Diabetic ketoacidosis (DKA) is a very serious condition that usually affects people with type 1 diabetes, and occasionally those with type 2 diabetes (Klingensmith et al, 2013). It happens when there is a lack of insulin in the body and the body switches to usage of fat as the source of energy, producing ketones as a by-product (Yan et al, 1983). The various signs and symptoms can be polyuria, polydipsia, confusion, rapid breathing, fruity breath odour, blurring of vision, lethargy, abdominal pain and vomiting. It is vital that DKA is diagnosed and treated urgently in order to avoid development of cerebral oedema, which can be life threatening (Rwiza et al, 1986; Murunga and Owira, 2013).
Case report
An 18-month-old male was referred from primary care during the night with a provisional diagnosis of constipation and suspected intestinal obstruction. He was looking unwell and his mother’s main concerns were that he had not opened bowels for 9 days, he had become very drowsy over the past 6 hours and had been vomiting. He subsequently developed abdominal distension. There was no history of fever. He had recently developed polyuria and polydipsia, along with weight loss, which was not documented. The mother reported that he had always suffered from constipation and would open his bowels once every 7–8 days.
Pregnancy was uneventful, he was born at 40 weeks 6 days (normal antenatal scans), by normal vaginal delivery, and the birth weight was 3.232 kg. He passed meconium within the first 24 hours of birth.
On further questioning, it was revealed that his speech was limited to bi-syllables. Furthermore, he could not sit up from a lying position and, when he did sit up, he could not hold himself upright with a straight back. He was unable to lift his hand above his head and he had not started walking but enjoyed playing with toys.
There was a family history of type 2 diabetes in both parents’ grandparents. His parents were fit and well apart from the mother’s history of Perthes’ disease as a child. His weight on admission was 10.5 kg (16th percentile).
Examination
On examination at admission, the child’s Glasgow Coma Scale (GCS) score was 8/15. He was moaning, had cool peripheries, tachypnoea and shallow breathing. He had a normal cardiovascular examination apart from tachycardia. He had marked abdominal distension with normal bowel sounds, no signs of peritonitis and there were palpable faecoliths all over the abdomen.
There was significant lower limb hypotonia and hyporeflexia. Calf muscle size was normal with downgoing plantar reflexes bilaterally. Both the pupils were equal and reactive. The genitalia looked normal and no dysmorphic features were noted. His heart rate was approximately 140 beats per minute, capillary refill time was <2 seconds centrally and 5 seconds peripherally. Blood pressure was not recordable and pulses were thready. A provisional diagnosis of sepsis was made and a fluid bolus of 20 mL/kg (normal saline) was being prepared as we performed the blood gas. The venous blood gas results and other blood test results are shown in Table 1.
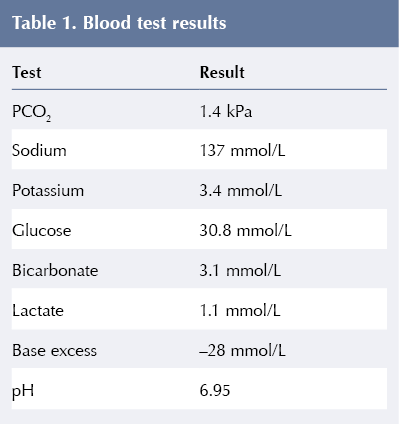
HbA1c at presentation was 91 mmol/mol (10.5%), so the child was managed as having severe DKA and British Society for Paediatric Endocrinology and Diabetes (BSPED, 2020) DKA guidelines were followed (Heddy, 2020).
We suspected cerebral oedema due to his low GCS, along with the abnormal neurological examination; therefore, he was treated with hypertonic saline. A subsequent CT scan did not show any signs of cerebral oedema. The DKA gradually resolved over the next 18–24 hours.
As part of initial work-up, he was found to be positive for anti-islet cell antibodies, with normal thyroid function tests and negative coeliac screen. Later, to evaluate hypotonia, magnetic resonance imaging of his head was undertaken. This revealed diffuse abnormal symmetrical changes involving the deep white matter of the cerebral hemispheres, with associated cortical abnormality predominantly involving the inferior surface of the temporal lobes. The occipital cortex had cobblestone polymicrogyria. The karyotyping and SNP (single-nucleotide polymorphism) array was normal.
Guidance on DKA management
The updated BSPED guidance from January 2020 has been adapted to a more flexible usage of resuscitative and maintenance fluids (Prentice, 2021). The rationale for this was based on new evidence from the Paediatric Emergency Care Applied Research Network (PECARN) DKA Fluid trial, which suggested that there is no significant difference in outcomes between rapid and slower administration of fluids while managing DKA (Kuppermann et al, 2018). The trial also showed that the initial conscious level was closely related to pH and weakly to age, but not to the levels of blood glucose or plasma sodium (Edge et al, 2006; Kuppermann et al, 2018).
COVID-19 pandemic and the impact on DKA management
A national survey undertaken by the UK Association of Children’s Diabetes Clinicians found that the proportion of children and young people with new-onset type 1 diabetes presenting with DKA during the COVID-19 pandemic was higher than previously reported and that there has been an increase in presentation of severe DKA at diagnosis in people under the age of 18 years (Ng et al, 2020). Up to 20% of units have documented delayed presentations of type 1 diabetes, for multiple reasons, ranging from fear of COVID-19 to an inability to contact or access a medical provider for timely evaluation (Ng et al, 2020).
It is possible that, as with many other cases presenting during the COVID-19 pandemic, the case of this 18-month-old boy may have been the consequence of a lack of GP appointments during the pandemic. This may have contributed to severe constipation and gross developmental delay/hypotonia going unnoticed. Moreover, as the pandemic put a strain on the healthcare system, health visitor appointments may have been cancelled, resulting in many missed opportunities to detect the health problems (Logan et al, 2020).
The adaptations to NHS working during the pandemic could have contributed to the delay in diagnosis of diabetes and this may explain why many patients progress into DKA at the time of initial presentation (International Society for Pediatric and Adolescent Diabetes, 2020).
Diabetes education and additional challenges
Diabetes education is essential for the whole family once there has been a diagnosis of type 1 diabetes. The physical and mental health problems of any family member can be a challenge when trying to deliver the education effectively.
In this case, educating the parents about diabetes was extremely challenging, as the mother had not completed her schooling and our team suspected that she may have had mild learning difficulties. The father had a diagnosis of attention deficit hyperactivity disorder (ADHD). It was decided that the diabetes education should be provided in stages and their understanding was double-checked at every point. The child’s mother preferred making notes and his father liked to watch videos to learn. A great deal of reinforcement was required with both parents regarding tackling hypoglycaemic episodes and other aspects of the condition.
The child stayed in the hospital for approximately 8 weeks, until the team was confident about the level of diabetes care at home. Thankfully, effective education must have contributed to the successful management of diabetes in this case, as reflected by the HbA1c, which dropped down to 52 mmol/mol (6.9%) 8 weeks post-discharge.
Holistic management
As this was a complex case, a multidisciplinary approach was followed. Along with the diabetes team and a general paediatrician, a community paediatrician was involved for ongoing care. The child was also referred to the muscle disorders team for further evaluation and management. Genetic tests were undertaken as well.
As is evident from this case, a multidisciplinary approach is a must, along with being consistent, in order to achieve the best outcomes in complex conditions like diabetes (Yan et al, 1983).
Conclusion
DKA is a very complex condition and the COVID-19 pandemic made it even more difficult to diagnose and manage. This was a challenging case in which the child was initially referred for severe constipation with possible intestinal obstruction and eventually diagnosed with DKA. While in hospital, he was found to have associated generalised hypotonia and global developmental delay. Possible maternal learning difficulties and ADHD in the father warranted prolonged education sessions and a multidisciplinary team approach. The multidisciplinary team involvement alongside a prolonged hospital stay helped immensely with the successful management of this case.
Acknowledgement
The authors would like to thank Birmingham City University.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022