Historically, diabetes care in Ireland was delivered in secondary care. However, the establishment of the National Clinical Programme for Diabetes in 2011 led to the development of a Model of Integrated Care for people with type 2 diabetes (Health Service Executive of Ireland [HSE], 2018). The appointment of the community-based Clinical Nurse Specialist Diabetes Integrated Care (CNSp) role is seen to be fundamental to the success of this new model of diabetes care.
The Model of Integrated Care defines where people with diabetes should be cared for according to the complexity of their condition. Those with uncomplicated type 2 diabetes are managed in primary care, and those with complicated type 2 diabetes are managed between primary and secondary care. People with type 1 diabetes are managed in secondary care only.
The Clinical Nurse Specialist Diabetes Integrated Care
The creation of the CNSp post has greatly improved the integrative function of the nursing role between primary and secondary care (HSE, 2018). In addition to delivering specialist nursing care, the CNSp provides support to primary and secondary care. CNSps review patients referred to them by the GP or practice nurse, and they also provide training and support in the setting-up and delivery of integrated diabetes care clinics.
The CNSps also deliver structured patient education as well as educational programmes for healthcare professionals. They carry out research and audit, and use audit data to improve integrated care at the practice level. The CNSps spend approximately 80% of their working time in primary care and 20% in secondary care, which enables them to support the integration of care.
The CNSp service is funded by the HSE to general practice. The HSE estimates that there are 2932 GPs in Ireland. At present, the CNSp service accesses only 990 GPs (34%) nationally. There are a variety of reasons why this is so, including the service being at capacity in some areas.
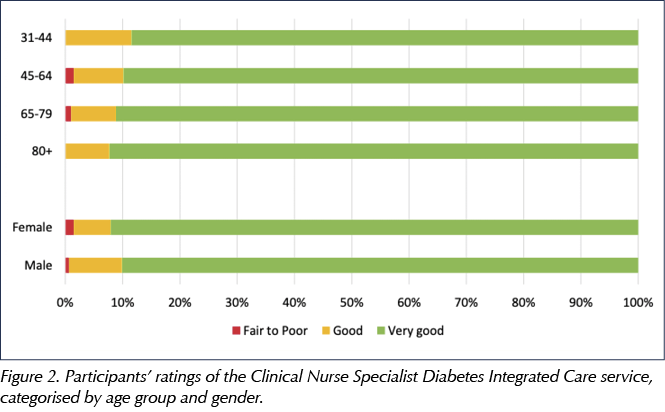
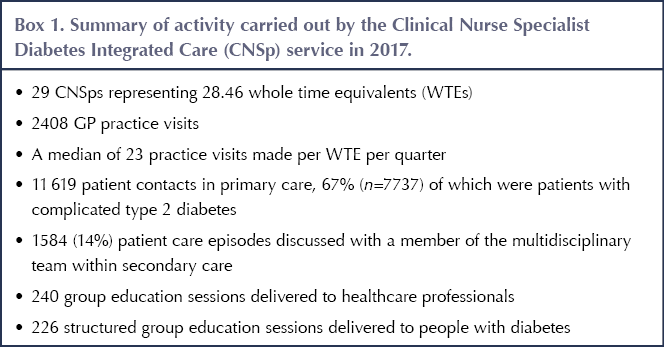
A report on CNSp data in 2017 highlighted the work carried out over a 12-month period (Box 1).
Patient experience
Improving the quality of care is a goal of health systems worldwide, and patient experience can be used as an indicator of healthcare quality (Guler, 2017). Patient experience is distinct from patient satisfaction in that the former asks for information on what happens to someone when they use a service, rather than whether they were satisfied with the service. The first National Patient Experience Survey was conducted in 2017 (HSE, 2017).
Models of integrated care have been found to impact favourably on patient satisfaction. Nine UK studies of integrated care across different services involving diabetes reported high levels of satisfaction (Baxter et al, 2018). A further qualitative study explored the views of GPs and practice nurses in their experience of a local CNSp service (Newell and O Donnell, 2018). Few studies have evaluated the perspective of service users (Harkins, 2016) or their experience of nurse-led specialist care.
This article summarises the results of a national project which was undertaken in 2018 to measure patients’ experience of the CNSp service in Ireland (Riordan et al, 2018).
Methods
Ethical approval
Ethical approval to conduct the study was obtained from the Clinical Research Ethics Committee of the Cork Teaching Hospitals Group.
Questionnaire
The survey was developed by the National Diabetes Integrated Care Nursing Group in conjunction with the Evidence to Support Prevention Implementation and Translation Research Group at University College Cork. The questions used were modified from the National Patient Experience Survey, which originated from a library developed by the Picker Institute.
Five CNSps piloted the questionnaire with ten patients to ensure clarity and understanding. Each CNSp distributed questionnaires to two consecutive patients. As some participants included their own names, the questionnaire was subsequently revised to emphasise anonymity. The questionnaire contained seventeen closed questions and three open-ended questions about the CNSp service. The final open-ended questions were designed to allow participants to express their experience of the CNSp consultation in their own words.
Questions included aspects of care relating to the consultation with the CNSp, such as notice given of appointment, privacy during consultation, whether foot assessment was performed and nurse–patient communication. Participants were asked to rate their overall experience on a scale of one to ten. They were invited to comment on positive aspects of the consultation, areas that may be improved and any general feedback with the use of three open-ended questions. The full questionnaire is available in Appendix 1.
Participants and sampling
Participants were recruited across the nine Community Healthcare Organisations. Eligible participants were people with diabetes who had attended the CNSp service and who had the mental and physical capacity to complete the questionnaire. Those responsible for distributing the questionnaire at the general practice assessed eligibility.
Consecutive eligible patients were invited to participate in this research between June and August 2018 until there were ten participants per CNSp. Participants were invited following their consultation with the CNSp to complete the questionnaire. The majority of the questionnaires were distributed by receptionists or practice nurses; others were distributed by the CNSp in general practices where it was not feasible for the receptionist or practice nurse to do so. After completing the questionnaires, participants placed them in a sealed box.
Results
In total, 33 CNSps of the 34 (32.46 whole time equivalents) currently employed in Ireland recruited participants. One CNSp declined to participate, having already completed a patient satisfaction survey. A variety of distribution methods was employed. Seventeen CNSps (52%) had receptionists distribute questionnaires, three (9%) had practice nurses distribute questionnaires, four (12%) distributed the questionnaire themselves and nine (27%) used a combination of all three approaches. A total of 404 questionnaires were distributed.
In total, 318 participants (79%) returned questionnaires, and 315 completed them either fully or partially. Only 233 of the questionnaires (58% of those distributed) were completed fully. The characteristics of the sample population are detailed in Table 1.
Key findings of the survey
- Patient consultations with the CNSp typically lasted 30–45 minutes.
- 99% (n=302) of participants felt the prior notice of their appointment was satisfactory.
- 92% (n=285) of participants reported their feet were checked during the consultation.
- 98% (n=306) of participants felt that the CNSp explained their condition in a clear and concise manner and answered their questions in a way they could understand.
- 98% (n=306) of participants had enough time to discuss blood results and treatment plans with the CNSp.
- 97% (n=304) of participants were involved as much as they wanted to be in decisions about their care and treatment.
- 94% (n=295) of participants received enough information to manage their diabetes.
- 99% (n=302) of participants rated their overall experience between good and very good.
Overall experience
Participants were asked to rate their experience with the CNSp service on a scale from one to ten, with ten being the best and one being the worst. Overall, 91% (n=277) of participants rated their experience as very good (overall rating between nine and ten), and 8% (n=25) as good (between seven and eight; Figure 1). A small proportion (n=3) rated the service as fair to poor (overall rating between zero and six). Experience was similar across different age groups and between men and women (Figure 2).
 |
 |
Discussion
This survey evaluated patients’ experiences of CNSp services across Ireland. The participants reported a positive experience, reflecting favourably on different aspects of the consultation. This includes aspects such as length of consultation, notice time, patient–nurse communication, understanding, and involvement in their care and care planning. When asked what they found good about their consultation, people commented on the value of the service in terms of improving their understanding and management of their condition.
Strengths and limitations
This is the first survey in Ireland to evaluate patients’ experience of the CNSp service in primary care. The findings show patients have an overall positive experience of the CNSp service. However, participants’ objectivity must be considered when analysing their responses.
Selection bias could be present in this study as patients volunteered to complete the questionnaire. Furthermore, the sample size was small when compared with the number of people the nurses see in primary and secondary care (Box 1).
In practices where no receptionist or practice nurse was available, surveys were distributed by the CNSp. Where there were literacy or language issues, assistance to complete the questionnaire may have been given. This may have impacted participants’ objectivity when responding and created social desirability bias, whereby they may have answered questions in a manner that will be viewed favourably by the CNSp.
Study implications
- CNSps largely manage people with complex type 2 diabetes.
- The CNSp service improves service users’ understanding and management of their condition.
- CNSps have dedicated discussions with patients about their condition. The majority, 94%, are very positive about relevant information received. This highlights the ability of CNSps to make complex information accessible to people with diabetes.
- The survey highlights that the CNSp service empowers people to better self-manage their diabetes, which, over the long term, should reduce inpatient admissions and diabetes complications.
- In addition, participants stated that CNSps carry out foot examinations. Foot examinations should be performed annually in primary care (HSE, 2011), but often they are not, and they are less frequently performed by GPs than by specialists (SIGN, 2010).
Further recommendations
This survey demonstrates that patients value the CNSp service positively. However, further evaluation of the service is required. This work was limited to the patients’ perspectives. Future research should consider exploring the perceptions of primary healthcare professionals who access the CNSp service, such as GPs and practice nurses. It would also be useful to compare findings with practices that do not have access to a CNSp.
Conclusion
Despite its limitations, this survey was innovative in Ireland by assessing patients’ experience of the CNSp service for the first time. The participants’ evaluation of the service was excellent and there was evidence that the service contributes significantly to the promotion of self-management of a chronic condition. With additional support, the service could expand to be accessible to all.
Acknowledgements
The authors wish to acknowledge Fiona Riordan, Ciara Lynch and Patricia Kearney, authors of the original patient experience report (Riordan et al, 2018).
Fiona Riordan is a Postdoctoral Researcher in the School of Public Health (SPH), University College Cork. She conducted data analysis and led preparation of the report.
Ciara Lynch was responsible for data entry, cleaning and analysis, and contributed to drafting the report. She conducted this work as part of a Health Research Board Summer Student Scholarship based in the SPH, under the supervision of Fiona Riordan and Patricia Kearney.
Patricia Kearney is a Professor of Epidemiology in the SPH. She advised on the analysis, read drafts of the report and approved the final version.






Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024