Recent research has identified an increase in the number of children diagnosed with type 1 diabetes following COVID-19 infections (Barrett et al, 2022). Along with an increasing number of children diagnosed, there has also been technological advancements to help manage the disease for these children. While mobile and wearable devices have been crucial in the tighter management of blood glucose levels, there has been concern about the effects of these tools on the child’s caregivers (Shivers et al, 2013). The current research seeks to explore the effects of continuous glucose monitoring (CGM) on parents and caregivers of children with type 1 diabetes.
COVID-19 virus
Recent research has shown that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can infect and replicate inside the beta cells responsible for insulin production (Müller et al, 2021). Further evidence shows that the virus can alter the function of the pancreatic tissue, or the islets, that contain the beta cells. Both mechanisms of action decrease the body’s ability to effectively secrete insulin (Tang et al, 2021; Wu et al, 2021).
Continuous glucose monitoring
Due to recent technological advancements, it is possible to know the blood glucose level of a child on a continual basis through the utilisation of CGM. These devices can result in more desirable HbA1c results and decrease the number of emergencies related to diabetic conditions. These devices require the child to wear a small sensor on their skin that transmits information to a receiver or other cellular device. Some versions of the CGM systems allow a reading to be remotely sent to a parent or caregiver on a continuous basis.
Alarm fatigue and sleep deprivation
Parents or caregivers who receive continuous glucose readings can set alarms for a wide variety of conditions to alert them to take action. For example, a parent can be alerted to a low blood glucose level so that they can provide the child with quick-acting carbohydrates. Similarly, when alerted to a high blood glucose, a parent can administer insulin. Other options, in addition to those alerting that a child is out of the desired blood glucose range, include rapid fall and rapid increase in blood glucose levels, as well as “no data” alarms.
The continuous nature of the monitor allows parents and caregivers to be alerted by the monitor 24 hours a day, including throughout the night. Parents and caregivers can be awakened many times during the night to administer insulin or provide carbohydrates for repeat low blood glucose readings. This disruption in sleep can have a negative impact not only on the parent, but also the child. Administering insulin incorrectly can have very serious consequences, including death, and often requires mathematical calculations. Caregivers who are suffering from sleep deprivation could be more likely to make an error in calculating the appropriate dosage of insulin. Additionally, the caregiver who is suffering from continual sleep disruption may experience unwanted undesirable mental and physical health outcomes (Hanson & Huecker, 2021).
The average number of times a parent or caregiver is alerted by CGM is not known. Research has shown that individuals who utilise CGM check their device an average of 15 times a day, but can be up to 48 times per day or every half hour (Aleppo, 2018). It is thought that in children with diabetes, there is an increase in the number of CGM checks and alarms due to the fluctuations in blood glucose often experienced during times of growth and activity. Additionally, there could be an increased need to monitor glucose levels in younger, non-verbal children who are unable to recognise or report symptoms of hyper- or hypoglycaemia.
Aims
The increased use of technology is allowing for the tighter control of blood glucose levels in the paediatric population with type 1 diabetes, but it also may have negative effects on the caregivers who receive multiple alarms throughout the day and night. It is theorised that the multiple alarms that occur 24 hours a day can have a negative impact on the quality and quantity of sleep in a caregiver and result in “alarm fatigue”. Unfortunately, there is a paucity of data in the literature regarding these two topics. This study aimed to determine the sleep quality and quantity and the prevalence of alarm fatigue in parents and caregivers of children with type 1 diabetes using CGM.
Method
This study used an anonymous electronic survey of parents and caregivers. They were asked to self-report data related to sleep quality and alarm fatigue. No identifying information was collected as part of the study. Institutional Review Board approval from Sacred Heart University, Connecticut, USA was obtained prior to data collection.
Sample and data collection
A convenience sample of parents and caregivers was established and data collection was conducted via an online survey. An initial post with the link to the survey was made on several Facebook support groups for parents and caregivers for children with type 1 diabetes. Participants were invited to share the survey with others who met the criteria for inclusion in the study. The study remained open for approximately two weeks.
Tools
The online survey tool consisted of three sections. The first section focused on demographics, including variables such as age, race and education. The second section focused on alarm fatigue. No tool was found in the literature that measures alarm fatigue in this population, therefore, a tool that measures alarm fatigue in nurses in the acute care setting was adapted for use. Face validity of the tool was determined by interviewing a focus group of current parents and caregivers of children using CGM. The tool contains 10 questions that ask the respondent to state how often they agree with the statement using a five-point Likert scale.
The third section of the survey was the Pittsburgh Sleep Quality Index (PSQI; Buysse et al, 1989). The PSQI examines sleep quality over a 1-month time frame. The tool consists of 19 self-report items, which combine to form seven components. Each component is measured on a 0–3 scale with 0 being the best outcome and 3 being the worst outcome. These seven components then allow for the calculation of one overall score. Validity and reliability of the Pittsburgh Sleep Quality Index (PSQI) has been well established in the literature.
Data analysis
Data analysis was completed using SPSS 10.0 for PC. Frequencies and means were calculated for demographics and the Alarm Fatigue Scale. The PSQI was analysed in accordance with the methodology described in the original paper publication (Buysse et al, 1989).
Results
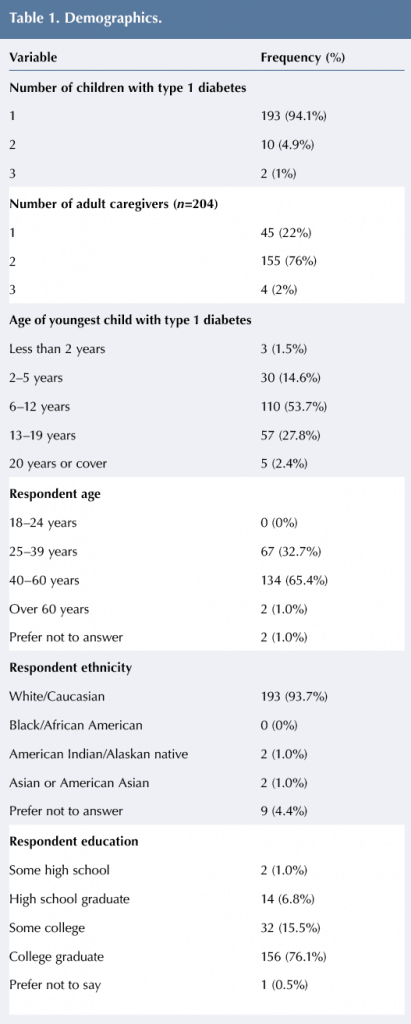
A total of 205 individuals completed at least one section of the study. Most respondents had only one child with type 1 diabetes (94.1%) and two caregivers in the house (75.6%). A little over 50% of the participants stated that their youngest child with type 1 diabetes was 5–12 years old and approximately 65% of the participants were 40–60 years old. The majority of the respondents were white or Caucasian (93.7%) with a college education (76.1%). See Table 1 for additional information about demographics of the population.
Alarm fatigue
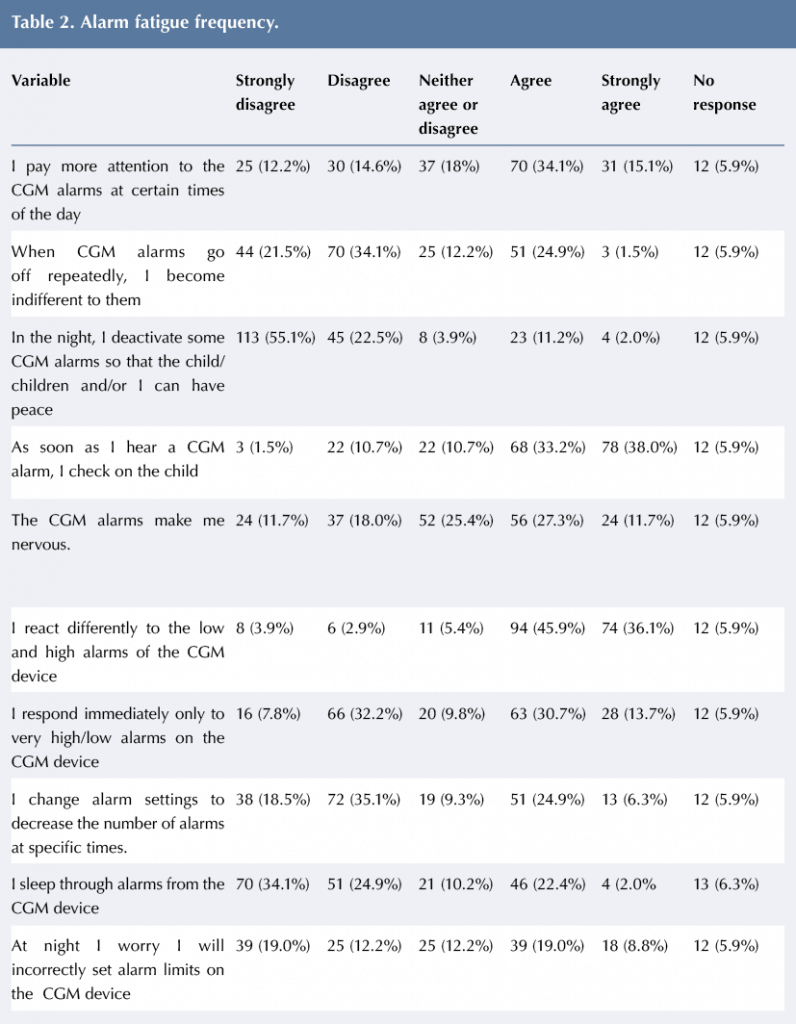
Results of the Alarm Fatigue Scale are presented in Table 2. Nearly half of the participants agreed or strongly agreed that they paid more attention to the CGM alarms at certain times of the day. Additionally, about a quarter of respondents stated that when the CGM alarms go off repeatedly, they become indifferent to the alarm. Approximately 75% of caregivers strongly disagreed or disagreed that they deactivate some CGM alarms so that the child/children and/or parent/caregiver can have uninterrupted sleep at night. Most participants (about 70%) reported that they agreed or strongly agreed that they checked on the child as soon as they heard the alarm go off.
About 40% of the caregivers also agreed or strongly agreed that the CGM alarms make them nervous. When asked about responding immediately, approximately 44% agreed or strongly agreed that they respond immediately only to very high/low alarms on the monitor. Additionally, about a third of caregivers agreed or strongly agreed that they change alarm settings to decrease the number of alarms at specific times.
When asked if caregivers worry they will incorrectly set alarm limits on the CGM device at night, almost 30% agreed or strongly agreed.
Sleep deprivation
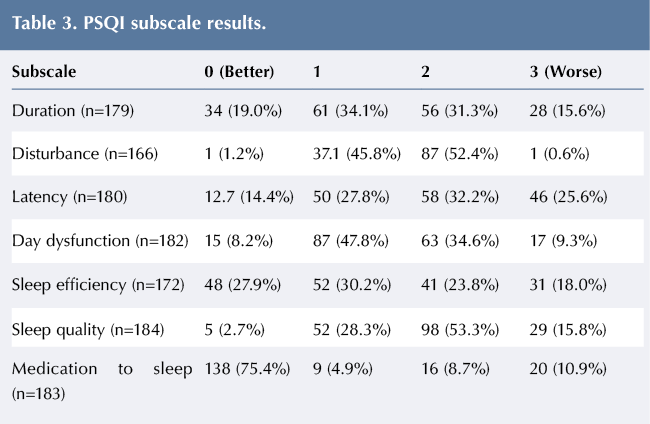
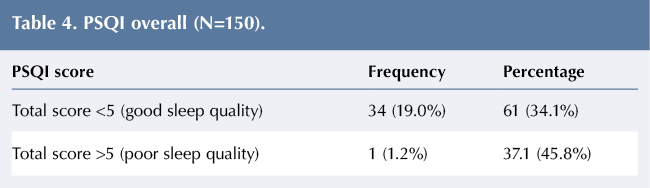
Results of the seven subscales of the PSQI are presented in Table 3. Utilising the 0–3 scale, with 0 being the best and 3 being the worst, over 50% of the respondents scored a 2 or 3 on the sleep disturbance subscale. Over a quarter of the caregivers scored a 3 on sleep latency. In regards to day dysfunction, over 90% of participants received a score of 1–3 on the subscale. With regards to sleep quality, which asks participants to describe their sleep from very good to very bad, approximately 70% reported their quality of sleep as fairly bad or very bad. Over 75% of participants reported that they have not taken any medication to assist with sleeping in the past month. The seven subscales are combined for one overall score to rate sleep quality for participants, which is presented in Table 4. As seen in the table, nearly 89% of respondents had a score of ≥5, which is associated with poor sleep quality.
Discussion
Results of this study showed that sleep deprivation and alarm fatigue are a significant concern for parents and caregivers of children with type 1 diabetes using CGM. Approximately 25% of caregivers responded that they become indifferent to alarms when the CGM alarms go off repeatedly. This fatigue from alarms could result in poor outcomes for the child. About 40% of the respondents also reported that the CGM device makes them nervous. Continued anxiety in the caregivers could result in disruption in sleep and have negative effects on mental and physical health (Kubzansky et al, 1998; Staner, 2003). The scores of the PSQI show significant dysfunction in sleep quality, resulting in reported dysfunction in daily life.
One of the most alarming findings of the study was that almost 70% of the caregivers surveyed stated their sleep quality was fairly bad or very bad. A sufficient amount of sleep is vital to good physical and mental health (Ferrara and De Gennaro, 2001). For the individuals in this study, roughly 20% reported problems staying awake while driving, eating meals or engaging in social activity at least once or twice a week. These exhausted caregivers provide a very precise level of care to children while often maintaining full-time jobs. Therefore, it is not surprising that over 60% of the caregivers in the study reported that it was somewhat, or a very big problem, for them to keep up enough maintain enthusiasm to get things done.
Providers should be aware that the caregivers of their patients may be experiencing significant disruptions in sleep and quality of daily life. Parents and caregivers should be provided with resources to help cope with the significant impacts on daily life that occur. Resources might include assistance identifying and obtaining peer and respite support along with mental health services for the parents and caregivers.
Furthermore, this may have implications for disability benefits that are available for children with type 1 diabetes.
Limitations
One major limitation of this study is the use of self-report data from support groups. Individuals who take the time to respond to the survey and/or to be a part of a support group may be more likely to experience difficulties than those who did not respond. Additionally, it is noted that there was a significant lack of diversity in the sample. Due to the anonymous nature of the study and the use of a convenience sample, the findings cannot be generalised to specific populations.
Conclusion
In conclusion, there is a need for supporting parents and caregivers of children with type 1 diabetes. This research has shown that these caregivers experience a significant decrease in quality of sleep, suffer from the resulting disruptions in quality of life, and experience alarm fatigue from the use of CGM devices. These monitors are vital to the management of blood glucose levels in children, however the health and quality of life of the caregiver must be considered as well.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022