Type 1 diabetes mellitus (T1DM) is a common condition in childhood. It poses serious health risks and is associated with devastating long-term complications and a 20-year reduction in life expectancy (McKnight et al, 2015). The prevalence of T1DM is higher in the UK than in most other European countries and the incidence is increasing each year; the National Paediatric Diabetes Audit (NPDA) reported an increase from 22.6 new cases per 100,000 in 2013/14 to 26.5 new cases per 100,000 in 2014/15 (Royal College of Paediatrics and Child Health [RCPCH], 2016). Despite its increasing prevalence, paediatric diabetes outcomes and organisational structures in the UK were poor and HbA1c figures were considerably worse when compared to similar countries. In 2010, the median HbA1c for children and young people (CYP) in the UK was 73 mmol/mol (8.9%), and less than a third of young people aged 12 and above had received all of the key care processes recommended for this patient group (RCPCH, 2016). In comparison, the mean HbA1c in Germany and Austria was 65 mmol/mol (8.1%) (Rosenbauer et al, 2012; Bohn et al, 2016). In comparison, the mean HbA1c in Germany and Austria was 65 mmol/mol (8.1%) (Randel, 2012; Bohn et al, 2016). In 2015/16, the NPDA showed an improved national mean HbA1c of 67.8 mmol/mol (8.4%) (RCPCH, 2016). It has been estimated that a 4 mmol/mol (0.4%) reduction in mean HbA1c would save the NHS £995 million over the next 25 years, demonstrating that modest improvements in glycaemic control can generate huge reductions in the cost of diabetes complications in people with type 1 and 2 diabetes (Baxter et al, 2016).
National quality initiatives
To standardise UK diabetes healthcare and improve outcomes for CYP with diabetes, several national quality initiatives have been conceived and implemented in recent years. These have included the National CYP Diabetes Network, the Best Practice Tariff (BPT) and National Diabetes Peer Review Quality Assurance Programme (DQUINs).
National Children and Young People’s Diabetes Network
The National CYP Diabetes Network was formed in 2009 with the support of NHS Diabetes. This consisted of 10 regional CYP diabetes networks comprising of multidisciplinary healthcare professionals looking after CYP with diabetes with essential managerial support to the networks. The aims were to develop national standards of care, share good practice, improve quality standards, advise health commissioners and act as a forum to ensure equity.
Since its inception, the National CYP Network has supported paediatric diabetes units (PDUs) struggling to drive change to achieve service improvements and actively promotes feedback and collaboration with families with diabetes. This initiative has resulted in:
- Individual school healthcare plans for all CYP nationally
- A single database for all CYP with diabetes
- NPDA data submission from all PDUs,
- Improvements in shared guidelines and operational policies to reduce the disparity between service providers.
In 2013, in collaboration with NHS Diabetes and the Department of Health, the National CYP Network produced a 5-year national paediatric diabetes service improvement delivery plan aimed at achieving better health outcomes for CYP with diabetes by improving the quality of planning, service redesign and commissioning.
Best Practice Tariff
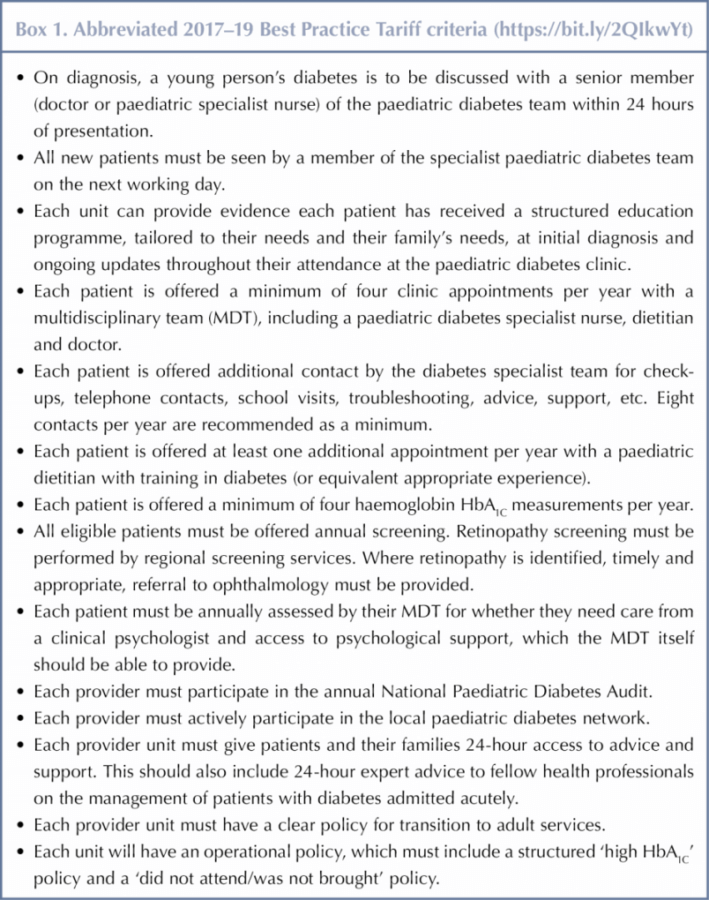
The BPT was introduced in April 2012, comprising of 13 national mandatory standards to be met by each PDU, with a tariff of £3,189 per individual per year to be paid to the PDUs that achieved all the requirements (Randell, 2012). These standards have since been slightly revised, see Box 1. PDUs failing to meet the mandatory standards of care were supported by the regional and national networks to deliver these standards within a year. Since April 2013, services that have not met the BPT standards have not been able to claim any funding from local commissioners to provide their CYP diabetes service. As a result, local commissioners have been asked to consider making alternative provider arrangements for CYP with diabetes in their area.
The BPT has provided not only clinical goals but financial incentives for improved care for CYP with T1DM. While limited resources and staff shortages initially made these standards unachievable, NHS providers and commissioners took notice and investments were made in paediatric diabetes care.
National Quality Assurance Programme
In 2013, a DQUINs were implemented in all PDUs. The units underwent self-assessment followed by external certification of assessments by peer review visits. The programme was based on the fundamental principles of being clinically led, confirming the quality of service via comprehensive peer review and user and patient involvement, and publishing reports providing accessible information about the quality of the services (National Peer Review Programme, 2013).
Aims
The aims of this study were to assess the impact of the National CYP Diabetes Network, BPT and DQUINS and to explore trends in paediatric diabetes care within all PDUs in the CYP North West Diabetes Network.
Method
The North West CYP Diabetes Network is the largest regional CYP diabetes network in the UK. Data were collected from each PDU in the region and extracted from the NPDAs from 2010/11 to 2015/16. We compared staffing before and after the national initiatives, mean HbA1c values and the percentage of patients with HbA1c <58 mmol/mol (7.5%). Data were analysed using paired student T-tests.
Results
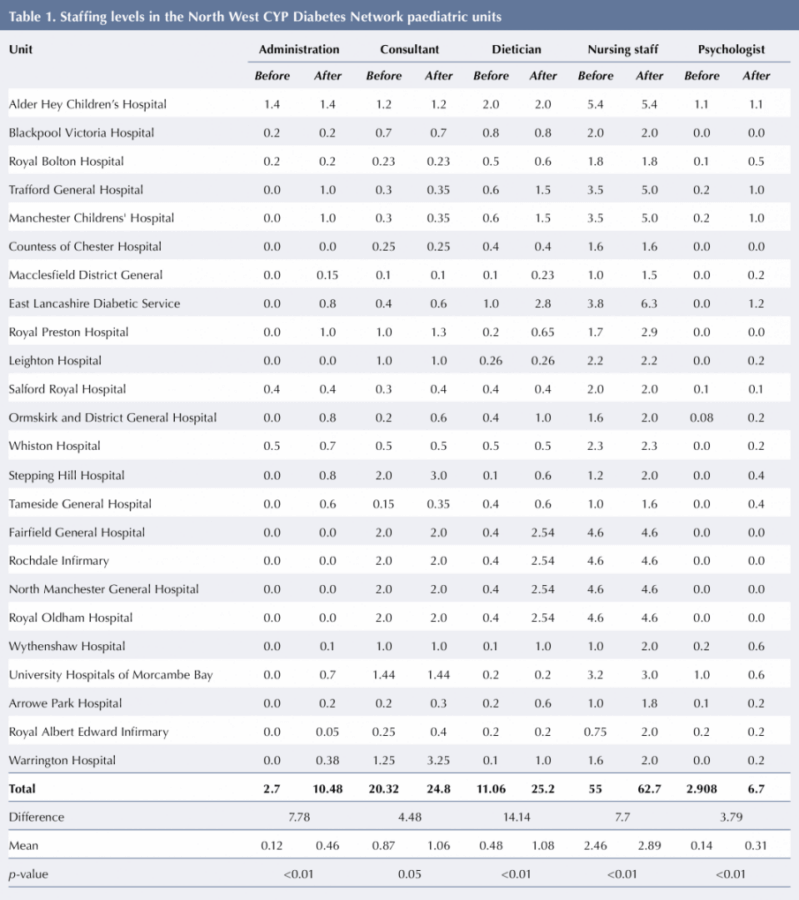
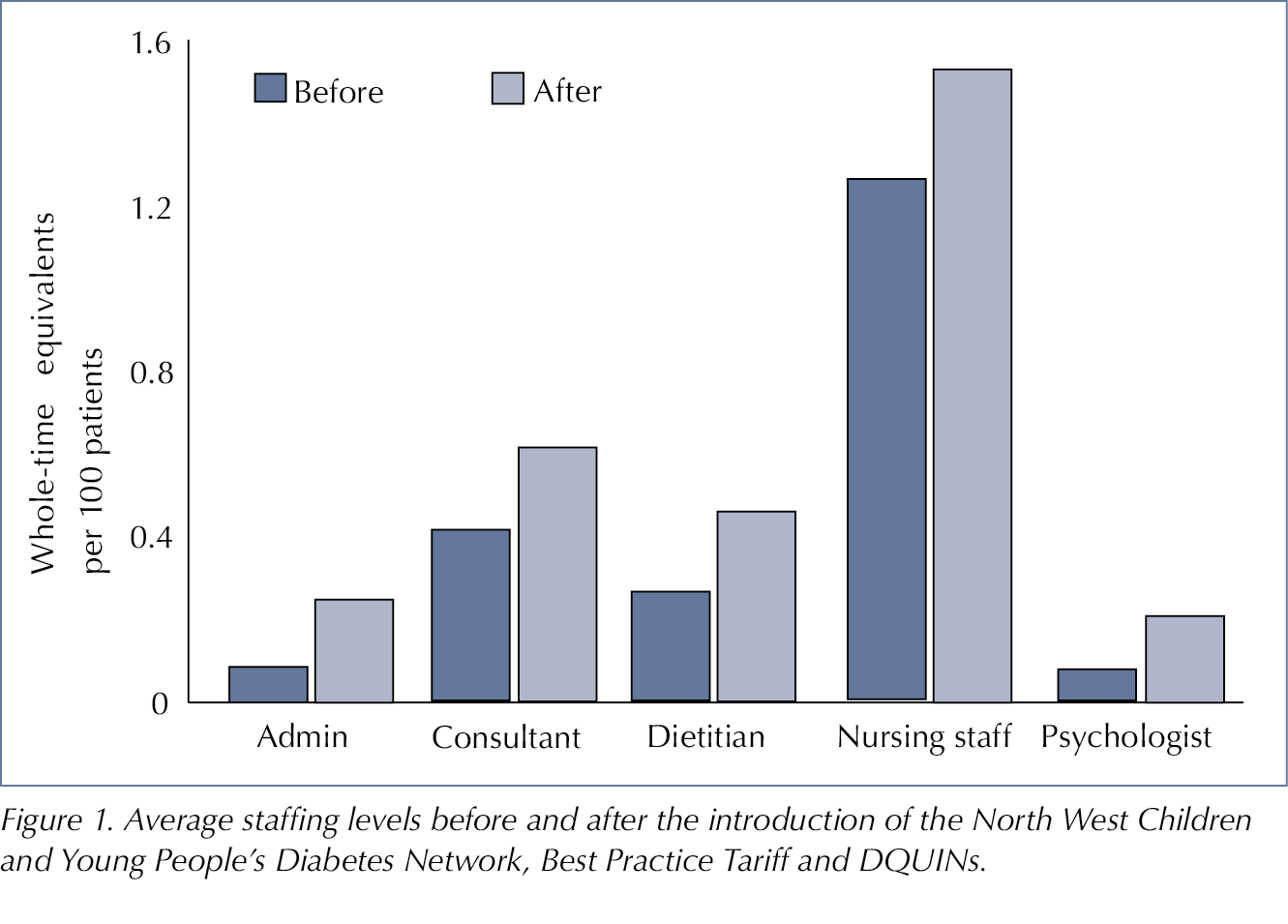
Data on staffing levels before and after the implementation of the BPT and DQUINs were collected and received from all 24 PDUs within the CYP North West Diabetes Network, see Table 1. There were significant increases in full-time equivalent administrative staff (p<0.001), consultants (p=0.03), dieticians (p<0.01), specialist diabetes nurses (p<0.01) and psychologists (p=0.01) across the network after the BPT and DQUINs were introduced, see Figure 1.
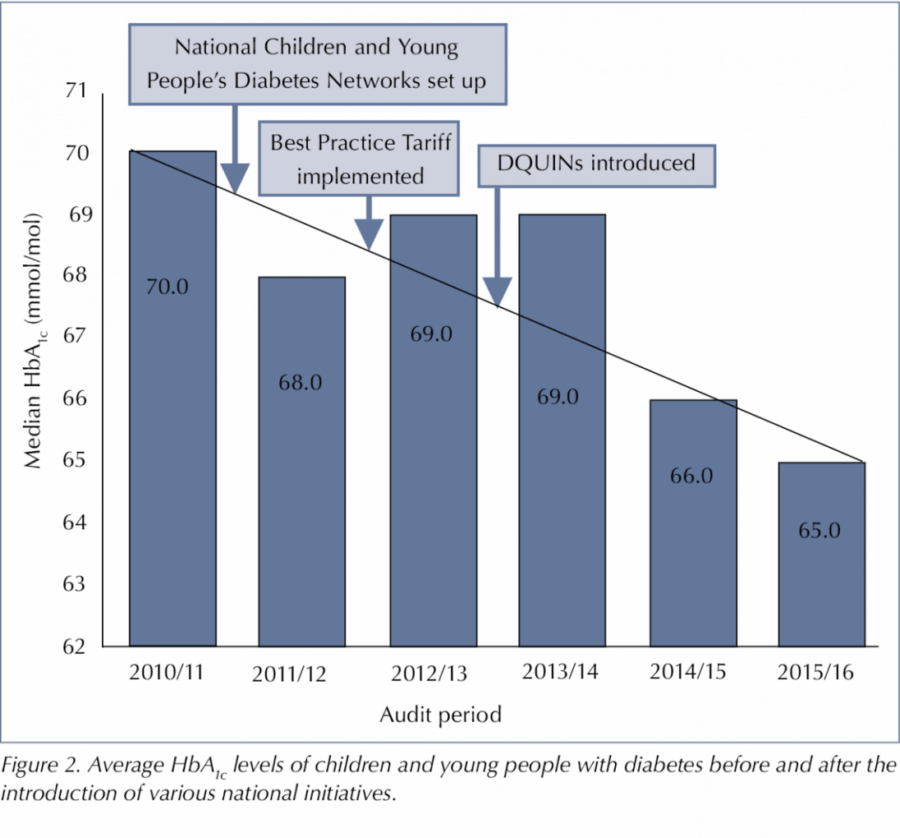
Data relating to CYP HbA1c levels were extracted from the NPDA for the years 2010/11, 2011/12, 2012/13, 2013/14, 2014/15 and 2015/16. There was a statistically significant improvement in the percentage of patients with HbA1c <58 mmol/mol (7.5%) when compared year on year, with significant improvement between 2010/11 and 2015/16. The mean HbA1c was also significantly improved for each year and compared to baseline at 2010/11 prior to the national initiatives, see Figure 2.
Discussion
Since the formation of the national CYP diabetes network, the introduction of the BPT and the implementation of DQUINs, there has been a dramatic and significant improvement in PDU staffing levels across all groups, from consultants to administrators, in the North West region. In practical terms, this means that each group can spend more time dedicated to the care of CYP with diabetes. More diabetes specialist nurses will ensure better care and education is delivered to CYP with diabetes and improved resources, such as home visits, support for school and education, the delivery of age-appropriate structured education and acting direct points of contact for GPs and families. Dieticians were now able to deliver group education and hold one-to-one consultations with patients, as well as taking part in multidisciplinary clinics. Clinical psychologists, who were not part of the diabetes teams in the past, are now being appointed within PDUs to deliver a holistic service encompassing psychosocial aspects of diabetes care in CYP.
Setting standards for paediatric diabetes care and appropriate staffing levels are critical to delivering a good service and improving health outcomes. Provider NHS trusts have made huge investments in PDUs, with the main driver for change being the knowledge that the BPT will be removed if mandatory standards are not met.
Over the past 6 years, the North West CYP Diabetes Network has also seen a significant and continued improvement in our mean HbA1c levels and increases in the percentages of patients with HbA1c <58 mmol/mol (7.5%) over the past 5 years. In 2015, 176 PDUs were audited in England and Wales and 24% of CYP were found to have HbA1c <58 mmol/mol (7.5%) (RCPCH, 2016). This mirrors results seen in Germany and Austria. Rosenbauer and colleagues examined trends in the metabolic control of children and adolescents with T1DM over a 15-year period. They found an improvement in HbA1c levels across all insulin regimens, leading them to conclude that it was the development of the multidisciplinary care team and improvements in the structural quality of diabetes care and patient education that had led to the improved results and outcomes (Rosenbauer et al, 2012).
Investments and national initiatives to improve paediatric diabetes care are in the best interest of CYP with diabetes. While we are seeing significant improvements, there are fewer than one in six CYP achieving HbA1c values of <48 mmol/mol (6.5%), which has been identified as providing the best future outcomes. A significant proportion of CYP have levels that are much higher than this. In 2015, 21% of CYP in England and Wales had a mean HbA1c values of >80 mmol/mol (9.5%) (RCPCH, 2016). There remains a wide variation in outcomes between PDUs that are achieving BPT. There must be a link between diabetes strategies and frontline quality improvements for CYP with diabetes. This needs to be provided by national leadership and direction from both clinical and political leaders to champion excellent diabetes care in the UK.
While many national initiatives have shown quality improvements, the NHS has been faced with budgetary constraints in recent years. Unfortunately in 2016, as a result of the reorganisation of health care under NHS England’s Organisational Alignment and Capability Programme, the DQUINs National Peer Review Programme lost its funding. A programme called the Quality Surveillance Team was formed to continue the progress (Waldron and Campbell, 2015) and in October 2017, the RCPCH launched its new CYP Diabetes Quality Programme of Peer Review and Quality Improvement Collaborative across PDUs in England and Wales. Devised and supported by the National CYP Diabetes Network, comprising 11 constituent regional networks, the programme is clinically driven and aims to further transform outcomes for the approximately 29,000 CYP living with type 1 and, increasingly, type 2 diabetes (RCPCH, 2017).
While national initiatives in paediatric diabetes care has been at the forefront of drivers for change in past years, there are concerns that such standards and focus only applied to CYP under the age of 19 and did not include preparing young people for the move to adults services. There are now clear gaps between PDUs and adult diabetes units, and more work needs to be done to address the transition from child to adult services, including incentives such as BPT in adult diabetes.
Patients and families must be at the forefront of any quality improvement initiatives and the success of national initiatives is dependent on collaboration between clinical networks and national organisations to improve the quality of care for CYP with diabetes.





NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022