Diabetes is an increasingly common long-term condition in children and young people (CYP). People with diabetes who are able to maintain glycaemic control are able to reduce the incidence of complications, comorbidities and death (Herman et al, 2018).
In 2019, there were an estimated 36000 CYP in the UK with diabetes under the age of 19; this was up from 31500 in 2015 (Royal College of Paediatrics and Child Health [RCPCH], 2020).
CYP will very often need to administer extra glucose, check blood glucose levels, or administer extra units of insulin while in school. National guidance in response to the growing number of CYP diagnosed with type 1 diabetes has been implemented over the past 25 years. In 1996, a good practice guide for supporting pupils with medical needs was introduced. The latest version of this guidance, Supporting pupils at school with medical conditions, was published in 2017 (Department for Education, 2017). This guidance recommended that all pupils at school with medical conditions should be properly supported so that they have full access to education, including school trips and physical education.
Quality improvement
A recent quality improvement (QI) programme (RCPCH, 2019) instigated a review of the caseload conducted by our diabetes multidisciplinary team (MDT). This showed that a high proportion of CYP in our care were identified as “red” (HbA1c >100 mmol/mol) or “amber” (>80 mmol/mol) in terms of their diabetes control.
The QI Collaborative supports the MDT by sharing processes and the development of new models of care to improve health outcomes. Furthermore, NICE (2020) guidance advises that CYP with type 1 diabetes should maintain an HbA1c target level of ≤48 mmol/mol (6.5%) to minimise the risk of long-term complications associated with type 1 diabetes. This can be incredibly difficult for most CYP and adults with type 1 diabetes to achieve. NICE stresses that if a CYP has an HbA1c level above the recommended target, professionals should encourage and support the CYP to reduce their HbA1c level, therefore aiming to reduce the risk of long-term complications, such as diabetes retinopathy and nephropathy.
All patients identified as “red” or “amber” were already on a high-HbA1c pathway and had been invited to extra hospital clinics. Despite this, rates of CYP who “were not brought” (WNB) were escalating and clinic demand was increasing. Due to limited clinic space and availability of healthcare professionals, it was increasingly challenging to support some CYP and meet the criteria listed as part of the high-HbA1c pathway. CYP reported concerns about missing school and lack of privacy during hospital consultations, where different professionals are frequently present. Consequently, the service needed to employ an alternative strategy to meet the needs of the CYP and their families.
Aim
Traditionally, CYP with diabetes attend hospital clinics a minimum of four times a year for an MDT review, as stipulated in the introduction of the Paediatric Best Practice Tariff in England assessment criteria. The aim of the Paediatric Best Practice Tariff is to support diabetes clinical services to deliver consistent, high-quality care to CYP with diabetes until the age of 19 years.
Non-attendance of CYP who WNB to clinic had increased in our service and highlighted the need for change. WNB rate impacts on healthcare resources, with clinic slots going unused and additional time invested in contacting patients to reschedule appointments. As a result this can compromise patient care and reduce compliance with National Paediatric Diabetes Audit targets (RCPCH, 2021).
There are multiple factors that can influence clinic non-attendance, including the CYP being reluctant to come to hospital due to the perceived burden of illness and the need for time off school during a critical period, as well as parental factors, such as time off work and practicalities such as parking (Andreou et al, 2015). To address these issues the service developed an innovative clinic model based on taking the MDT clinic out to local schools.
The initiative aimed to identify and address the challenges the school environment poses to CYP with diabetes and provide useful targets and solutions implemented collaboratively by the CYP, guardians, healthcare professionals and the school. A holistic approach was endorsed by all healthcare professionals.
Method
Prior to commencing the 6-month pilot scheme of monthly school diabetes drop-in clinics, verbal and/or written consent was obtained from the CYP, their guardians and the schools. The target age was 11–16 years, attending 22 local secondary schools over five counties. Voluntary sessions were conducted in an identified space within the school to reduce any potential feelings of being “singled out”. The boundaries of confidentiality were communicated and the CYP were aware that anything that was discussed that highlighted risk would need to be escalated. This is an explicit requirement of the Nursing and Midwifery Council (2000) Code of Practice (paragraph 5) and can be found in the ethical codes of all other health professions.
The young person’s voice and engagement were paramount in the sessions. Livesley and Long (2013) advised there is growing evidence that CYP’s subjective interpretations of events may differ significantly from those of adults; yet CYP’s knowledge regarding treatment remain relatively unexplored. The sessions aimed to give the CYP the opportunity to talk to the professional without having guardians listening and potentially interrupting. HbA1c was checked, and glucose meter and insulin pump data were downloaded. Quarterly hospital clinics and nurse-led reviews continued to be offered to all patients.
Results
A high level of attendance to the clinics (87%) was recorded, with only 13% choosing not to attend over the 6-month pilot. Some individuals disclosed that they did not want to attend if clinics were run by certain members of the MDT, so the MDT rotated to accommodate this and attendance increased gradually. WNB rates to hospital clinics declined, CYP reported their anxiety levels had reduced and the MDT achieved the target of seeing patients at least every 6–8 weeks.
It was noted that some patients’ high HbA1c levels (>100 mmol/mol) were not reduced (Figure 1). When reasons for this were explored, there seemed to be a lack of motivation as a result of years of inadequate diabetes management, scantiness of support at home from guardians and escalating mental health issues. Kordonouri et al (2019) suggest that age-related challenges, sociodemographic factors and psychological comorbidities are all barriers to achieving best possible glycaemic outcomes.
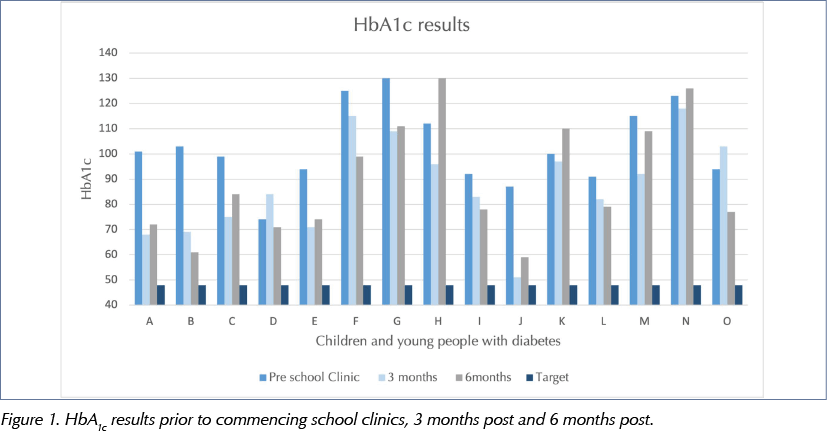
For CYP who were initially in the “amber” group for their high HbA1c levels, reductions in HbA1c were noted (Figure 1) and became closer to the target level of 48 mmol/mol (NICE, 2020). The MDT also reported that more CYP improved their HbA1c level, and a reduction in the overall deterioration of patients’ HbA1c level was seen.
All CYP were asked to complete an anonymous evaluation on their experiences and suggest any areas for improvement. Odiase et al (2020) highlight the importance of reviewing practice and that the impact of a consultation is affected by multiple factors, such as delivery style, communication skills, personality type and connectivity between the CYP and healthcare professional.
Anecdotally, CYP reported that they felt supported in school clinics and that small concerns raised were alleviated before they escalated. Some CYP explained they felt rushed at times, so school clinic slots were increased to make more time available for them. Knowledge gaps and “learned habits”, for example missing blood test readings, omitting insulin doses and forgetting to monitor ketones when blood glucose results are above 14 mmol/L, were discovered and appropriate guidance and teaching were given. Emotional difficulties were identified and addressed with referrals to peer support and school counselling services.
Lifestyle challenges associated with family dynamics and academic performance not previously known to the team were also shared by the CYP and school, including suboptimal school attendance, bullying, self-harm or high-risk behaviours. In these cases, supplementary referrals to the team’s clinical psychologist were made. An increase in engagement of CYP in self-management of their diabetes was observed by the school. Unfortunately, however, it was noted that some CYP still felt unmotivated to self-manage their diabetes and therefore did not improve their management or reduce their HbA1c level.
In a small sample of CYP included in the pilot, it appeared that the areas of most concern were hypoglycaemic episodes and suboptimal dietary habits. The opportunity to deliver dietary guidance in the school canteen was a great benefit as CYP gained confidence in healthy eating and carbohydrate counting. King (2015) suggested that for CYP with type 1 diabetes, being able to accurately calculate the amount of carbohydrate in something they are going to eat is essential for the effective management of their blood glucose levels. Once they can confidently calculate carbohydrates, they have much more freedom to eat what they want, when they want.
The school clinics gave the MDT the opportunity to stress the importance directly to the school staff in allowing the CYP the time and resources required to successfully complete this task. CYP explained that they felt more prepared for transition to the young persons’ clinic and had the opportunity to discuss sensitive topics, including sex, alcohol, smoking and drugs, without having guardians present. Thynne et al (2014) explained the journey of a young person with type 1 diabetes is laden with challenges, especially during the transition from paediatric to adult services. It is the responsibility of healthcare professionals to ensure that the journey is as smooth as possible.
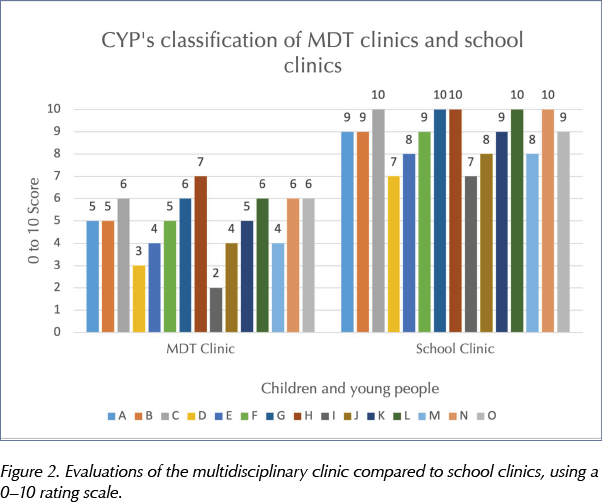
Results from the evaluations (see Figure 2) showed that CYP often associated hospital appointments with negative experiences, due to guardians taking control of their consultations. Furthermore, some CYP reported feeling that a reduction in HbA1c was the main priority of the hospital appointments.
Discussion
This pilot showed that school clinics improved clinical contact and liberated scarce clinic slots, highlighting that extra hospital appointments may not always be a suitable approach to all CYP with challenging glycaemic control. It highlighted a need to improve our existing hospital clinics through actively defining parental roles during clinics, as well as prioritising patients’ views and improving our counselling skills to facilitate a young person’s engagement in self-care.
Psychological wellbeing is an essential component of long-term condition self-management, and psychological support is increasingly recognised as an essential component of effective long-term condition healthcare (Day, 2020).
The provision of education by the healthcare professional provides CYP with valuable tools that will support and develop their self-management skills and overall diabetes control (Christie and Khatun, 2020). The diabetes drop-in clinics improved communication and partnership with schools, enabling individual healthcare plans (IHCPs) to be more effectively implemented. The IHCP is a written agreement that details exactly what care CYP need in school, including when the care is needed and who will provide the care. It is drawn up with input from the CYP, their guardian, their specialist nurse or dietitian and relevant school staff (Singleton, 2015).
The East of England Paediatric Diabetes Network recognised the importance of working together with a common protocol to enhance care in schools (Waldron and Campbell, 2014). It was clearly evident that CYP with diabetes had previously received mixed support in the management of their condition while at school.
Lehmkuhl and Nabors’ (2008) pilot study found that children who reported greater satisfaction with school support had lower HbA1c (Hayes et al, 2017). Challenges that were identified were associated with a lack of understanding from the school staff. Particular areas of concern included finding appropriate private places for injections and checking blood glucose levels, taking snacks, and the ability of school staff to recognise hypoglycaemic and hyperglycaemic episodes. Under the 2014 Children and Families Act, schools have a duty to support children with medical conditions (Thornton, 2017). Additionally, NICE (2020) guidance, as well as International Society for Pediatric and Adolescent Diabetes (ISPAD, 2018) guidance and the Diabetes Quality programme (RCPCH, 2019) all recognise the importance of school training. School diabetes education is a key part of our role as diabetes healthcare professionals. Additionally, ISPAD (2018) guidelines recommend that:
“Optimal management of diabetes at school is a prerequisite for optimal school performance, including learning and for the avoidance of diabetes-related complications.”
Therefore, there should be emphasis on healthcare professionals educating school staff about all aspects of diabetes, including the signs and effects of hyperglycaemic and hypoglycaemia, the life-threatening consequences of lack of intervention and the urgency of treatment to prevent diabetic ketoacidosis.
The MDT adapted our school education as part of this QI pilot programme, in particular focusing on the symptoms and signs individual CYP may have when they are experiencing a hypoglycaemic or hyperglycaemic episode. This was essential to avoid situations that had been previously experienced by CYP in the school setting. It provided the opportunity to involve all teachers that have contact with the pupil rather than just the school’s medical team. The pilot was also important in encouraging the schools to provide a private area for each pupil to administer their insulin, check blood glucose levels and eat snacks and be supported throughout their time in school with their diabetes. Moreover, the importance of not discriminating against the CYP and offering all the same opportunities as their peers was a key point communicated and offering extra training for residential and day trips.
The drop-in clinics gave the MDT the opportunity to discuss directly with the schools their responsibility to the CYP and the guidance from Department for Education (2017), and the funding challenges associated with IHCPs.
To further extend the support to CYP in schools, a key factor may be the involvement of social networks during a school or diabetes nurse visit. With individual consent, this would help peers to have an understanding of the CYP with diabetes and the daily challenges that they can face, giving them an opportunity to explore and empathise.
A suggestion for further research in this area would be to look at the duration of the high HbA1c levels in those in the amber and red groups, and to determine the benefits of the school clinics in these groups.
Conclusion
The unintended benefits of this QI initiative to pilot school drop-in clinics were facilitating engagement to improve self-management and improved healthcare for CYP with type 1 diabetes. Diabetes drop-in clinics were a useful platform to begin an effective transition to young adult diabetes services. The information shared challenged the MDT to look critically at the traditional model of care for the CYP. The introduction of a transition specialist nurse was also supported by our findings.
All schools adapted to the school clinics, and anecdotal evidence suggested they appreciated having a professional to support the challenges regarding funding, resources and increase in child and adolescent mental health (CAMHS). Where required, CAMHS and Early Help referrals were supported, alongside signposting to other agencies.
The MDT recognised the positive impact for the young people, schools, guardians, as well as the MDT, and endorsed the continuation of the monthly school drop-in clinics.
Acknowledgement
The author would like to thank the paediatric diabetes multidisciplinary team at North West Anglia NHS Foundation Trust & Birmingham City University, LBR7587 Collaborative Children and Young People’s Diabetes Care Module and course leaders.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022