that he/she is able to manage diabetes independently away from the support available at the hospital.
The importance of follow-up, which includes frequent clinic appointments, is discussed. It is emphasised that this four-step intervention is the first step moving forward and not a ‘quick fix’ for the young person’s T1D.
Snapshot review
A snapshot retrospective review was undertaken to determine the effectiveness of the four-step intervention (Pichierri et al, 2016). Ten admissions between May 2014 and January 2016 were reviewed (eight female and two male). The young people were aged from 13 to 17 years and all were on insulin pump therapy and demonstrating unusual, unexplained blood glucose trends, which could be either prolonged hypoglycaemia or recurrent episodes of diabetic ketoacidosis or both. Their duration of diabetes ranged from 2 to 14 years. Psychology was continued during the plan if it had been initiated beforehand, and three of the 10 patients continued with this therapy. The patients stayed in UCLH for between 7 and 14 days. Data were obtained pertaining to the young people’s HbA1c levels and hospital admission rates.
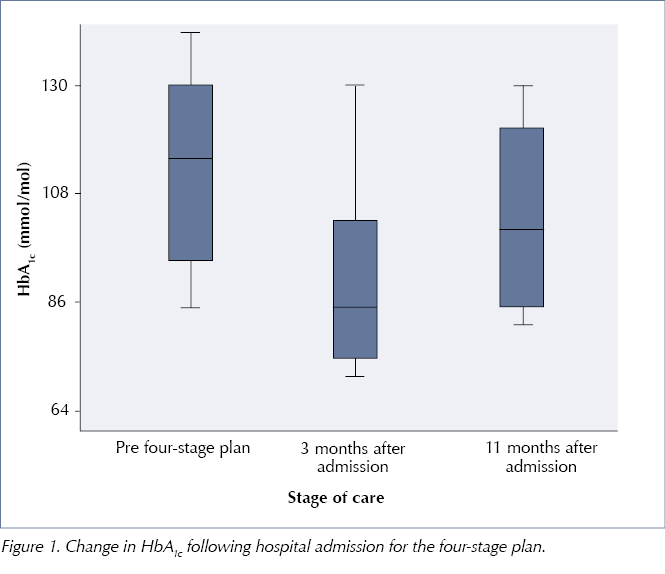
Follow-up data were available for all 10 patients (median follow-up 0.9 years). Their HbA1c levels dropped in the first 3 months after participating in the four-stage plan (P=0.05) but rose thereafter, see Figure 1. Almost a year after the intervention, their HbA1c levels were only slightly, but not significantly, lower than prior to admission. There was a slight reduction in emergency hospital admissions rate following the intervention. No diabetes-related hospital admissions were recorded during the follow-up period; however, due to the small numbers reviewed this cannot be considered significant.
Young people provided feedback on the intervention. They described their diabetes as being ‘more under control, less hassle’ and said that they ‘feel able to trust their pump settings’. They said that they felt ‘more able to manage diabetes independently’ and reported ‘increased confidence in using features on the pump independently, e.g. temporary basal rates, extended boluses’. Two of young people requested admission for a second four-stage plan when they felt they were losing control again.
Discussion
The four-stage plan poses a number of challenges. From young people’s perspective it requires considerable commitment from them and their families. It could mean them missing school, work or college. From a ward perspective, there is an impact on both workload and bed availability. It is important that ward staff are involved in planning the admission and are fully prepared, as they will be required to take an active role in the young person’s diabetes management. Despite careful planning, admission dates may need to be changed as emergency admissions take priority over planned admissions. This process also blocks a bed for a significant period of time, which has financial ramifications.
The hospital is not the appropriate environment to confirm glycaemic control, as the young person’s activity levels are reduced and his/her routine is disrupted. A long admission could result in distorted outcomes and frustration. It is therefore important to manage expectations during the goal-setting stage of this process. Young people must be encouraged to go home or at least spend some time off the ward after completion of stage 2 of the plan to demonstrate that they can manage their glycaemic levels outside the hospital environment.
Follow-up is vital. Weekly or fortnightly nurse-led clinics are booked, however these are often poorly attended. One suggestion could be to provide a structured pathway for follow-up. Part of this must include psychology, as this is often the root of poor diabetes management. Psychological treatment would then become an integral part of the plan, so the young person would need to be made aware that this was an expectation when he/she agreed to the admission.
The psychology team at UCLH run group sessions called the Tree of Life for young people with T1D (Casdagli et al, 2017). This focuses on their strengths and abilities in life apart from diabetes and enhances their self-esteem, allowing them to build their confidence and reduce the negative impact diabetes has had on their lives. This could be incorporated into the follow-up plan for these young people. (Casdagli et al 2017). The effectiveness of Tree of Life remains to be seen and requires further investigation.
Follow-up will include one or two weekly hospital-based outpatient clinics, depending on the level of concern the diabetes team bestows upon them. Introducing virtual clinics, such as Skype or telephone clinics, could supplement these.
Education will also be reviewed in group ‘refresher’ sessions, using scenarios as a point of reference and examples of how they would manage those situations. We are planning to introduce this for young people who were diagnosed in early childhood when they prepare to leave primary school as a means to support them in taking over responsibility for managing their diabetes.
Conclusions
The four-stage plan appears to produce a transient reduction in HbA1c. This could be the result of initial intensive management and support that is not adequately reinforced. The initial outcomes, if short-lived, prove that this process does help young people to ‘get diabetes back on track’ and increases their confidence in managing diabetes, thereby improving their quality of life. It is up to diabetes teams to investigate ways of maintaining this positive effect.
Further studies on the effects of this intervention are indicated to determine how diabetes teams can achieve much longer-term sustained improvements in outcomes to support young people and their families.
Acknowledgement
The author would like to thank her colleagues Francesca Annan, Clinical Specialist Paediatric/Adolescent Diabetes Dietitian, Rebecca Martin, Nurse Consultant for Paediatric and Adolescent Diabetes and Professor Peter Hindmarsh, Consultant in Paediatric Endocrinology and Diabetes for their support in writing this article.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022