Since the emergence of COVID-19 in the UK, social distancing and restrictions on face-to-face contact have led to the utilisation of alternative communication methods. The use of technology in the care of people with diabetes has rapidly increased, largely replacing traditional face-to-face consultations in order to free up space and capacity in acute hospitals, enable remote working and reduce the risk of infection transmission in NHS settings (Nuffield Trust, 2020).
Background
In November 2020, guidance for secondary care outlined that remote consultations were recommended, if appropriate (NICE, 2020). More specifically, it was recommended that remote consultations should be used for check-ups for people with long-term conditions, especially if the person is stable and has monitoring devices at home (NICE, 2020). This description can be used to classify young adults with diabetes (aged 18–25 years old).
Research prior to COVID-19 has shown encouraging benefits of virtual consultations in people with long-term conditions (Mallow et al, 2016). Despite this, the transition from the traditional face-to-face appointments to online and telephone consultations that took place during the pandemic was very rapid. With it being a relatively recent transition, there is limited research on the effects of this drastic change on the quality of care, patient satisfaction and clinical practice.
Technology paradox
Research has shown that young adults with type 1 diabetes experience challenges with engagement to healthcare services (Hamilton et al, 2002) and this is associated with suboptimal glycaemic control and health outcomes. Additionally, evidence exists of a “technology paradox” in young people with diabetes, where the use of routine technology (internet, social media, smart phones and tablets) is high, but the use of wearable diabetes technology (insulin pumps and continuous glucose monitors) is low (Hinshaw and Basu, 2015; Foster et al, 2019). Furthermore, research on virtual consultations (online and telephone) in young adults with diabetes is scarce, with mixed results.
This qualitative research study was conducted following the recent changes in the way care is delivered to young adults with diabetes in response to the spread of COVID-19. It is hoped that this will assist in gaining a wider understanding of the consultation preferences of this population, and how they are responding to the shift from in-person contact to remote, technological consultations with their specialist clinicians.
Aims
The aim of this study was to determine which consultation style (face-to-face, online or telephone) young adults with diabetes prefer, and the factors influencing their preference.
Methods
In May 2021, the records of all young adults with diabetes under the Royal Liverpool University Hospital were obtained. These included 176 people, of whom 60 were randomly selected (36 males and 24 females) to participate in a short telephone survey at the end of their clinic consultation.
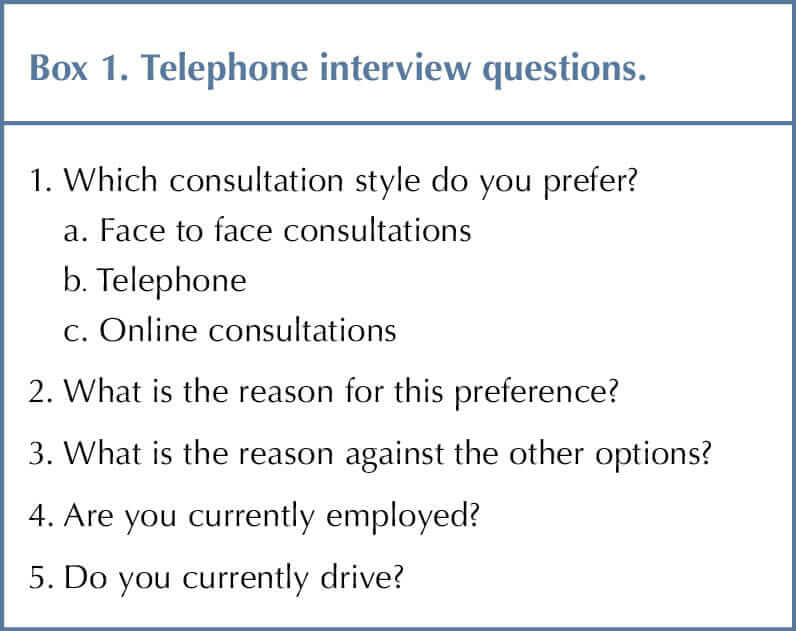
To meet the inclusion criteria, participants had to be young adults (aged 18–25 years old) and under the care of the Young Adult Diabetes Service at the Royal Liverpool University Hospital. Further data regarding the duration of diabetes was obtained via the online clinic register, and was calculated in months. The young person’s most recent HbA1c (mmol/mol) was retrieved using the hospital laboratory via Integrated Clinical Environment (ICE). The questionnaire consisted of a single multiple-choice question, and open-ended and closed-ended questions (Box 1).
Data analysis
The data was collated and analysed, and interview responses about the reasons for and against each of the consultation styles were coded into themes. For statistical significance, a Chi-square test was performed to test the relationship between gender and consultation style preference, HbA1c and consultation style preference, employment status and consultation style preference, and driving status and consultation style preference. The statistical significance level was set at P <0.05.
Results
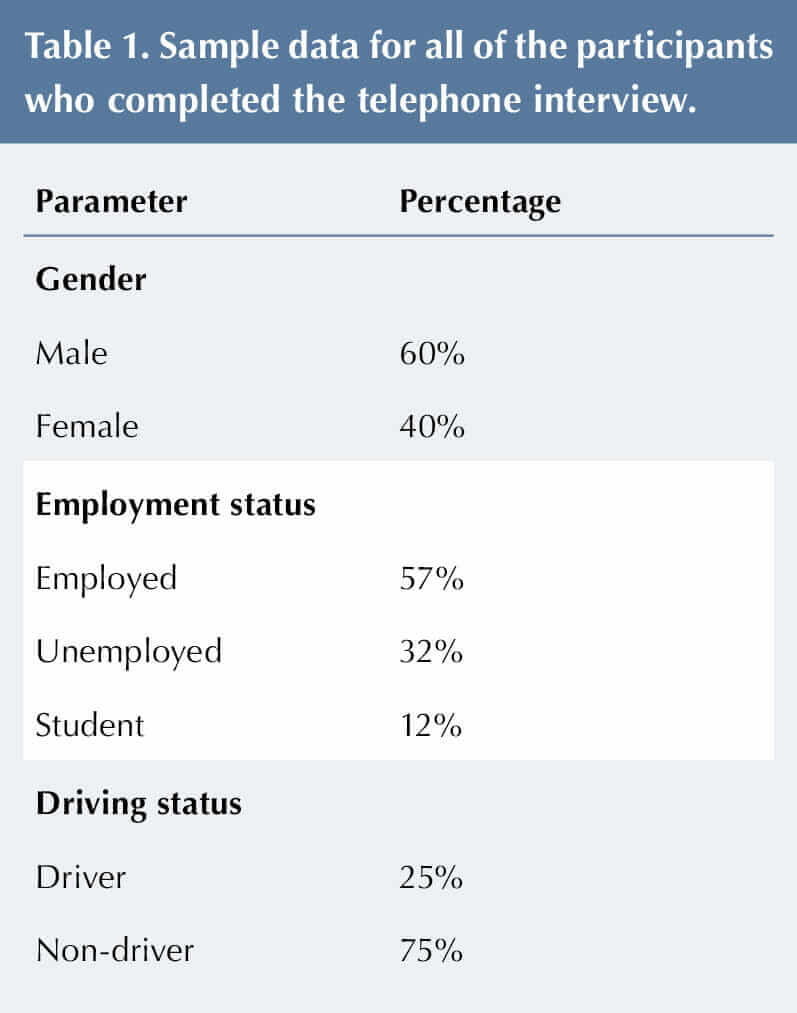
A response rate of 100% (n = 60/60) was achieved for the telephone interviews. The demographics of these participants can be seen in Table 1.
Consultation preference
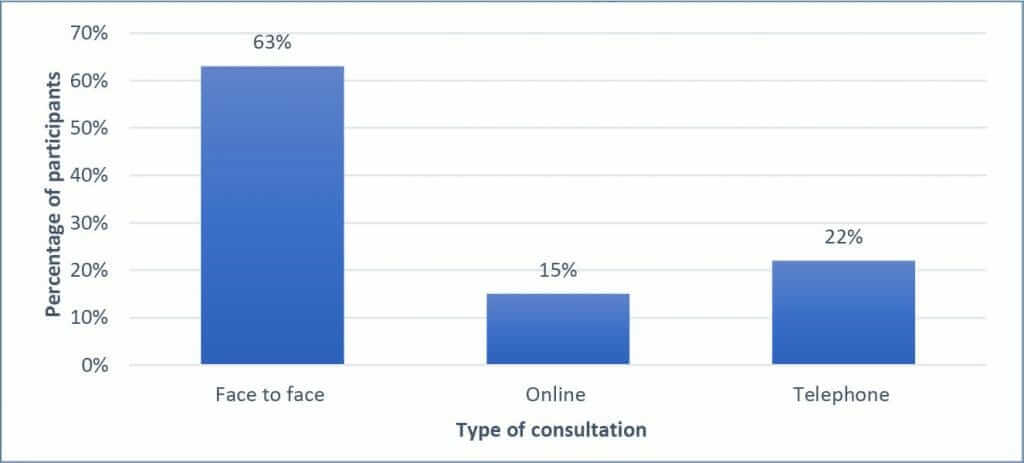
Of the 60 participants, 63% preferred face-to-face consultations, 15% favoured online consultations and 22% preferred telephone consultations (see Figure 1).
Gender and consultation preference
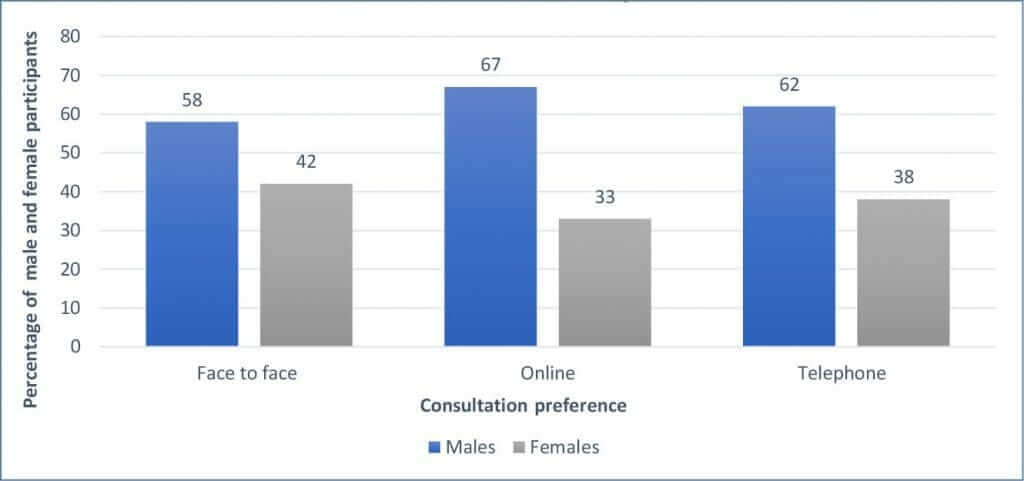
Of the participants who preferred face-to-face consultations, 58% were male and 42% were female. In those who preferred online consultations, 67% were male and 33% were female, while those who preferred telephone consultations, 62% were male and 38% were female. There was no statistically significant association between gender and consultation preference (P=0.88; Figure 2).
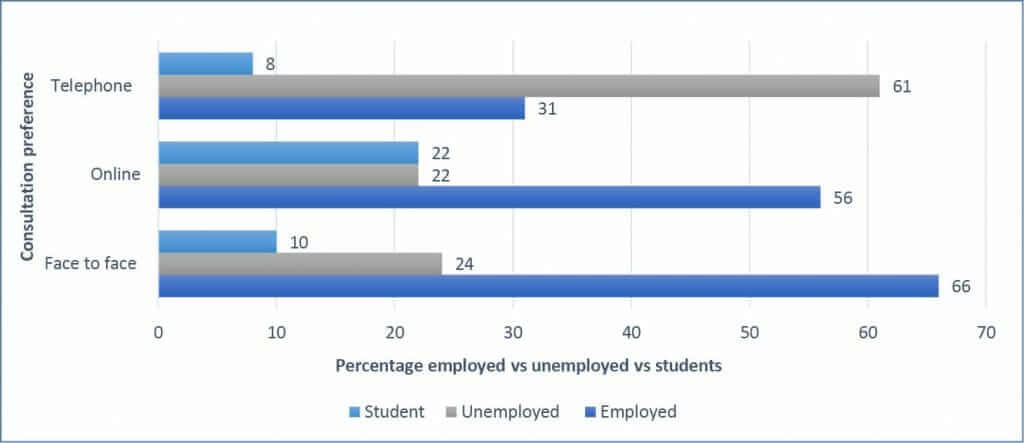
Employment status and consultation preference
Of the young people who preferred face-to-face consultations, 66% were employed, 24% unemployed and 10% were students, while those favoured online consultations, 56% were employed, 22% were unemployed and 22% were students.
For participants who preferred telephone consultations, 31% were employed, 61% were unemployed and 8% were students (Figure 3). There was no statistically significant association between employment status and consultation preference (P=0.97; Figure 3).
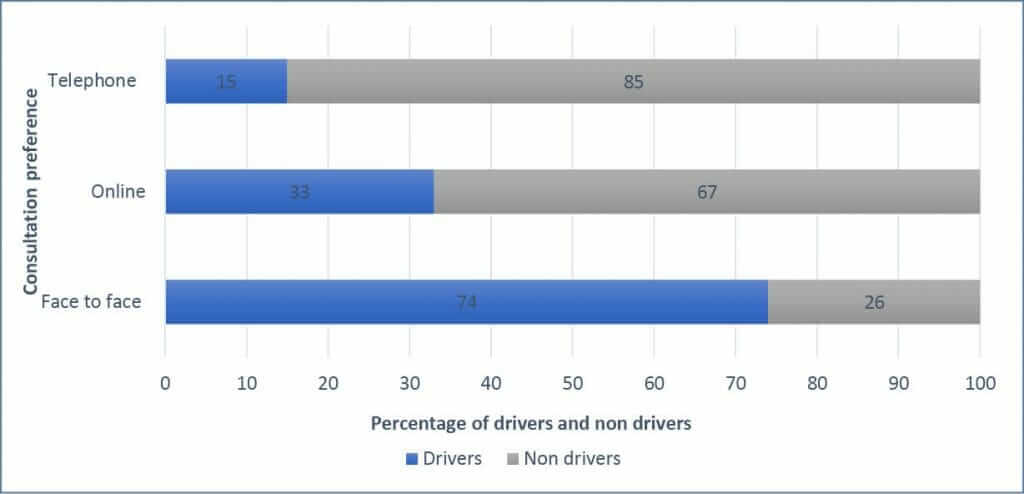
Driving status and consultation preference
Out of those participants who preferred face-to-face consultations, 74% were drivers and 24% did not drive, while of those who preferred online consultations, 33% were drivers and 67% did not drive. In the young people who favoured telephone consultations, 15% were drivers and 85% did not drive. There again was no significant difference between driving status and consultation preference (P=0.88; Figure 4).
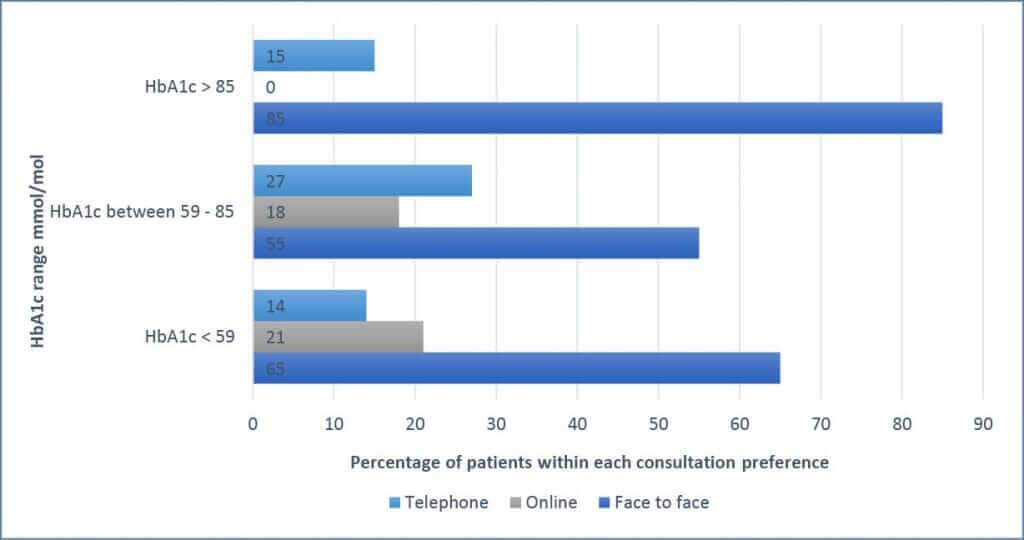
HbA1c and consultation preference
The most recent HbA1c level was recorded for each participant. This data was stratified into three HbA1c groups (≤58 mmol/mol [7.5%], 59–85 mmol/mol [7.5–9.9%], ≥86 mmol/mol [10%]) and the percentage of participants who preferred each consultation style was calculated for each HbA1c group.
Face-to-face consultations were overwhelmingly preferred in all 3 groups (65%, 55% and 85%, respectively; Figure 5).
Median age and duration of diabetes
The median age was 24 years for those preferring face-to-face consultations and 23 years for those preferring online and telephone consultations.
The median duration of diabetes was 131 months (11 years) for face to face, 88 months (7.3 months) for online and 112 months (9.3 years) for telephone consultations.
Reasons for and against consultation style preferences
Themes identified indicating preference for face-to-face consultation included:
- Ease with communication.
- Comfort.
Meeting the healthcare professionals.
For online and telephone consultations, reasons included:
- Convenience.
- Not needing to travel.
Anxiety around transmission of COVID-19.
The reasons cited against face-to-face consultations mirrored preferences for online and telephone consultations. The reasons against telephone and online consultations, however, included:
- Being uncomfortable on video.
- Impersonal consultations.
- Forgetting to highlight important issues.
- Poor internet and technology access.
Discussion
Young adults with diabetes face several challenges with their condition, which can impact on self-management (Hamilton and Daneman, 2002; Foster et al, 2019). While this is multifactorial, regular follow up with specialist services plays a pivotal role in ensuring good management of type 1 diabetes (Kunasegaren et al, 2018).
Our study found that 63% of the young adults with diabetes preferred face-to-face consultations compared with online or telephone consultations. Participants expressed the main reason for this as being the ease of communication and the ability to raise concerns during in-person consultations. This finding echoes previous research, which highlights that face-to-face consultations allow patients to discuss more problems. Participants also felt “more comfortable” in an in-person setting, perhaps because of being used to the professional hospital clinic environment when discussing their condition. This notion of consultations feeling “foreign” was mentioned three times when describing online consultations.
Participants also raised the issue that face-to-face consultations make it easier to download glucometer and insulin pump data, perhaps due to the fact that they do not have access to appropriate technology to do this at home. This is also compounded by the fact that the clinic is surrounded by one the most deprived areas in the UK (Liverpool City Council, 2020).
The main reason participants disliked face-to-face consultations was that they required travelling a long distance. Equivalently, the lack of travel needed to attend consultations was the most common reason participants preferred online and telephone consultations. This correlated with the driving status of the participants, with virtual consultations being preferred over in-person among non-drivers.
The least preferred consultation style was online consultations, and this study found that only 15% of participants preferred online consultations over telephone and face-to-face consultations. Being “uncomfortable” on video was the most common reason cited by the participants in this study. This mirrors previous research showing that this format is preferred less among young people (Hammersley et al, 2019). Participant’s preferred telephone consultations second to face-to-face consultations. Apart from the convenience among non-drivers, a lack of camera also contributed to the preference over online consultations.
In this study, 66% of the participants who preferred face-to-face consultations were employed. It could, therefore, be hypothesised that in-person appointments are easier to prioritise when working, with it being easier to schedule time off for an in-person consultation. It may be that employers are more likely to grant time off for a face-to-face appointment that requires travel than for a virtual or telephone appointment, which can be scheduled during a break.
While all participants preferred in-person consultations, regardless of HbA1c level, there was a predominant preference for them among those with levels >85 mmol/mol (10%).
Limitations
This study is small, observational with qualitative features, limited to young adults with diabetes at a tertiary care hospital, with no comparator group. The authors acknowledge, therefore, that the study may not accurately represent young adults with diabetes across the country. With a median age of 24 years, many of the participants had gone past the “transition years” between paediatric and adult care by a few years. As a result, the study did not capture the impact of challenges of transition between services.
Conclusion
The results of this study are not statistically significant, but represent the perception of young people with different consultation styles during a pandemic. There is a general preference for the face-to-face style of consultation, with virtual consultations being preferred among non-drivers and unemployed young adults. While anxiety around attending in-person consultations remains due to the pandemic, there is also a need to adopt a person-centred approach in offering clinic appointments to young adults with diabetes.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022