Diabetic ketoacidosis (DKA) affects more than 40% of people with newly diagnosed type I diabetics and acute kidney injury (AKI) is one of its recognised complications. Together the insulin deficiency and reduced kidney function can create a multitude of complex and life-threatening electrolyte abnormalities that can be difficult to manage.
This case report discusses a young girl who developed DKA as the first presentation of type 1 diabetes and was subsequently diagnosed with AKI requiring haemodialysis. This case also highlights the importance of a multidisciplinary team approach when it comes to managing complicated DKA patients and the need to minimise further episodes of AKI to reduce the risk of long-term chronic kidney disease (CKD).
DKA stems from insulin deficiency along with an excess of counter-regulatory hormones and is the most feared complication of type 1 diabetes (Fan et al, 2021). AKI occurs in 40–50% of people hospitalised with severe DKA and is a well-known complication that often responds very well to the timely management of DKA (Hoste et al, 2015). By definition, AKI is characterised by a sudden deterioration of renal function usually accompanied by a decrease in the urine output. This leads to complex electrolyte and acid-base disorders and also an increased incidence of micro- and macrovascular complications of diabetes in later life (Orban et al, 2014). The most frequent cause of AKI in DKA is renal ischemia/reperfusion injury, which predominantly results from dehydration induced by hyperglycaemia (Fan et al, 2021).
Case report
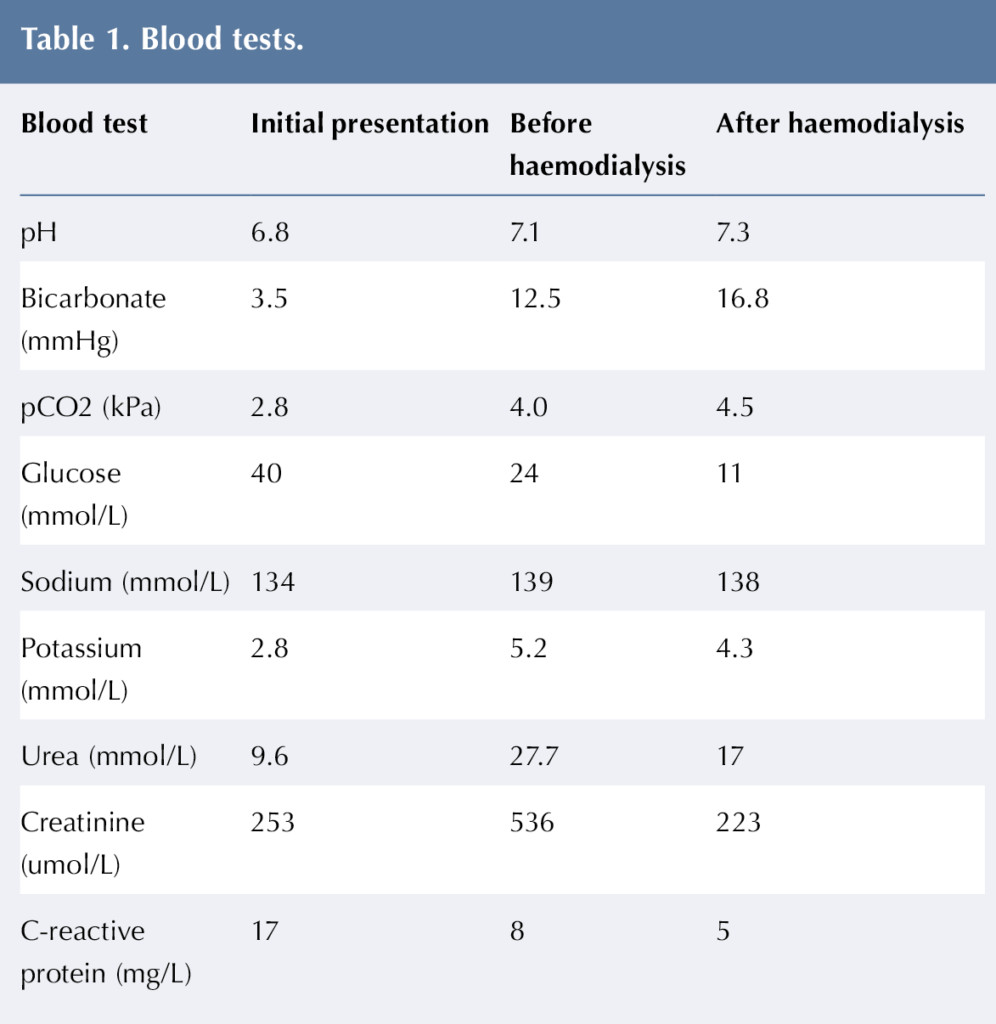
An 11-year-old girl was brought to the paediatric emergency department due to increased work of breathing for 4 hours, followed by loss of consciousness at home. The girl had a history of lethargy, polyuria and polydipsia for the past three months. When brought to the emergency department she had tachycardia, hypotension, dry mucous membranes and cold peripheries. She had a Glasgow Coma Scale (Teasdale and Jennett, 1974) of 8/15 and she was unable to maintain her airway, so she was intubated and ventilated. Her blood glucose level was high and she was diagnosed and subsequently managed as severe DKA with shock. The initial capillary blood gas done in the emergency department showed a pH of 6.8, a bicarbonate of 3.5 mmHg and a blood glucose of 40 mmol/L. As per the guidelines of DKA management, bloods were performed and were markedly abnormal (Table 1). From her clinical presentation and biochemical markers, a diagnosis of sepsis and AKI was considered alongside severe DKA.
Management
Since the girl was intubated and ventilated, discussions were initiated to transfer her to tertiary centre for further management. She received two boluses of normal saline, which was followed by an improvement in her heart rate and blood pressure. The girl was started on the DKA protocol as per the British Society of Paediatric Endocrinology and Diabetes guidelines. She was catheterised with strict input/output, blood gas, blood glucose and ketone monitoring. The parents were kept informed about her clinical condition and the need for specialist intervention. Her clinical condition was also discussed with the paediatric nephrology team at the tertiary hospital. After initial resuscitation and start of antibiotics and DKA protocol, the girl was transferred to the tertiary centre in-view of her clinical condition and the need for ventilatory support.
At the tertiary centre further bloods were taken after 2 hours of starting treatment with insulin and they showed further worsening of the urea and creatinine. At this moment she had anuria and was hypertensive. After discussions with the paediatric endocrine and nephrology teams, the girl was started on haemodialysis via a haemodialysis central line passed into the left femoral vein. The girl received two sessions of haemodialysis, which was followed by improvement in urea, creatinine and electrolytes. This ultimately lead to an improvement in conscious level and clinical condition of the patient. Her hypertension was managed with amlodipine and the dose was titrated according to the blood pressure measurements done subsequently. The girl showed full renal recovery in terms of correction of urea and creatinine back to baseline in about 10 days. She was continued on amlodipine for hypertension for a period of 6 weeks and this was discontinued after follow-up with the nephrology team.
Classification of AKI
According to KDIGO (Kidney Disease: Improving Global Outcomes) guidelines (KDIGO, 2021), AKI is defined as serum creatinine greater than 1.5 times the baseline creatinine levels. AKI can be classified on the basis of a rise in estimated baseline creatinine (EBC). According to this classification, stage 0 AKI is a creatinine level <1.5 times the EBC, stage 1 AKI is creatinine level 1.5 to 2 times the EBC, stage 2 AKI is a creatinine level 2 to 3 times the EBC, and stage 3 AKI is a creatinine level >3 times the EBC (KDIGO, 2021). It was found that people with stage 2–3 AKI had a greater mortality as compared to individuals with milder AKI. Also, the recovery time from metabolic acidosis is longer in children with greater severity of AKI (Fan et al, 2021).
Incidence of AKI in DKA
The incidence of AKI is about 41.2–54.8% in people hospitalised with DKA (Chen et al, 2020a). The incidence is greater in children with known type 1 diabetes, compared to those who have DKA as a first presentation of type 1 diabetes (Hursh et al, 2017).
Pathophysiology of AKI
The mechanism of injury in most cases is pre-renal, but renal tubular injury has also been documented in a few children with DKA and severe AKI. Such patients further have a reduced ability to compensate for metabolic acidosis because of reduced renal function (Chen et al, 2020b).
Management of AKI in DKA
The management of AKI in severe DKA is essentially conservative to begin with. It depends on the severity of DKA and also the improvement in clinical condition and biochemical markers seen within a few hours of starting treatment for DKA. Only a small percentage of people with decreasing urine output and worsening clinical condition and biochemical markers are going to require haemodialysis (Myers et al, 2020).
In a study involving 165 DKA patients, only 102 patients developed AKI and out of these only two people with severe DKA required haemodialysis. None of the patients required renal replacement therapy on a long-term basis (Hursh et al, 2017).
In the majority of cases the AKI will resolve spontaneously as the dehydration is corrected with fluids and insulin infusion. A small proportion of patients, however, will still require specialist intervention including haemodialysis for the management of fluid overload and electrolyte abnormalities. The response to treatment is fairly quick, with most children (approximately 80%) recovering from metabolic acidosis on the first day of treatment (Kashani et al ,2016).
There are significant long-term complications associated with AKI in DKA. Episodes of AKI during DKA in children with diabetes were found to be associated with increased risk of developing microalbuminuria and rapid progressive CKD (Huang et al, 2022).
Multidisciplinary team approach
In view of the nature of DKA presentation for this young girl and the accompanying AKI, she was managed with the involvement of a multidisciplinary team including a paediatric endocrinologist, paediatric nephrologist, general paediatrician and the diabetes specialist nurse. The paediatric radiologist was involved as well in order to look for underlying kidney and urinary tract abnormalities that may have precipitated the AKI, although none was identified. The girl remained on amlodipine for the treatment of hypertension for about 4 weeks and this was gradually tapered once the blood pressure had normalised on serial measurements.
Conclusion
AKI is one of the well-known complications of DKA that needs to be anticipated especially in individuals presenting in shock with severe DKA. The management may be conservative in most cases, but does require collaboration with the paediatric nephrology team. AKI in DKA is associated with increased risk of long-term kidney sequelae. Therefore, it is important to minimise recurrence of DKA and minimise chances of AKI in any person with diabetes.
This girl also had a complex social background, which resulted in a delayed presentation, a prolonged hospital stay and a multidisciplinary team meeting before discharge. During this time, she was continuously observed for any further complications and the family was given satisfactory education before discharge.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022